AKT serine threonine kinase of the protein kinase B (PKB) family plays essential roles in cell survival, growth, metabolism, and differentiation. In the erythroid system, AKT is known to be rapidly phosphorylated and activated in response to erythropoietin (Epo) engagement of Epo receptor (EpoR) and to sustain survival signals in cultured erythroid cells. Here we demonstrate that activated AKT complements EpoR signaling and supports erythroid-cell differentiation in wild-type and JAK2-deficient fetal liver cells. We show that erythroid maturation of AKT-transduced cells is not solely dependent on AKT-induced cell survival or proliferation signals, suggesting that AKT transduces also a differentiation-specific signal downstream of EpoR in erythroid cells. Down-regulation of expression of AKT kinase by RNA interference, or AKT activity by expression of dominant negative forms, inhibits significantly fetal liver–derived erythroid-cell colony formation and gene expression, demonstrating that AKT is required for Epo regulation of erythroid-cell maturation.
Introduction
Protein kinase B (PKB) or AKT is phosphorylated and activated in response to the erythropoietin (Epo) engagement of its receptor, downstream of the PI3 kinase. In addition to the regulation of survival, AKT is involved in many fundamental biologic processes, including the regulation of cell cycle, differentiation, and intermediary metabolism, and is often activated in human cancers.1-3 Activation of the PI3 kinase signaling pathway,4-12 alone in the absence of other signaling pathways, may be required and sufficient, under certain conditions, to sustain erythroid-cell development.4,13,14 In addition, the PI3 kinase signaling pathway, and AKT specifically, are associated with the pathogenesis of polycythemia vera in which they may play a role.15-17
Here the potential role of AKT kinase in Epo-induced maturation of primary fetal liver erythroid progenitor cells using an in vitro system we previously established14 was investigated.
Study design
Cells, flow cytometry, and erythroid colony assay
Retroviral transduction
TER 119- wild-type (E14) and JAK2-/- (E12.5) fetal liver cells (2 × 105/mL) were resuspended in viral supernatants and plated on 60 mm RetroNectin– (chimeric fibronectin peptide; Takara Biomedicals, Osaka, Japan) coated dishes as previously described14,19 in the presence of 100 ng/mL each of interleukin-6 (IL-6) and Steel factor (SF) (PeproTech, Rocky Hill, NJ). GFP-positive cells were FACS sorted the next day and cultured under the same conditions with or without Epo (2 U/mL) for another 24 hours.
RNA interference
Duplices of oligonucleotides were cloned into BglII/HindIII sites of MSCV-U3-H1 plasmid and subcloned subsequently into NotI/ScaI sites of pMSCV-puromycin-IRES-EGFP-U3-H1 plasmid (provided by B.L.).
Real-time PCR analysis
Real-time polymerase chain reaction (PCR) was performed in duplicates on LightCycler 2.0 (Roche, Indianapolis, IN) using SYBR Green Taq Ready-Mix (Sigma, St Louis, MO) (as described by Ghaffari et al20 ). Gene-specific primers were designed to span intron-exon boundary by Primer Express 2.0 (ABI; Applied Biosystems, Foster City, CA). Relative quantification of gene expression between multiple samples was achieved by normalization against 2 of endogenous Hprt, β-actin, and/or Rpl32 using the LightCycler Relative Quantification Software (Roche).
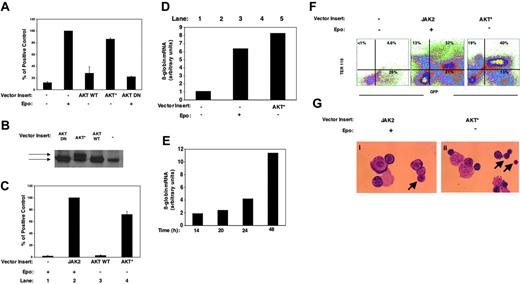
AKT complements EpoR signaling in inducing erythroid differentiation in wild-type and JAK2-/- fetal liver progenitor cells. TER 119- E14 wild-type (A) or JAK2-/- (C) fetal liver cells were transduced with a bicistronic retroviral vector (MIG) or MIG containing the indicated inserts and cultured in the presence or absence of Epo (2 U/mL) on RetroNectin. Thirty-six hours later, live GFP-positive cells from wild-type–(A) or JAK2-/--transduced cells (C) were assayed for CFU-E–generated colony content as determined by diaminobenzidine staining of hemoglobin. Graphs are from duplicates of 4 (A) and 3 (C) independent experiments. The average of the absolute number of CFU-E–derived colonies formed from vector control–transduced cells in the presence of Epo was 3160 ± 64 (n = 4) per 105 wild-type TER 119- cells and 1248 ± 263 per 105 JAK2-transduced JAK2-/-- (n = 3) plated cells. (B) Western blot analysis of transduced NIH 3T3 cells with 1:10 dilution of the retroviral supernatant. The upper band in the activated AKT*-transduced cells corresponds to the Flag-tagged myristylated AKT. (D) Real-time PCR analysis of the β-globin gene in live GFP-positive cells from panel A. Representative graph from duplicate analysis of 2 independent experiments. (E) Real-time PCR analysis of kinetics of up-regulation of β-globin gene expression in TER 119- E14 wild-type fetal liver–derived cells transduced with MIG-AKT* (results expressed as relative to time zero are from total cells). (F) JAK2-/- fetal liver–transduced cells with MIG, MIG-JAK2, or with a constitutively active AKT (MIG-AKT*) and cultured in the presence of Epo (MIG-JAK2 cells) or in the absence of Epo (vector control and MIG-AKT* cells) were analyzed for erythroid-cell differentiation 36 hours later (note TER 119+ cells within transduced GFP-positive cells). (G) Representative field of Wright-Giemsa staining of live GFP-positive transduced JAK2-/--derived cells (magnification, × 1000). Arrows show (i) polychromatophilic erythroblast and (ii) polychromatophilic erythroblast and normoblast. Images were obtained using a Nikon Eclipse E600 microscope (Nikon, Garden City, NJ) and a 100 ×/0.3 numeric aperture oil immersion lens. Images were captured using an RT Slider SPOT 2.3.1 camera and SPOT Advanced software (both from Diagnostic Instruments, Sterling Heights, MI).
AKT complements EpoR signaling in inducing erythroid differentiation in wild-type and JAK2-/- fetal liver progenitor cells. TER 119- E14 wild-type (A) or JAK2-/- (C) fetal liver cells were transduced with a bicistronic retroviral vector (MIG) or MIG containing the indicated inserts and cultured in the presence or absence of Epo (2 U/mL) on RetroNectin. Thirty-six hours later, live GFP-positive cells from wild-type–(A) or JAK2-/--transduced cells (C) were assayed for CFU-E–generated colony content as determined by diaminobenzidine staining of hemoglobin. Graphs are from duplicates of 4 (A) and 3 (C) independent experiments. The average of the absolute number of CFU-E–derived colonies formed from vector control–transduced cells in the presence of Epo was 3160 ± 64 (n = 4) per 105 wild-type TER 119- cells and 1248 ± 263 per 105 JAK2-transduced JAK2-/-- (n = 3) plated cells. (B) Western blot analysis of transduced NIH 3T3 cells with 1:10 dilution of the retroviral supernatant. The upper band in the activated AKT*-transduced cells corresponds to the Flag-tagged myristylated AKT. (D) Real-time PCR analysis of the β-globin gene in live GFP-positive cells from panel A. Representative graph from duplicate analysis of 2 independent experiments. (E) Real-time PCR analysis of kinetics of up-regulation of β-globin gene expression in TER 119- E14 wild-type fetal liver–derived cells transduced with MIG-AKT* (results expressed as relative to time zero are from total cells). (F) JAK2-/- fetal liver–transduced cells with MIG, MIG-JAK2, or with a constitutively active AKT (MIG-AKT*) and cultured in the presence of Epo (MIG-JAK2 cells) or in the absence of Epo (vector control and MIG-AKT* cells) were analyzed for erythroid-cell differentiation 36 hours later (note TER 119+ cells within transduced GFP-positive cells). (G) Representative field of Wright-Giemsa staining of live GFP-positive transduced JAK2-/--derived cells (magnification, × 1000). Arrows show (i) polychromatophilic erythroblast and (ii) polychromatophilic erythroblast and normoblast. Images were obtained using a Nikon Eclipse E600 microscope (Nikon, Garden City, NJ) and a 100 ×/0.3 numeric aperture oil immersion lens. Images were captured using an RT Slider SPOT 2.3.1 camera and SPOT Advanced software (both from Diagnostic Instruments, Sterling Heights, MI).
Results and discussion
Activated AKT complements Epo receptor (EpoR)/JAK2 signaling and supports differentiation of wild-type and JAK2-deficient fetal liver erythroid progenitor cells
JAK2-deficient and TER 119- wild-type fetal liver cells are deprived of mature erythroid cells. As expected, erythroid maturation of CFU-E progenitors contained in TER 119- wild-type (Figure 1A) and JAK2-/- fetal liver cells (Figure 1C), as determined by diaminobenzidine staining of hemoglobin, required Epo and a functional JAK2 tyrosine kinase. Interestingly, overexpression of a constitutively active form of AKT (AKT*; Flag-tagged myristylated AKT) (Figure 1A,C, lane 4) but not wild-type AKT (Figure 1A,C, lane 3) overrides the need for Epo and JAK2. Activation and not merely overexpression of AKT is thus required for induction of erythroid differentiation of fetal liver progenitor cells. The size of the clusters and the degree of hemoglobinization was comparable between AKT*- and control-transduced cells of either JAK2-/- or wild-type origin. Overexpression of a dominant negative (DN) form of AKT in erythroid progenitors resulted in a significant decrease in the number of mature CFU-E–derived colonies in the presence of Epo (Figure 1A, lane 5) without a major effect on the total cell numbers, suggesting that the inhibitory effect of AKT DN is not due to apoptosis. Equal viral titers used in these experiments generated routinely similar levels of expression of AKT wild-type and mutants in heterologous cells (Figure 1B). Activated AKT and Epo induced similar levels of expression of β-globin in differentiating wild-type progenitor cells (Figure 1D). Expression of the β-globin gene was up-regulated by 2-fold after 14 hours and increased with time in activated AKT-transduced progenitor cells in culture (Figure 1E). The degree of maturation of JAK2-/- fetal liver cells transduced with either an active AKT in the absence of Epo or with JAK2 in the presence of Epo was comparable as judged by the up-regulation of TER 119 (glycophorin A),18 a marker of post–CFU-E erythroid cells (Figure 1F), and by their morphology and Wright Giemsa staining (Figure 1G). These results demonstrate that AKT supports Epo-mediated erythroid-cell maturation without the need for any additional signaling protein that requires JAK2 for its activation.
AKT induces a signal required for differentiation of erythroid progenitor cells
To further determine the stage of erythroid differentiation, the expression of TER 119 and CD71 (transferrin receptor) in transduced cells was analyzed. In the absence of Epo, expression of activated AKT (Figure 2A, bottom right panel, and Figure 2B, lane 3), in contrast to wild-type AKT (Figure 2A, bottom left panel, and Figure 2B, lane 2), induced maturation of erythroid cells to the CD71-/low TER 119+ stage of differentiation. Overexpression of active AKT* had some mild inhibitory effect in the later stages of fetal liver cell maturation (Figure 2A; compare top and bottom right panels), although the effect did not seem to be statistically significant in the limit of the number of experiments performed (Figure 2B; compare populations of CD71- TER 119+ in lanes 3 and 4).
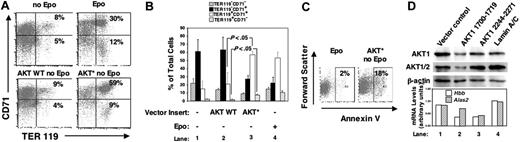
AKT induces full postprogenitor erythroid differentiation through a signal distinct from its survival signal. (A) FACS analysis of TER 119 and CD71 cell-surface expression within live GFP-positive wild-type TER 119- (E14) fetal liver progenitor-derived cells after 36 hours of retroviral transduction with indicated constructs and cultured in the presence or absence of Epo on RetroNectin. Percentages for CD71+ TER 119+ (top right quadrant) and for CD71-/low TER 119+ (bottom right quadrant) are shown. Representative plot from 5 independent experiments is shown. (B) Relative content of different erythroid subpopulations of the same experiments as in panel A. The P values (Student t test) are calculated from differences in CD71+ TER 119+ and CD71- TER 119+ cells between active (AKT*) or wild-type AKT-transduced cells. (C) Percentages of annexin V–positive cells in a fraction of live GFP-positive transduced cells from panel A; a representative of 3 independent experiments is shown. (D) Primary fetal liver progenitor (TER 119-) cells were retrovirally transduced with retroviral vectors expressing shRNA targeting the following sequences: (AKT1 1700-1719) 5′AACAGTTCTCCTACTCAGCCA3′, (AKT1 2244-2271) 5′GATTCTTGTTCCTCTGTCAACCTCACTT3′ 21 or lamin A/C.22 Supernatants of retroviral vectors with RNA polymerase III H1 promoter driving the expression of shRNA and containing no insert (lane 1), shRNA targeting AKT (lanes 2 and 3),21 or shRNA targeting lamin A/C (lane 4)22 were used. Total cells were cultured in the presence of Epo (2 U/mL), SF (50 ng/mL), and IL-6 (50 ng/mL). Seventy-two hours after retroviral transduction, protein and RNA lysates were prepared from aliquots of the same samples for Western blot analysis (top panel, using indicated antibodies) and real-time PCR analysis (bottom panel). To minimize cell loss during the procedure, GFP-positive cells, in average 50%, were not FACS sorted in these experiments.
AKT induces full postprogenitor erythroid differentiation through a signal distinct from its survival signal. (A) FACS analysis of TER 119 and CD71 cell-surface expression within live GFP-positive wild-type TER 119- (E14) fetal liver progenitor-derived cells after 36 hours of retroviral transduction with indicated constructs and cultured in the presence or absence of Epo on RetroNectin. Percentages for CD71+ TER 119+ (top right quadrant) and for CD71-/low TER 119+ (bottom right quadrant) are shown. Representative plot from 5 independent experiments is shown. (B) Relative content of different erythroid subpopulations of the same experiments as in panel A. The P values (Student t test) are calculated from differences in CD71+ TER 119+ and CD71- TER 119+ cells between active (AKT*) or wild-type AKT-transduced cells. (C) Percentages of annexin V–positive cells in a fraction of live GFP-positive transduced cells from panel A; a representative of 3 independent experiments is shown. (D) Primary fetal liver progenitor (TER 119-) cells were retrovirally transduced with retroviral vectors expressing shRNA targeting the following sequences: (AKT1 1700-1719) 5′AACAGTTCTCCTACTCAGCCA3′, (AKT1 2244-2271) 5′GATTCTTGTTCCTCTGTCAACCTCACTT3′ 21 or lamin A/C.22 Supernatants of retroviral vectors with RNA polymerase III H1 promoter driving the expression of shRNA and containing no insert (lane 1), shRNA targeting AKT (lanes 2 and 3),21 or shRNA targeting lamin A/C (lane 4)22 were used. Total cells were cultured in the presence of Epo (2 U/mL), SF (50 ng/mL), and IL-6 (50 ng/mL). Seventy-two hours after retroviral transduction, protein and RNA lysates were prepared from aliquots of the same samples for Western blot analysis (top panel, using indicated antibodies) and real-time PCR analysis (bottom panel). To minimize cell loss during the procedure, GFP-positive cells, in average 50%, were not FACS sorted in these experiments.
We next investigated whether expression of activated AKT resulted in a survival advantage that facilitated erythroid-cell maturation. To our surprise, the survival rate of activated AKT-transduced cells (in the absence of Epo) was significantly lower (Figure 2C, right plot) than that of control cells cultured in Epo (Figure 2C, left plot) as measured by annexin V (an early measure of apoptosis) binding. These results suggest that AKT may not substitute for the apoptosis-suppressing function of the Epo-STAT5-Bcl-XL pathway.
The enhanced erythroid maturation of AKT*-transduced cells was not accompanied by an increase in total cell number. AKT*-transduced TER 119- WT fetal liver cells cultured in the absence of Epo were found less in the S phase (S, 38.5%; G0-G1, 46.8%) as compared with cells cultured in Epo (S, 47.5%; G0-G1, 42%), suggesting that AKT induction of erythroid differentiation was not only due to its enhancement of cell-cycle progression. Thus, the ability of activated AKT to induce fetal liver erythroid-cell differentiation does not solely stem from its potential to promote cell survival or proliferation.
AKT involvement was further evaluated by using RNA interference to inhibit the expression of AKT during Epo-induced differentiation of primary fetal liver cells. Retrovirally transduced fetal liver progenitor-derived cells expressing short hairpin RNA (shRNA) targeting AKT1 and AKT2 exhibited a significant decrease in the expression of red cell–specific genes β-globin and Alas2 (Figure 2D, lane 2) as compared with controls. Inhibition of expression of AKT also induced a significant suppression of the number but not the size of CFU-E–derived colonies consistent with an inhibition of erythroid differentiation of fetal liver cells (data not shown). The presence of inhibitors of caspase 3, a general inhibitor of apoptosis in cultured fetal liver cells, did not affect these results. Collectively, these results further confirmed that the effect of AKT on erythropoiesis is not limited to its regulation of apoptosis.
The combined data from both JAK2-/- and wild-type fetal liver cells demonstrate that AKT mediates a signal downstream of EpoR,23 distinct from its survival signal, that supports differentiation of fetal liver erythroid progenitor cells. These data are consistent with an in vivo role for AKT in normal24 and in polycythemia vera15-17 hematopoiesis.
Prepublished online as Blood First Edition Paper, October 27, 2005; DOI 10.1182/blood-2005-06-2304.
Supported by a National Cancer Institute Clinician Scientist Career Award NIH5K08 (CA77675) (S.G.), a National Institutes of Health (NIH) grant (NIH/NHLBI P01 HL32262) (H.F.L.), and the Mount Sinai School of Medicine Foundation (S.G.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr Zhou Songyang (Baylor College of Medicine) for AKT constructs,25 Dr Klaus Pfeffer (Technical University of Munich, Germany) for JAK2+/- mice, and Glenn Paradis (Massachusetts Institute of Technology [MIT], Cancer Center) for flow cytometry. We are grateful to Drs Gordon Keller, Bill Schiemann, and Nai-Wen Chi for critical reviews of the manuscript.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal