Abstract
Azaspirane (N-N-diethyl-8,8-dipropyl-2-azaspiro [4.5] decane-2-propanamine; trade name, Atiprimod) is an orally bioavailable cationic amphiphilic compound that significantly inhibits production of interleukin 6 (IL-6) and inflammation in rat arthritis and autoimmune animal models. We here characterize the effect of atiprimod on human multiple myeloma (MM) cells. Azaspirane significantly inhibited growth and induced caspase-mediated apoptosis in drug-sensitive and drug-resistant MM cell lines, as well as patient MM cells. IL-6, insulin-like growth factor 1 (IGF-1), or adherence of MM cells to bone marrow stromal cells (BMSCs) did not protect against atiprimod-induced apoptosis. Both conventional (dexamethasone, doxorubicin, melphalan) and novel (arsenic trioxide) agents augment apoptosis induced by atiprimod. Azaspirane inhibits signal transducer activator of transcription 3 (STAT3) and a PI3-K (phosphatidylinositol 3-kinase) target (Akt), but not extracellular signal-regulated kinase 1 and 2 (ERK1/2), inhibits phosphorylation triggered by IL-6, and also inhibits inhibitorκBα (IκBα) and nuclear factor κB (NFκB) p65 phosphorylation triggered by tumor necrosis factor α (TNF-α). Of importance, azaspirane inhibits both IL-6 and vascular endothelial growth factor (VEGF) secretion in BMSCs triggered by MM cell binding and also inhibits angiogenesis on human umbilical vein cells (HUVECs). Finally, azaspirane demonstrates in vivo antitumor activity against human MM cell growth in severe combined immunodeficient (SCID) mice. These results, therefore, show that azaspirane both induces MM cell apoptosis and inhibits cytokine secretion in the BM milieu, providing the framework for clinical trials to improve patient outcome in MM.
Introduction
Despite treatment with alkylating agents, anthracyclines, and corticosteroids,1,2 as well as high-dose therapy and stem cell transplantation,3-5 multiple myeloma (MM) remains incurable due to both intrinsic and acquired drug resistance.6-10 Furthermore, the bone marrow (BM) microenvironment also confers drug resistance in MM cells via at least 2 different mechanisms: adhesion of MM cells to fibronectin confers cell adhesion–mediated drug resistance (CAM-DR), associated with induction of p27Kip1 and G1 growth arrest,11,12 and cytokines (ie, interleukin 6 [IL-6] and insulin-like growth factor 1 [IGF-1]) in the BM milieu induce Janus kinase 2 (JAK2)/signal transducers and activators of transcription 3 (STAT3), phosphatidylinositol 3-kinase (PI3-K)/a PI3-K target (Akt) signaling, or both, which mediates resistance to conventional therapies.13-15 Importantly, novel biologically based treatments that target not only the MM cell but also MM cell–host interactions and cytokines in the BM microenvironment can overcome drug resistance in both preclinical and early clinical studies.16-19
Azaspirane (N-N-diethyl-8,8-dipropyl-2-azaspiro [4.5] decane-2-propanamine; trade name, Atiprimod) is an orally bioavailable cationic amphiphilic compound, which has been extensively studied in a variety of animal models of autoimmune disease and transplantation.20-22 For example, it significantly inhibits inflammation and protects against joint erosion in animal models of arthritis.23-26
In this report, we demonstrate that azaspirane induces potent cytotoxicity, at least in part, by inhibiting IL-6. Its favorable cytotoxicity profile, combined with the major role of IL-6 as an MM growth, survival, and drug-resistance factor, provided the framework for its preclinical evaluation against MM cells. It triggers apoptosis via activation of caspase-8 and caspase-3, followed by poly(ADP [adenosine diphosphate]–ribose) polymerase (PARP) cleavage. As with proteasome inhibitor PS-34127-29 and immunomodulatory derivatives of thalidomide (IMiDs),30 azaspirane-induced MM cell growth inhibition is augmented by dexamethasone (Dex). Although IL-6 and IGF-1 are major MM cell growth factors and confer protection against Dex-induced apoptosis,14,27,31-33 neither exogenous IL-6 nor IGF-1 protect against azaspirane-induced cytotoxicity. Moreover, adherence of MM cells to bone marrow stromal cells (BMSCs) both augments tumor cell growth and protects against drug-induced apoptosis34 ; importantly, azaspirane induces apoptosis even of MM cells adherent to BMSCs. Vascular endothelial growth factor (VEGF) both directly stimulates MM cell proliferation and migration35,36 and induces angiogenesis in the BM milieu.37,38 Azaspirane inhibits VEGF secretion from BMSCs and human umbilical vein endothelial cells (HUVECs), as well as angiogenesis. Finally, azaspirane shows activity against human MM cells in a xenograft severe combined immunodeficient (SCID) mouse model. Our studies, therefore, demonstrate that azaspirane can overcome conventional drug resistance in preclinical models by targeting both MM cells and the BM milieu, providing the frameworks for its clinical evaluation to improve patient outcome in MM.
Patients, materials, and methods
Reagents
Azaspirane was provided by Callisto Pharmaceuticals (New York, NY). IL-6 and IGF-1 were purchased from R&D Systems (Minneapolis, MN). Pan caspase inhibitor Z-Val-Ala-DL-Asp-fluoromethylketone (Z-VAD-FMK; Calbiochem, San Diego, CA) was dissolved in dimethyl sulfoxide (DMSO), stored at -20°C, and used at 25 μM. Doxorubicin (Dox) and arsenic trioxide (As2O3) were used as in our prior studies.39
MM-derived cell lines and patient MM cells
Dex-sensitive (MM.1S) and -resistant (MM.1R) human MM cell lines were kindly provided by Dr Steven Rosen (Northwestern University, Chicago, IL). RPMI8226 and U266 human MM cells were obtained from American Type Culture Collection (Rockville, MD). Dox-resistant (RPMI-Dox40) and melphalan (Mel)–resistant (RPMI-LR5) cells were kindly provided by Dr William Dalton (Lee Moffitt Cancer Center, Tampa, FL). OPM1 cells were kindly provided by Dr Edward Thompson (University of Texas Medical Branch, Galveston, TX). IL-6–dependent human plasma cell line INA-6 was derived from a tumor of INA-6 cells grown in the peritoneum of severe combined immunodeficient mice.40 HUVECs were purchased from Clonetics Biowhittaker (Walkersville, MD). MM cell lines were cultured in RPMI-1640 containing 10% fetal bovine serum (Sigma Chemical, St Louis, MO), 2 μM l-glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin (GIBCO, Grand Island, NY). INA-6 cells were cultured in medium that additionally contained 1 ng/mL IL-6. HUVECs were cultured in endothelial cell growth media (EGM-2 MV; Cambrex Bio Science, Walkersville, MD). Patient plasma cells were purified from patient BM aspirates as described previously.29,41 Approval for these studies was obtained from the Dana-Farber Cancer Institute Institutional Review Board. Informed consent was obtained from all patients in accordance with Declaration of Helsinki protocol.
BMSC cultures
BM specimens were obtained from patients with MM, and mononuclear cells separated by Ficoll-Hypaque density sedimentation were used to establish long-term BM cultures, as previously described.34 When an adherent cell monolayer had developed, cells were harvested in phosphate-buffered saline (PBS) solution containing 0.25% trypsin and 0.02% EDTA (ethylenediaminetetraacetic acid), washed, and collected by centrifugation.
Growth inhibition assay
The inhibitory effect of azaspirane on growth of MM cell lines, peripheral blood mononuclear cells (PBMCs), and BMSCs was assessed by measuring 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrasodium bromide (MTT; Chemicon International, Temecula, CA) dye absorbance, as previously described.29 Cells from 48-hour cultures with azaspirane were pulsed with 10 μL of 5 mg/mL MTT to each well for the last 4 hours of 48-hour cultures, followed by 100 μL isopropanol containing 0.04N HCl. Absorbance was measured at 570 nm, using a spectrophotometer (Molecular Devices, Sunnyvale CA). All experiments were performed in quadruplicate.
Assays of apoptosis
Azaspirane-induced apoptosis was confirmed by the transferase-mediated dUTP (deoxyuridine triphosphate) nick end labeling (TUNEL) method, using fragmentation of genomic DNA detected by MEBSTAIN Apoptosis Kit Direct (Medical & Biological Laboratories, Nagoya, Japan) and followed by analysis by Coulter Epics XL flow cytometry (Beckman Coulter, Fullerton, CA). Briefly, MM.1S and U266 cells were cultured for 48 and 72 hours in control media (0.01% DMSO) or 5 μM azaspirane at 37°C, washed, and fixed with 4% paraformaldehyde in PBS (pH 7.4). After washing, cells were permeabilized in 70% ethanol, DNA nick ends were labeled with terminal deoxynucleotidyl transferase (TdT) solution, and analysis was performed using Coulter Epics XL flow cytometry.
Immunoblotting
MM cells were cultured with azaspirane in the presence or absence of caspase inhibitors, harvested, washed, and lysed using lysis buffer: 50 mM Tris (tris(hydroxymethyl)aminomethane)–HCl (pH 7.4), 150 mM NaCl, 1% NP-40 ([Octylphenoxy]polyethoxyethanol), 10 mM sodium pyrophosphate, 5 mM EDTA, 1 mM EGTA (ethylene glycol tetraacetic acid), 2 mM Na3VO4, 5 mM NaF, 1 mM PMSF (phenylmethlsulfonyl fluoride), 5 μg/mL leupeptin, and 5 μg/mL aprotinin, as described previously.41 Cell lysates were subjected to sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE), transferred to phenylmethlsulfonyl fluoride (PVDF) membrane (Bio-Rad Laboratories, Hercules, CA), and immunoblotted with anti–PARP, caspase-8, caspase-3, caspase-9, Bcl-2 (B-cell lymphoma leukemia 2)–associated X protein (BAX), Bcl-xL, myeloid cell leukemia-1 (Mcl-1), nuclear factor κB (NFκB) phospho-p65, phospho–inhibitorκBα (IκBα) (Cell Signaling, Beverly, MA), phospho-JAK2 (Bio Source, Camarillo, CA), phospho–extracellular signal-regulated kinase (ERK), phospho-STAT3, JAK2, ERK1, STAT3, NFκB p65, IκBα, and α-tubulin (Santa Cruz Biotech, Santa Cruz, CA) antibodies (Abs).
Caspase-3 activation after azaspirane treatment
Caspase-3 activation was detected by using a Caspase-3/CPP32 Colorimetric Assay Kit (Medical & Biological Laboratories). After azaspirane (5 μM) treatment, MM.1S cells were harvested and lysed with lysis buffer. Protein concentration in cell lysates was diluted 50 to 200 μg and incubated with DEVD–p-nitroanilide (DEVD-pNA) substrate at 37°C for 2 hours in 96-well culture plates (Costar, Cambridge, MA). Samples were read at 405 nm using a spectrophotometer (Molecular Devices, Sunnyvale, CA).
Effect of azaspirane on paracrine MM cell growth in the BM
To evaluate the effect of drug on growth of MM cells (3 × 104 cells/well) adherent to BMSCs, MM.1S and U266 cells were cultured in BMSC-coated 96-well plates (Costar) for 48 hours in the presence or absence of media, azaspirane, Dex, Mel, Dox, and As2O3. DNA synthesis was measured by [3H]-thymidine (Perkin Elmer, Boston, MA) uptake, with [3H]-thymidine (0.5 μCi/well [0.0185 MBq]) added during the last 8 hours of 48-hour cultures.41 IL-6 and VEGF levels in supernatants were detected by DuoSet ELISA (enzyme-linked immunosorbent assay) Development kit (R&D Systems), and absorbance was measured at 450 nm and 540 nm using a spectrophotometer (Molecular Devices). All experiments were performed in quadruplicate.
Angiogenesis assay
The effect of azaspirane on angiogenesis was detected by In Vitro Angiogenesis Assay Kit (Chemicon International). ECMatrix (50 μL) was transferred into 96-well plates and incubated at 37°C for 12 hours. HUVECs (1 × 104 cells/well) were seeded in each well with or without 1.25 and 2.5 μM azaspirane and incubated for 6 hours at 37°C. Cellular network structures were visualized by inverted Olympus CK2 (Olympus, Tokyo, Japan) microscopy, photographed with an F440 digital camera (Fujifilm, Tokyo, Japan) and processed with Adobe Photoshop 7.0 (Adobe, San Jose, CA).
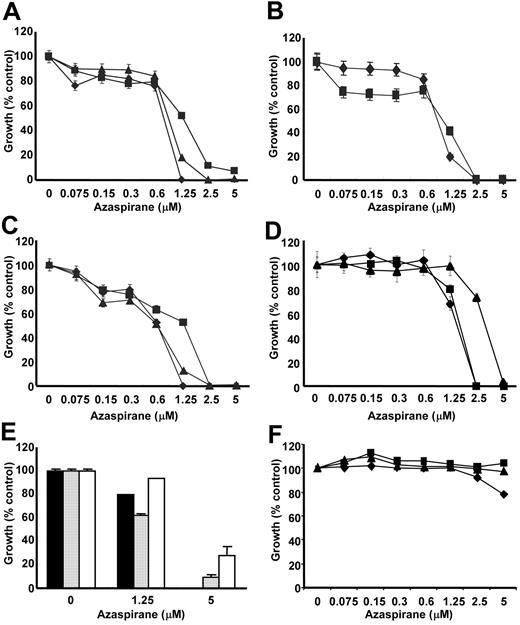
Azaspirane induces growth inhibition in MM cell lines and patient MM cells. (A) MM.1S (♦), U266 (▪), and RPMI8226 (▴) MM cells; (B) Dex-sensitive MM.1S (♦) and Dex-resistant MM.1R (▪) MM cells; (C) drug-sensitive RPMI8226 (♦), melphalan-resistant RPMI-LR5 (▪), and doxorubicin-resistant RPMI-Dox40 (▴) cells; (D) OPM1 (▴), INA-6 (▪), and MM.1S (♦) cells; (E) freshly isolated tumor cells from patients with MM (n = 3; ▪,  , □), as well as (F) peripheral blood mononuclear cells from healthy volunteers (n = 3; ▪, ▴, ♦) were cultured for 48 hours in the presence of azaspirane (0-5 μM). Cell growth was assessed by MTT assay, and data represent mean (± SD) of quadruplicate cultures.
, □), as well as (F) peripheral blood mononuclear cells from healthy volunteers (n = 3; ▪, ▴, ♦) were cultured for 48 hours in the presence of azaspirane (0-5 μM). Cell growth was assessed by MTT assay, and data represent mean (± SD) of quadruplicate cultures.
Azaspirane induces growth inhibition in MM cell lines and patient MM cells. (A) MM.1S (♦), U266 (▪), and RPMI8226 (▴) MM cells; (B) Dex-sensitive MM.1S (♦) and Dex-resistant MM.1R (▪) MM cells; (C) drug-sensitive RPMI8226 (♦), melphalan-resistant RPMI-LR5 (▪), and doxorubicin-resistant RPMI-Dox40 (▴) cells; (D) OPM1 (▴), INA-6 (▪), and MM.1S (♦) cells; (E) freshly isolated tumor cells from patients with MM (n = 3; ▪,  , □), as well as (F) peripheral blood mononuclear cells from healthy volunteers (n = 3; ▪, ▴, ♦) were cultured for 48 hours in the presence of azaspirane (0-5 μM). Cell growth was assessed by MTT assay, and data represent mean (± SD) of quadruplicate cultures.
, □), as well as (F) peripheral blood mononuclear cells from healthy volunteers (n = 3; ▪, ▴, ♦) were cultured for 48 hours in the presence of azaspirane (0-5 μM). Cell growth was assessed by MTT assay, and data represent mean (± SD) of quadruplicate cultures.
In vivo activity of azaspirane
Six- to 8-week-old male CB-17 SCID mice (Taconic, Germantown, NY) were housed and monitored in our animal research facility. All experimental procedures and protocols had been approved by the Institutional Animal Care and Use Committee. In a human MM xenograft murine model,42 mice were subcutaneously inoculated in the interscapular area with 5 × 106 OPM1 cells in 100 μL RPMI-1640 medium. Mice were then treated intravenously with either vehicle alone (PBS) or azaspirane (50 mg/kg per day) for 6 days. Treatment was initiated after the detection of palpable tumors, approximately 3 weeks following injection of MM cells. Tumor size was measured weekly in 2 dimensions using a caliper, and volume was calculated using the formula: V = 0.5a × b2, where a and b are the long and short diameter of tumor, respectively.
Statistical analysis
Statistical significance of differences observed in drug-treated versus control cultures was determined using the Wilcoxon signed rank test. The minimal level of significance was P less than .05.
Results
Azaspirane induces growth inhibition of MM cell lines
We first determined the effect of treatment with azaspirane (0-5 μM) for 48 hours on growth of MM cell lines (MM.1S, U266, and RPMI8226), freshly isolated patient MM cells, and PBMCs using MTT assay. Azaspirane demonstrated significant cytotoxicity (> 95% growth inhibition, P < .001), with IC50 (inhibitory concentration 50%) of 0.5 to 1.25 μM in MM.1S, U266, and RPMI8226 MM cell lines (Figure 1A). Azaspirane also triggered cytotoxicity in Dex-resistant MM.1R cells (Figure 1B), as well as Dox-resistant RPMI-Dox40 and Mel-resistant RPMI-LR5 MM cells (Figure 1C). These results demonstrate that azaspirane induces cytotoxicity even in MM cell lines resistant to conventional chemotherapy. Azaspirane also demonstrated significant cytotoxicity against INA-6 cell lines and OPM1 MM cells (Figure 1D). Importantly, azaspirane also induced cytotoxicity in freshly isolated tumor cells from patients with MM (Figure 1E); however, it did not trigger cytotoxicity in PBMCs from 3 healthy volunteers (Figure 1F). These data demonstrate that azaspirane specifically induces cytotoxicity in MM cells but not in normal cells.
Apoptosis triggered by azaspirane is mediated via caspase-8/-3 and PARP cleavage
To confirm drug-related cytotoxicity and to determine its mechanisms of action, we next performed TUNEL assay in MM.1S and U266 cells treated with azaspirane (5 μM). As can be seen in Figure 2A, azaspirane induced DNA fragmentation in both MM.1S and U266 cells in a time-dependent fashion, confirming that azaspirane-triggered cytotoxicity is induced via apoptosis. To further analyze the mechanism of azaspirane-induced apoptosis in MM cells, we next assessed activation of caspases in MM cell lines cultured with either media or azaspirane. Caspase-3 activation was induced in MM.1S cells after 4 hours and 8 hours of treatment with azaspirane, assessed by colorimetric assay (Figure 2B). Immunoblotting showed that azaspirane triggered caspase-8 cleavage, followed by typical PARP cleavage (95 kDa), but did not induce caspase-9 cleavage (Figure 2C). Conversely, the pan-caspase inhibitor Z-VAD-FMK blocked azaspirane-induced PARP cleavage in MM.1S cells (Figure 2D). These results indicate that cytotoxicity triggered by azaspirane, like other novel agents,29,39,43 is mediated via caspase-8/-3/PARP cleavage and apoptosis.
Azaspirane induces caspase-dependent apoptotic cell death. (A) MM.1S and U266 cells were cultured with azaspirane (5 μM) for 48 and 72 hours. Azaspirane-induced apoptosis was confirmed by the TUNEL method, using flow cytometry. Percentage demonstrated is TUNEL-negative fraction gated by horizontal bars. (B) MM.1S cells were cultured with azaspirane (5 μM) for 4 and 8 hours. Whole-cell lysates were subjected to caspase-3 colorimetric assay. The absorbance was measured at 405 nm, using a spectrophotometer, and data represent mean (± SD) of triplicate cultures. (C) MM.1S cells were cultured with azaspirane (5 μM) for 4, 8, and 12 hours. Whole-cell lysates were subjected to Western blotting, using anti–caspase-8, anti–caspase-3, PARP Abs, as well as anti–caspase-9, BAX, Bcl-2, and Mcl-1 Abs. (D) MM.1S cells were preincubated with Z-VAD-FMK (20 μM) for 1 hour prior to treatment with azaspirane (5 μM) for 4, 8, and 12 hours. Whole-cell lysates were subjected to Western blotting using anti-PARP Ab.
Azaspirane induces caspase-dependent apoptotic cell death. (A) MM.1S and U266 cells were cultured with azaspirane (5 μM) for 48 and 72 hours. Azaspirane-induced apoptosis was confirmed by the TUNEL method, using flow cytometry. Percentage demonstrated is TUNEL-negative fraction gated by horizontal bars. (B) MM.1S cells were cultured with azaspirane (5 μM) for 4 and 8 hours. Whole-cell lysates were subjected to caspase-3 colorimetric assay. The absorbance was measured at 405 nm, using a spectrophotometer, and data represent mean (± SD) of triplicate cultures. (C) MM.1S cells were cultured with azaspirane (5 μM) for 4, 8, and 12 hours. Whole-cell lysates were subjected to Western blotting, using anti–caspase-8, anti–caspase-3, PARP Abs, as well as anti–caspase-9, BAX, Bcl-2, and Mcl-1 Abs. (D) MM.1S cells were preincubated with Z-VAD-FMK (20 μM) for 1 hour prior to treatment with azaspirane (5 μM) for 4, 8, and 12 hours. Whole-cell lysates were subjected to Western blotting using anti-PARP Ab.
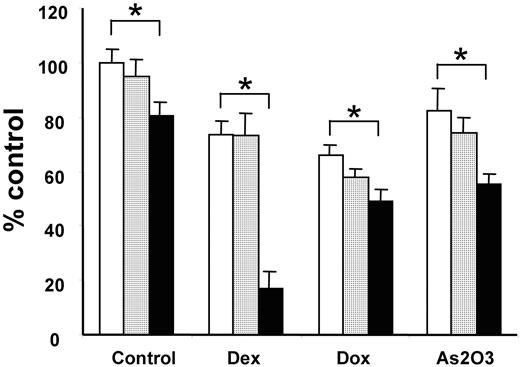
Azaspirane augments growth inhibition in MM cells triggered by conventional and novel chemotherapeutic agents
Since we have shown that conventional agents may augment cytotoxicity of novel chemotherapeutic agents,27,30,34,41,44 we next similarly examined whether conventional (Dex, Dox) or novel (As2O3) chemotherapeutic agents could enhance the growth inhibitory effect of azaspirane. MM.1S cells were cultured with Dex (0.5 μM), Dox (0.5 μM), or As2O3 (1 μM) in media or with azaspirane (0.6 and 1.25 μM) for 24 hours. Dex, Dox, As2O3, and azaspirane induced 10% to 25% growth inhibition when used alone; however, these agents enhanced MM.1S cell death triggered by azaspirane (Figure 3). Specifically, 1.25 μM azaspirane or 0.5 μM Dex alone triggered 20% and 22% cytotoxicity, respectively; however, combining azaspirane with Dex triggered 82% cytotoxicity.
Azaspirane overcomes the antiapoptotic effect of IL-6 and IGF-1
Since we and others have shown that IL-631,32,45 and IGF-146-48 mediate both growth and antiapoptosis in MM cells, we next examined whether azaspirane could overcome these effects of exogenous IL-6 and IGF-1. Although IL-6 (25 ng/mL) and IGF-1 (50 ng/mL) triggered a 1.3-fold (Figure 4A) and a 1.7-fold (Figure 4B) increase in MM.1S cell growth in cultures relative to media alone, neither IL-6 nor IGF-1 protected against azaspirane-induced MM.1S cell death.
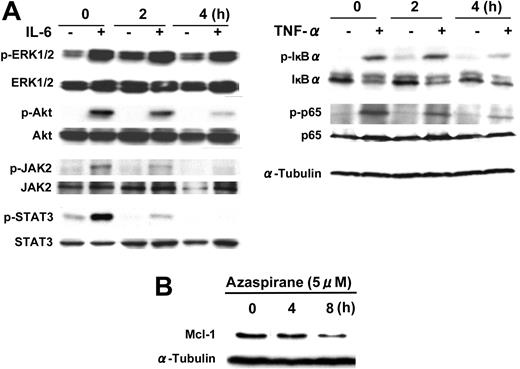
Azaspirane inhibits phosphorylation of JAK2/STAT3, IκBα, and p65 NFκB and down-regulates Mcl-1 expression
Since we15,28,45,49 and others50,51 have shown that ERK, JAK2/STAT3, and Akt signaling cascades mediate proliferation, survival, and drug resistance in MM cells, we next examined whether azaspirane could block these signaling pathways (Figure 5A). Phosphorylation of ERK1/2, Akt, and JAK2/STAT3 was induced by IL-6 (25 ng/mL) in MM.1S cells; however, pretreatment with azaspirane (5 μM for 1 and 2 hours) abrogated IL-6–induced JAK2, STAT3, and Akt phosphorylation. Interestingly, phosphorylation of ERK induced by IL-6 was not similarly altered by azaspirane. Since JAK2/STAT3 pathway regulates expression of Mcl-1, which plays a crucial role in MM cell survival and antiapoptosis,51-54 we next examined whether azaspirane could inhibit Mcl-1 expression. As can be seen in Figure 5B, azaspirane down-regulates Mcl-1 expression in MM.1S cells. Moreover, azaspirane also inhibited IκBα and NFκB p65 phosphorylation induced by TNF-α in MM.1S cells (Figure 5A). This result suggests that azaspirane blocks IκBα phosphorylation and translocation of NFκB from cytoplasm to nucleus, thereby overcoming the antiapoptotic activity of NFκB.
Azaspirane enhances the growth inhibitory effect of conventional chemotherapeutic agents. MM.1S cells were cultured with control media (□) and with 0.6 μM (▦) or 1.25 μM (▪) azaspirane in the absence or presence of Dex (0.5 μM), Dox (0.5 μM), and As2O3 (1 μM) for 24 hours. Cell growth was assessed by MTT assay, and data represent mean (± SD) of quadruplicate cultures. *P < .01.
Azaspirane enhances the growth inhibitory effect of conventional chemotherapeutic agents. MM.1S cells were cultured with control media (□) and with 0.6 μM (▦) or 1.25 μM (▪) azaspirane in the absence or presence of Dex (0.5 μM), Dox (0.5 μM), and As2O3 (1 μM) for 24 hours. Cell growth was assessed by MTT assay, and data represent mean (± SD) of quadruplicate cultures. *P < .01.
IL-6 and IGF-1 do not protect against azaspirane-induced apoptosis. MM.1S cells were cultured with azaspirane (0-8 μM) for 48 hours in the presence (▪) or absence (♦) of IL-6 (25 ng/mL) (A) or IGF-1 (50 ng/mL) (B). Cell growth was assessed by [3H]-thymidine uptake, and data represent mean (± SD) of quadruplicate cultures.
IL-6 and IGF-1 do not protect against azaspirane-induced apoptosis. MM.1S cells were cultured with azaspirane (0-8 μM) for 48 hours in the presence (▪) or absence (♦) of IL-6 (25 ng/mL) (A) or IGF-1 (50 ng/mL) (B). Cell growth was assessed by [3H]-thymidine uptake, and data represent mean (± SD) of quadruplicate cultures.
Azaspirane inhibits MM cell growth, as well as cytokine secretion, triggered by tumor cell binding to BMSCs
Since we have shown that the BM microenvironment confers growth and drug resistance in MM cells,16,19 we next studied the effect of azaspirane on paracrine MM cell growth in the BM milieu. We first examined the direct toxicity of azaspirane on patient BMSCs using MTT assay, as in our previous studies27,41 ; no significant growth inhibition in BMSCs was triggered by azaspirane treatment (data not shown). MM.1S and U266 MM cells were next cultured with or without BMSCs, in the presence or absence of azaspirane. Tumor cell adherence to BMSCs triggered increased [3H]-thymidine uptake in MM.1S cells (1.72-fold, P < .01; Figure 6A) and U266 cells (2.2-fold, P < .01; data not shown); azaspirane inhibited this up-regulation of DNA synthesis in a dose-dependent fashion. Since adherence of MM cells to BMSCs also triggers increased secretion of IL-6 and VEGF in culture supernatants,34,41,55 we further examined whether azaspirane could inhibit cytokine secretion in cultures of MM cells adherent to BMSCs. Azaspirane inhibited not only IL-6 (Figure 6B) but also VEGF (Figure 6C) secretion in cultures of BMSCs, both alone and with adherent MM.1S cells.
Azaspirane inhibits phosphorylation of JAK2/STAT3 and Akt but not ERK1/2. MM.1S cells were pretreated with azaspirane (5 μM) for 2 hours and 4 hours. Cells were then stimulated with IL-6 (20 ng/mL) or TNF-α (10 ng/mL) for 10 minutes. Whole-cell lysates were subjected to Western blotting using anti–phospho-ERK/ERK, phospho-Akt/Akt, phospho-STAT3/STAT3, phospho-JAK2, phospho-IκBα/IκBα, phospho-NFκB p65/NFκB p65, and α-tubulin Abs (A); MM.1S cells were treated with azaspirane (5 μM) for 4 hours and 8 hours. Whole-cell lysates were subjected to Western blotting, using anti–Mcl-1 and α-tubulin Abs (B).
Azaspirane inhibits phosphorylation of JAK2/STAT3 and Akt but not ERK1/2. MM.1S cells were pretreated with azaspirane (5 μM) for 2 hours and 4 hours. Cells were then stimulated with IL-6 (20 ng/mL) or TNF-α (10 ng/mL) for 10 minutes. Whole-cell lysates were subjected to Western blotting using anti–phospho-ERK/ERK, phospho-Akt/Akt, phospho-STAT3/STAT3, phospho-JAK2, phospho-IκBα/IκBα, phospho-NFκB p65/NFκB p65, and α-tubulin Abs (A); MM.1S cells were treated with azaspirane (5 μM) for 4 hours and 8 hours. Whole-cell lysates were subjected to Western blotting, using anti–Mcl-1 and α-tubulin Abs (B).
Azaspirane inhibits MM cell growth, as well as IL-6 and VEGF secretion, triggered by tumor cell binding to BMSCs. MM.1S cells, BMSCs, or both MM.1S cells and BMSCs were cultured for 48 hours in the presence of DMSO control (□) or with 0.6 μM(▦), 1.25 μM(▨), and 2.5 μM(▪) azaspirane (A). DNA synthesis was assessed by [3H]-thymidine uptake, and data represent mean (± SD) of quadruplicate cultures. IL-6 (B) and VEGF (C) levels in culture supernatants were measured by ELISA. *P < .01.
Azaspirane inhibits MM cell growth, as well as IL-6 and VEGF secretion, triggered by tumor cell binding to BMSCs. MM.1S cells, BMSCs, or both MM.1S cells and BMSCs were cultured for 48 hours in the presence of DMSO control (□) or with 0.6 μM(▦), 1.25 μM(▨), and 2.5 μM(▪) azaspirane (A). DNA synthesis was assessed by [3H]-thymidine uptake, and data represent mean (± SD) of quadruplicate cultures. IL-6 (B) and VEGF (C) levels in culture supernatants were measured by ELISA. *P < .01.
Azaspirane inhibits generation of capillary vessels on HUVECs
Since VEGF plays an important role in MM cell growth and migration, as well as stimulating angiogenesis in the BM microenvironment,38,56,57 inhibition of VEGF secretion by azaspirane might both inhibit angiogenesis and have anti-MM activity in the BM milieu. We, therefore, first examined the direct effect of azaspirane on generation of capillary vessels of HUVECs. Azaspirane clearly inhibited development of cellular network structures for 6 hours (Figure 7A), but was not directly cytotoxic in HUVECs, assessed by MTT assay (Figure 7B). In HUVECs, as well as in BMSCs, azaspirane similarly inhibited secretion of VEGF (Figure 7C).
Azaspirane inhibits human MM cell growth in a SCID mouse model
We next studied the effect of azaspirane treatment in SCID mice injected with OPM1 human MM cells as in prior studies.42 Mice were treated with either azaspirane (50 mg/kg per day; n = 5) or control PBS (n = 4) for 6 days beginning when tumors become palpable. As seen in Figure 8, treatment with azaspirane induced a significant reduction in tumor growth in vivo.
Discussion
Although MM is incurable with conventional and high-dose therapies, novel biologically based treatment strategies targeting both MM cells and the BM microenvironment offer great promise to improve patient outcome since they overcome drug resistance in both preclinical and clinical studies.16,58 In this report, we demonstrate that azaspirane (N-N-diethyl-8,8-dipropyl-2-azaspiro [4.5] decane-2-propanamine), a novel class of agents, induces apoptosis in drug-resistant MM cell lines and patient tumor cells with an IC50 of 0.6 to 1 μM and 1.25 to 5 μM, respectively. Importantly, we observed no cytotoxicity in PBMCs at drug concentrations of 0.08 to 5 μM, suggesting potential selective cytotoxicity against tumor cells and a therapeutic index for use of these inhibitors in vivo. To determine whether azaspirane enhances cytotoxicity of conventional therapies or novel agents, we examined the effect of Dex, Dox, and As2O3 together with azaspirane on proliferation of MM.1S cells. Among these agents, Dex synergizes with azaspirane-induced cytotoxicity, suggesting differential apoptotic signaling cascades for azaspirane versus Dex. For example, Dex induces caspase-9 activation via a cytochrome-c–independent, second mitochondria-derived activator of caspases (Smac)–dependent, pathway,59 whereas our study shows caspase-8 activation by azaspirane. These results are similar to our prior report that low concentrations of PS-341 sensitize MM cell lines and patient cells to DNA-damaging chemotherapeutic agents, such as Dox and Mel.44 Our ongoing studies will delineate the mechanisms of synergy of DNA-damaging agents with azaspirane to provide a rational framework for clinical use of this agent in combination with conventional chemotherapy.
Azaspirane inhibits generation of capillary vessels on HUVECs. HUVECs were cultured in 96-well plates with ECMatrix with or without azaspirane (Aza; 1.25 and 2.5 μM) (magnification, × 40) (A). Cytotoxicity of azaspirane (0-5μM) against HUVECs was determined at 24 hours by MTT assay (B), and VEGF levels in culture supernatants were measured by ELISA (C), and data represent mean (± SD) of quadruplicate cultures. *P < .01.
Azaspirane inhibits generation of capillary vessels on HUVECs. HUVECs were cultured in 96-well plates with ECMatrix with or without azaspirane (Aza; 1.25 and 2.5 μM) (magnification, × 40) (A). Cytotoxicity of azaspirane (0-5μM) against HUVECs was determined at 24 hours by MTT assay (B), and VEGF levels in culture supernatants were measured by ELISA (C), and data represent mean (± SD) of quadruplicate cultures. *P < .01.
IL-6 triggers proliferation of MM cells via activation of the Ras/Raf/MAPK (mitogen-activated protein kinase)/p42/44 MAPK signaling cascade,45,49 and survival of MM cells via JAK2/STAT3 activation with downstream induction of Bcl-xL50 and Mcl-1.51,54,60,61 IGF-1 also promotes MM cell proliferation and survival via Ras/Raf/MAPK/p42/44 MAPK and PI3-K/Akt signaling cascades.15,28 Specifically, IL-6 protects against Dex-induced apoptosis via PI3-K/Akt signaling.14,15,62 We, therefore, next examined whether exogenous IL-6 and IGF-1 inhibited azaspirane-induced cytotoxicity in MM cells. Importantly, neither IL-6 nor IGF-1 protect against azaspirane-induced cytotoxicity, suggesting that azaspirane, in contrast to conventional therapies, can overcome the protective effects of these cytokines in the BM milieu.
Azaspirane inhibits in vivo human MM cell growth in a SCID mouse model. CB-17 SCID mice were inoculated subcutaneously in the interscapular area with 5 × 106 OPM1 MM cells. Three weeks later with detection of palpable tumors, mice were treated intravenously with azaspirane (50 mg/kg per day) or vehicle control (PBS) for 6 days. Tumor volume was calculated as described in “Materials and methods.” Figure demonstrates significant tumor regression at 3 to 6 days following treatment. Error bars represent ± SD of tumor volume.
Azaspirane inhibits in vivo human MM cell growth in a SCID mouse model. CB-17 SCID mice were inoculated subcutaneously in the interscapular area with 5 × 106 OPM1 MM cells. Three weeks later with detection of palpable tumors, mice were treated intravenously with azaspirane (50 mg/kg per day) or vehicle control (PBS) for 6 days. Tumor volume was calculated as described in “Materials and methods.” Figure demonstrates significant tumor regression at 3 to 6 days following treatment. Error bars represent ± SD of tumor volume.
We have previously demonstrated that apoptosis triggered by conventional and novel anti-MM agents is mediated via caspase-8 or caspase-9 activation, or both, followed by caspase-3 and PARP cleavage.16,63 In this study, azaspirane induced caspase-8 and caspase-3 activation, followed by PARP cleavage, in a time-dependent fashion; conversely, drug-induced PARP cleavage was blocked by Z-VAD-FMK, confirming azaspirane induced caspase-dependent apoptosis. Azaspirane mediates caspase-8 activation, suggesting potential clinical utility of combining this agent with Dex or PS-341, which trigger caspase-9 activation, to induce dual apoptotic signaling, or with lenalidomide (Revlimid), which also triggers caspase-8 activation to enhance cytotoxicity.
Since azaspirane abrogated the effect of IL-6 and IGF-1 on the growth of MM.1S cells, we next examined which signaling cascades triggered by IL-6 were inhibited by this novel agent. IL-6 triggers p42/44 MAPK, STAT3, and PI3-K/Akt pathways mediating growth, survival, and drug resistance in MM cells.16,18,19 We demonstrated that azaspirane markedly inhibited IL-6–triggered JAK2/STAT3 and Akt phosphorylation. Since STAT3 can regulate antiapoptotic proteins Bcl-XL and Mcl-1,51,54,60 we further examined whether azaspirane could down-regulate these proteins, due to inactivation of STAT3. We demonstrate that baseline expression of Mcl-1 was down-regulated by azaspirane treatment. NFκB is present in the cytoplasm and inactivated by association with IκB30; conversely, NFκB is activated by TNF-α stimulation and translocates to the nucleus. In MM, NFκB confers drug resistance in tumor cells, modulates the expression of adhesion molecules on MM cells and BMSCs, and regulates cytokine transcription and secretion in BMSCs.41,64,65 Importantly, our study shows that azaspirane blocked phosphorylation of IκBα and p65 NFκB induced by TNF-α. Our ongoing studies are delineating downstream target molecules of STAT3 and NFκB inhibition, which may further augment the apoptotic effect of azaspirane.
Given that neither IL-6 nor IGF protect against azaspirane-induced cytotoxicity, we next examined whether azaspirane can overcome MM cell growth, survival, migration, and drug resistance in the BM microenvironment.16,18,19 We demonstrated that azaspirane inhibits growth of MM.1S and U266 cells adherent to BMSCs, without cytotoxicity on BMSCs. Furthermore, binding of MM cells to BMSCs up-regulates secretion of both IL-6 and VEGF, which further promote MM cell growth, survival, and drug resistance in the BM milieu. Importantly, azaspirane also blocked secretion of these cytokines in BMSCs triggered by MM cell binding.
There is growing evidence of a critical role for angiogenesis in pathogenesis of hematologic malignancies, including MM.56 Conversely, thalidomide and other novel agents impair angiogenesis by decreasing fibroblast growth factor 2 (FGF-2) and VEGF production.57 In MM, VEGF is expressed and secreted by tumor cells as well as BMSCs and induces growth, survival, and migration of MM cells.35,36 We have previously reported that novel agents55,66,67 and
Having shown the ability of azaspirane to overcome drug resistance in vitro, we then assessed its activity against human MM cells in a SCID mouse model. Azaspirane inhibits tumor growth in the MM xenograft model, using human OPM1 MM cell lines in SCID mice. This result suggests that azaspirane can similarly target human MM cells in the BM microenvironment in vivo.
In summary, azaspirane can inhibit MM cell growth, survival, and drug resistance within the BM milieu both in vitro and in vivo. Our results, therefore, provide the preclinical framework for clinical trials of this agent to improve patient outcome in MM.
Prepublished online as Blood First Edition Paper, February 10, 2005; DOI 10.1182/blood-2004-09-3794.
Supported by National Institutes of Health Specialized Program of Research Excellence (SPORE) IP50 grants (CA10070-01, PO-1 78378, and RO-1 CA50947), the Doris Duke Distinguished Clinical Research Scientist Award (K.C.A.), the Multiple Myeloma Research Foundation (T.H. and D.C.), and the Cure for Myeloma Research Fund (K.C.A.).
Two of the authors (D.H.P. and G.S.J.) are employees of Callisto Pharmaceuticals Inc, whose compound Atiprimod was studied in the present work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


![Figure 4. IL-6 and IGF-1 do not protect against azaspirane-induced apoptosis. MM.1S cells were cultured with azaspirane (0-8 μM) for 48 hours in the presence (▪) or absence (♦) of IL-6 (25 ng/mL) (A) or IGF-1 (50 ng/mL) (B). Cell growth was assessed by [3H]-thymidine uptake, and data represent mean (± SD) of quadruplicate cultures.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/105/11/10.1182_blood-2004-09-3794/6/m_zh80110578950004.jpeg?Expires=1767839051&Signature=4w~kLwHPpulvc9zy7KekkdSmFYIX0DTnKFKbJxfNhuD9ei7P5T8c2urFzii9lpT-sC8V3RWN0GZk-hZ6jvCFPEnhDmJNIG3NBvAMzllhv-y969io~YEbsOjbBEynPzA1-uha9xjNmN2rxYhxkzbJ3PMbUf1CMLQmQlfTZGakR2namcilNvFG7h9EtoYsa7m7chh59FmLDkxPDiZzdBE8mvH5eA~znrgSImrsCSfz6fMdj~6cuOib5eHocKNuSTMtrcs8jlwbS03q9bpOyIkSZfRSD-XLsl~zSK~RqRm4oH3sr7Wnk3axsGsfTsIbTipw5h~7869kKoEY0a6I6-7F5Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. Azaspirane inhibits MM cell growth, as well as IL-6 and VEGF secretion, triggered by tumor cell binding to BMSCs. MM.1S cells, BMSCs, or both MM.1S cells and BMSCs were cultured for 48 hours in the presence of DMSO control (□) or with 0.6 μM(▦), 1.25 μM(▨), and 2.5 μM(▪) azaspirane (A). DNA synthesis was assessed by [3H]-thymidine uptake, and data represent mean (± SD) of quadruplicate cultures. IL-6 (B) and VEGF (C) levels in culture supernatants were measured by ELISA. *P < .01.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/105/11/10.1182_blood-2004-09-3794/6/m_zh80110578950006.jpeg?Expires=1767839051&Signature=fwyOt2~6qT3wWbjQzXIDY0wh35yOk-la5UKu9-Z~9t4AeDysAdUJyF6uCwfAHbRUf6iwFxScSj4K5ve7LLtv2fHYBZr87B-l2kxN9VBL7MWTN5rlxKE67lFgBsOU4McktZZ-S2UvH3eC33raEafJjeusVlXkUPNESViTNGB0u6Gq2puJE53fsCYvO8Gz2AX~0gDirNgV2Uebq3Br~M5x9IGMZTqeOZVSaQWH7zWaAhb4-xVSl5olYB6hWMeTVQxXNyY3iUFiwQqPyv656G2qyk3c7aKzaiin3ef5nH65~zmy9jETDWJ-QrfFlnLUby0RSSy1A1zgRcqaqO58zTOFPw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal