Abstract
The prognostic relevance of FLT3 D835/I836 mutations (FLT3-TKD) in cytogenetically normal acute myeloid leukemia (CN-AML) remains to be established. After excluding patients with FLT3 internal tandem duplications, we compared treatment outcome of 16 de novo CN-AML patients with FLT3-TKD with that of 123 patients with wild-type FLT3 (FLT3-WT), less than 60 years of age and similarly treated on Cancer and Leukemia Group B protocols. All FLT3-TKD+ patients and 85% of FLT3-WT patients achieved a complete remission (P = .13). Disease-free survival (DFS) of FLT3-TKD+ patients was worse than DFS of FLT3-WT patients (P = .01; estimated 3-year DFS rates, 31% vs 60%, respectively). In a multivariable analysis, FLT3-TKD was associated with worse DFS (P = .02) independent of NPM1 status and percentage of bone marrow blasts. To gain further biologic insights, a gene-expression signature differentiating FLT3-TKD+ from FLT3-WT patients was identified. The signature (333 probe sets) included overexpression of VNN1, C3AR1, PTPN6, and multiple other genes involved in monocarboxylate transport activity, and underexpression of genes involved in signal transduction regulation. These associations with outcome, other prognostic markers, and the elucidated expression signature enhance our understanding of FLT3-TKD–associated biology and may lead to development of novel therapies that improve clinical outcome of CN-AML patients with FLT3-TKD.
Introduction
The fms-related tyrosine kinase 3 gene (FLT3) encodes a protein member of the type III platelet-derived growth factor family of receptor tyrosine kinases that play an important role in normal hematopoiesis (reviewed recently by Parcells et al1 ). The 2 most frequent FLT3 mutations associated with adult cytogenetically normal acute myeloid leukemia (CN-AML) are internal tandem duplications (FLT3-ITD) of the juxtamembrane region, present in approximately 30% of CN-AML patients, and nucleotide substitutions, deletions, or insertions involving the D835/I836 residues of the second tyrosine kinase domain (hereafter abbreviated FLT3-TKD), present in approximately 7% of CN-AML patients (reviewed by Mrózek et al2 ). The D835Y substitution constitutes approximately 50% of FLT3-TKD mutations. Less frequent FLT3-TKD mutations involving other amino acid residues include the Y842C,3 K663Q,4 and V592A5 and those occurring in the juxtamembrane domain.6 The proteins coded by the FLT3-ITD and FLT3-TKD mutations exhibit ligand–independent FLT3 dimerization and constitutive activation through autophosphorylation. Although both FLT3-ITD and FLT3-TKD mutations are transforming in in vitro models, several lines of evidence indicate that these 2 types of mutations influence downstream signal transduction pathways differently.7-9
Although the adverse clinical impact of the presence of FLT3-ITD in adults less than the age of 60 years with CN-AML is well established,2,10-16 the prognostic significance of FLT3-TKD remains to be elucidated.13,17-19 Here, we assessed the prognostic impact of FLT3-TKD, specifically D835/I836 mutations, in younger adults with de novo CN-AML lacking FLT3-ITD and treated on similar Cancer and Leukemia Group B (CALGB) frontline treatment protocols for AML (9621 and 19808). We show that the presence of FLT3-TKD is associated with worse disease-free survival (DFS) relative to similar patients with wild-type FLT3 alleles (FLT3-WT). We also report the first Affymetrix microarray-derived gene-expression signature differentiating FLT3-TKD+ from FLT3-WT CN-AML, which includes genes with potential biologic and therapeutic relevance.
Methods
Patients
Pretreatment bone marrow (BM) or blood samples were obtained from adult patients with de novo CN-AML, younger than 60 years and treated on similar protocols either CALGB 962120 or CALGB 19808.21 All patients gave The Ohio State University Institutional Review Board informed consent in accordance with the Declaration of Helsinki for the procurement and research use of their samples. CALGB 9621 evaluated variable doses of daunorubicin and etoposide in combination with fixed doses of cytarabine (100 mg/m2) without (ADE) or with (ADEP) PSC-833, a multidrug resistance protein inhibitor, also called valspodar.20 Based on the results of CALGB 9621, patients were treated on CALGB 19808 with fixed doses of daunorubicin (90 mg/m2) and etoposide (100 mg/m2) in ADE, or daunorubicin (40 mg/m2) and etoposide (40 mg/m2) in ADEP.21 On achievement of complete remission (CR), patients were assigned to intensification with high-dose cytarabine and etoposide for stem cell mobilization followed by myeloablative treatment with busulfan and etoposide supported by autologous peripheral blood stem cell transplantation (APSCT). Patients unable to receive APSCT received 2 additional cycles of high-dose cytarabine. There were no significant differences in CR rates, overall survival (OS), or DFS among patients with CN-AML between these 2 protocols.
Pretreatment cytogenetic analyses of BM were performed by CALGB–approved institutional cytogenetic laboratories as part of CALGB 8461, a prospective cytogenetic companion, and were centrally reviewed, as previously reported.22 To be considered cytogenetically normal, at least 20 BM metaphase cells were analyzed and the karyotype found to be normal in each case.
To detect the presence or absence of FLT3-TKD as previously described,15,23 RNA was extracted from thawed, pretreatment, cryopreserved cells (Trizol Reagent; Invitrogen, Carlsbad, CA) and cDNA prepared using Superscript II and random hexamer primers (Invitrogen). After polymerase chain reaction (PCR), aliquots were subjected to enzymatic digestion with EcoRV and size fractionation through 1.25% agarose gels. Quantification of FLT3-TKD mutant alleles determined as a percentage of total FLT3 alleles was carried out as described previously.24 Additional molecular markers, ie, presence or absence of FLT3-ITD,13,15 MLL partial tandem duplication (MLL-PTD),25,26 and NPM1 mutations,27 as well as BAALC28 and ERG29,30 expression levels, were assessed centrally as previously reported.
Affymetrix gene-expression profiling
RNA was extracted from thawed, pretreatment tissue samples and processed for Affymetrix U133 plus 2.0 GeneChip (Affymetrix, Santa Clara, CA) hybridizations. Briefly, from 8 μg of total RNA, double-stranded cDNA was prepared (Invitrogen) with the use of the T7-Oligo (dT) primer. In vitro transcription was performed with the BioArray High Yield RNA Transcript Labeling Kit (T7) (Enzo Life Science, Farmingdale, NY). Twenty micrograms of fragmented, biotinylated RNA was hybridized to the U133 plus 2.0 GeneChip for 16 hours at 45°C. Scanned images were converted to CEL files using GCOS software (Affymetrix).
Statistical methods
Associations between patients with and without FLT3-TKD and baseline demographic, clinical, and molecular features were described using Fisher exact and Wilcoxon rank-sum tests for categorical and continuous variables, respectively. CR required an absolute neutrophil count more than or equal to 1500/μL, a platelet count more than or equal to 100 000/μL, no leukemic blasts in the blood, BM cellularity more than 20% with maturation of all cell lines, no Auer rods, more than 5% BM blast cells, and no evidence of extramedullary leukemia, with persistence for at least 1 month. Relapse was defined by more than or equal to 5% BM blasts, circulating leukemic blasts or development of extramedullary leukemia.
DFS was measured from the date of CR until date of relapse, censoring for patients alive and relapse-free at last follow-up. OS was measured from the date on study until the date of death, where patients alive at last follow-up were censored. Median follow-up for patients who achieved a CR and were alive and relapse-free was 5.2 years (range, 1.5-8.8 years). Median follow-up for those alive was 4.6 years (range, 1.3-8.9 years). Estimated probabilities of DFS and OS were calculated using the Kaplan-Meier method, and the log-rank test evaluated differences between survival distributions. The proportional hazards model was used to evaluate the impact of FLT3-TKD on DFS using a limited backward selection procedure. Variables considered for the multivariable analysis included age, sex, race, hemoglobin, platelet, and white blood cell (WBC) counts, percentages of blood and BM blasts, extramedullary involvement, MLL-PTD, and NPM1 mutation status. A full model was fit with FLT3-TKD and variables with P less than .20 from univariable models. Variables reporting a P greater than .05 were subsequently dropped, unless they were confounding, defined by changing the estimated coefficient of FLT3-TKD by at least 15%. Because of the small number of FLT3-TKD+ patients with available data on BAALC and ERG expression levels measured by RT-PCR, the impact of FLT3-TKD on outcome in the presence of BAALC, or ERG was not considered in the multivariable model but rather explored separately.
Summary measures of Affymetrix microarray gene expression were computed for each probe set using the robust multichip average method, which incorporates quantile normalization of arrays.31 Expression values were logged (base 2) before analysis. A filtering step was performed to remove probe sets that did not display significant variation in expression across arrays. In this procedure, a χ2 test was used to test whether the observed variance in expression of a probe set was significantly larger than the median observed variance in expression for all probe sets using α = .01 as the significance level. A total of 24 183 probe sets passed the filtering criterion and were included in subsequent analyses. A comparison between gene-expression profiles derived from FLT3-TKD+ (n = 9) and FLT3-WT (n = 50) patient groupings was performed by univariable 2-sample t tests using α = .001 as the significance level, which would result in approximately 24 expected false discoveries of probe sets assuming no gene expression differences between the 2 groups. Analyses were performed using BRB-ArrayTools version 3.4.0 (R. Simon and A.P. Lam, National Cancer Institute, Bethesda, MD) and using the R version 2.3.1 (R Foundation for Statistical Computing, Vienna, Austria). GenMAPP version 2.1 and MAPPFinder version 2.132 were used to assess overrepresented ontologies among the genes comprising the identified signature that were overexpressed in FLT3-TKD+ patients and among those that were underexpressed in FLT3-TKD+ patients. MAPPFinder uses a permutation procedure to determine the overrepresented gene ontologies. All analyses were performed by the CALGB Statistical Center.
Results
Clinical and molecular characteristics at presentation
Among 217 screened CN-AML patients, 16 (7.4%) carried a FLT3-TKD mutation, 75 (34.6%) carried a FLT3-ITD mutation, and 3 (1.4%) harbored both mutations. To assess the impact of FLT3-TKD on clinical outcome, we excluded from further analyses patients with the prognostically unfavorable FLT3-ITD and those with both FLT3-TKD and FLT3-ITD mutations.
At diagnosis, FLT3-TKD+ patients had higher WBC counts, with a median of 57.2 × 109/L compared with 14.6 × 109/L for FLT3-WT patients (P < .001, Table 1). FLT3-TKD+ patients also had higher percentages of blood and BM blasts, with medians of 63% and 76%, respectively, compared with 46% and 63% for FLT3-WT patients (P = .03 and P = .001). For those patients with available quantitative RT-PCR data for BAALC and/or ERG, there was a strong association between FLT3-TKD and BAALC expression (P = .007); 93% of FLT3-TKD+ patients were classified as low BAALC expressers compared with 53% of FLT3-WT patients.
Presenting characteristics, treatment, and outcomes of CN-AML patients with FLT3-WT and those with FLT3-TKD
| Characteristic . | FLT3-WT, n = 123 . | FLT3-TKD, n = 16 . | P . |
|---|---|---|---|
| Age, y | .66 | ||
| Median | 47 | 43 | |
| Range | 19-59 | 19-57 | |
| Sex, no. of males (%) | 61 (50) | 8 (50) | 1.00 |
| Race, no. (%) | 1.00 | ||
| White | 108 (89) | 15 (94) | |
| Nonwhite | 13 (11) | 1 (6) | |
| Hemoglobin, g/L | .33 | ||
| Median | 93 | 89 | |
| Range | 46-134 | 64-124 | |
| Platelet count, ×109/L | .19 | ||
| Median | 66 | 57 | |
| Range | 7-466 | 12-145 | |
| WBC count, ×109/L | <.001 | ||
| Median | 14.6 | 57.2 | |
| Range | 0.9-146.0 | 15.3-295.0 | |
| Blood blasts, % | .03 | ||
| Median | 46 | 63 | |
| Range | 0-97 | 0-90 | |
| Bone marrow blasts, % | .001 | ||
| Median | 63 | 76 | |
| Range | 10-99 | 53-94 | |
| Centrally reviewed FAB, no. (%) | .15 | ||
| M0 | 1 (1) | 1 (9) | |
| M1 | 20 (24) | 3 (27) | |
| M2 | 28 (34) | 2 (18) | |
| M4 | 19 (23) | 1 (9) | |
| M5 | 9 (11) | 4 (36) | |
| M6 | 2 (2) | 0 (0) | |
| AML unclassified | 3 (4) | 0 (0) | |
| Extramedullary involvement, no. (%)* | .39 | ||
| No | 83 (69) | 9 (56) | |
| Yes | 37 (31) | 7 (44) | |
| MLL-PTD, no. (%) | 1.00 | ||
| Negative | 110 (89) | 15 (94) | |
| Positive | 13 (11) | 1 (6) | |
| NPM1, no. (%) | .18 | ||
| Wild-type | 53 (45) | 4 (25) | |
| Mutated | 65 (55) | 12 (75) | |
| BAALC expression, no. (%)† | .007 | ||
| Low | 47 (53) | 13 (93) | |
| High | 41 (47) | 1 (7) | |
| ERG expression, no. (%)‡ | .18 | ||
| Low | 67 (75) | 7 (54) | |
| High | 22 (25) | 6 (46) | |
| Induction treatment, no. (%) | .79 | ||
| ADE | 76 (62) | 9 (56) | |
| ADEP | 47 (38) | 7 (44) | |
| Received APSCT for consolidation treatment, no. (%) | 73 (70) | 12 (75) | .78 |
| Complete remission rate, no. (%) | 105 (85) | 16 (100) | .13 |
| Relapse rate, no. (%) | 45 (43) | 11 (69) | .06 |
| Disease-free survival | .01 | ||
| Median, y | NR | 1.03 | |
| Disease-free at 3 y (95% CI), % | 60 (50-69) | 31 (11-54) | |
| Overall survival | .17 | ||
| Median, y | NR | 2.18 | |
| Alive at 3 y (95% CI), % | 65 (55-73) | 40 (16-64) |
| Characteristic . | FLT3-WT, n = 123 . | FLT3-TKD, n = 16 . | P . |
|---|---|---|---|
| Age, y | .66 | ||
| Median | 47 | 43 | |
| Range | 19-59 | 19-57 | |
| Sex, no. of males (%) | 61 (50) | 8 (50) | 1.00 |
| Race, no. (%) | 1.00 | ||
| White | 108 (89) | 15 (94) | |
| Nonwhite | 13 (11) | 1 (6) | |
| Hemoglobin, g/L | .33 | ||
| Median | 93 | 89 | |
| Range | 46-134 | 64-124 | |
| Platelet count, ×109/L | .19 | ||
| Median | 66 | 57 | |
| Range | 7-466 | 12-145 | |
| WBC count, ×109/L | <.001 | ||
| Median | 14.6 | 57.2 | |
| Range | 0.9-146.0 | 15.3-295.0 | |
| Blood blasts, % | .03 | ||
| Median | 46 | 63 | |
| Range | 0-97 | 0-90 | |
| Bone marrow blasts, % | .001 | ||
| Median | 63 | 76 | |
| Range | 10-99 | 53-94 | |
| Centrally reviewed FAB, no. (%) | .15 | ||
| M0 | 1 (1) | 1 (9) | |
| M1 | 20 (24) | 3 (27) | |
| M2 | 28 (34) | 2 (18) | |
| M4 | 19 (23) | 1 (9) | |
| M5 | 9 (11) | 4 (36) | |
| M6 | 2 (2) | 0 (0) | |
| AML unclassified | 3 (4) | 0 (0) | |
| Extramedullary involvement, no. (%)* | .39 | ||
| No | 83 (69) | 9 (56) | |
| Yes | 37 (31) | 7 (44) | |
| MLL-PTD, no. (%) | 1.00 | ||
| Negative | 110 (89) | 15 (94) | |
| Positive | 13 (11) | 1 (6) | |
| NPM1, no. (%) | .18 | ||
| Wild-type | 53 (45) | 4 (25) | |
| Mutated | 65 (55) | 12 (75) | |
| BAALC expression, no. (%)† | .007 | ||
| Low | 47 (53) | 13 (93) | |
| High | 41 (47) | 1 (7) | |
| ERG expression, no. (%)‡ | .18 | ||
| Low | 67 (75) | 7 (54) | |
| High | 22 (25) | 6 (46) | |
| Induction treatment, no. (%) | .79 | ||
| ADE | 76 (62) | 9 (56) | |
| ADEP | 47 (38) | 7 (44) | |
| Received APSCT for consolidation treatment, no. (%) | 73 (70) | 12 (75) | .78 |
| Complete remission rate, no. (%) | 105 (85) | 16 (100) | .13 |
| Relapse rate, no. (%) | 45 (43) | 11 (69) | .06 |
| Disease-free survival | .01 | ||
| Median, y | NR | 1.03 | |
| Disease-free at 3 y (95% CI), % | 60 (50-69) | 31 (11-54) | |
| Overall survival | .17 | ||
| Median, y | NR | 2.18 | |
| Alive at 3 y (95% CI), % | 65 (55-73) | 40 (16-64) |
FLT3-WT indicates wild-type FLT3; FLT3-TKD, tyrosine kinase domain mutation of the FLT3 gene; WBC, white blood cell; FAB, French-American-British; MLL-PTD, partial tandem duplication of the MLL gene; ADE, cytarabine, daunorubicin, and etoposide; ADEP, cytarabine, daunorubicin, etoposide, and valspodar; APSCT, autologous peripheral blood stem-cell transplantation; CI, confidence interval; and NR, not reached.
Includes involvement of the central nervous system, hepatomegaly, splenomegaly, lymphadenopathy, skin infiltrates, gum hypertrophy, and/or a mediastinal mass.
For patients on protocol 9621, cut point same as in Baldus et al.28 For patients on protocol 19808, median BAALC expression value used for cut point.
For patients on protocol 9621, cut point same as in Marcucci et al.29 For patients on protocol 19808, median ERG expression value used for cut point.
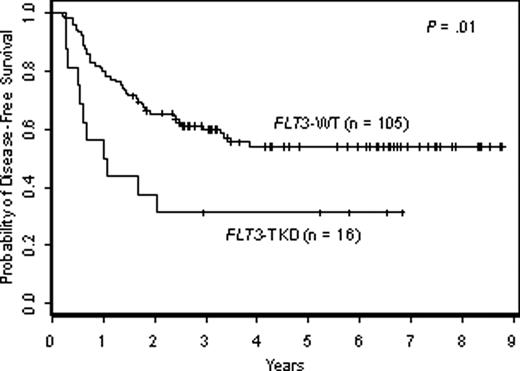
Clinical outcomes
No differences were observed between FLT3-WT and FLT3-TKD+ patients with respect to induction and consolidation treatments received on the 2 CALGB studies (Table 1). All patients with FLT3-TKD and 85% of patients with FLT3-WT achieved a CR (P = .13; Table 1). FLT3-TKD+ patients had significantly shorter DFS than FLT3-WT patients (P = .01). The estimated DFS rates at 3 years for the FLT3-TKD+ and FLT3-WT groups were 31% and 60%, respectively (Table 1; Figure 1). FLT3-TKD+ patients also tended to have worse OS, although the difference was not statistically significant (P = .17). The estimated OS rates at 3 years for the FLT3-TKD+ and FLT3-WT groups were 40% and 65%, respectively (Table 1).
Kaplan-Meier plot of disease-free survival of patients with FLT3-TKD and of those with wild-type FLT3 (FLT3-WT).
Kaplan-Meier plot of disease-free survival of patients with FLT3-TKD and of those with wild-type FLT3 (FLT3-WT).
In a multivariable analysis, the presence of a FLT3-TKD remained significantly associated with worse DFS (P = .02, Table 2), after adjusting for NPM1 mutational status (P = .02, Figure S1A, available on the Blood website; see the Supplemental Materials link at the top of the online article) and percentage of BM blasts (P = .17), a confounding variable. The estimated risk of relapse was 2.3 times higher for a FLT3-TKD+ patient compared with a similar FLT3-WT patient. The impact of FLT3-TKD on clinical outcome in the presence of BAALC or ERG expression status, for which information was available on only a subset of patients, was explored separately. Among low BAALC expressers, who were previously shown to have a more favorable outcome than high BAALC expressers,11,28 those with FLT3-TKD had significantly worse DFS than those with FLT3-WT (P = .003, Figure S1B). There was only one patient with both FLT3-TKD and high BAALC expression who relapsed within 9 months from achieving CR and died shortly thereafter; therefore, the impact of FLT3-TKD on high BAALC expressers could not be evaluated. With regard to ERG expression, patients with FLT3-TKD tended to have worse DFS than those without among both low and high ERG expressers, although no large differences were observed (Figure S1C).
Multivariable analysis for disease-free survival
| Variable* . | P . | Hazard ratio (95% CI) . |
|---|---|---|
| FLT3-TKD vs FLT3-WT | .02 | 2.3 (1.1-4.7) |
| NPM1-mutated vs NPM1-WT | .02 | 0.5 (0.3-0.9) |
| Percent BM blasts | .17 | 1.1 (1.0-1.3)† |
| Variable* . | P . | Hazard ratio (95% CI) . |
|---|---|---|
| FLT3-TKD vs FLT3-WT | .02 | 2.3 (1.1-4.7) |
| NPM1-mutated vs NPM1-WT | .02 | 0.5 (0.3-0.9) |
| Percent BM blasts | .17 | 1.1 (1.0-1.3)† |
Hazard ratios greater than (less than) 1 indicate an increased (decreased) risk of relapse for higher values of continuous variables and the first category listed for dichotomous variables.
FLT3-TKD indicates tyrosine kinase domain mutation of the FLT3 gene; FLT3-WT, wild-type FLT3; BM, bone marrow.
Variables considered for model inclusion were age, sex, race, hemoglobin, platelet and WBC count, percentage of blood and BM blasts, extramedullary involvement, MLL-PTD, and NPM1 mutation status. Only NPM1 mutation status, percentage of BM blasts, and WBC count had a P < .20 in univariable analyses and were fit with FLT3-TKD in a full model. The final model is shown.
Hazard ratio provided for a 10% increase in BM blasts.
The level of FLT3-TKD mutation was quantified in 14 of the 16 FLT3-TKD+ patients for whom material was still available. The percentage of FLT3-TKD mutation ranged from 54% to 100%, with 8 patients having 100% of the alleles mutated. Because all patients with FLT3-TKD achieved a CR, this endpoint did not depend on the percentage of FLT3-TKD mutation. Similarly, we found no significant relationship between the percentage of FLT3-TKD and OS or DFS using percentage of FLT3-TKD as a continuous variable (P = .68 and P = .31, respectively) or as a dichotomous variable (100% vs <100% mutated alleles; P = .68 and P = .30, respectively). Six of the 8 patients with 100% of mutant alleles relapsed compared with 3 of the 6 patients with less than 100% of mutant alleles; in both groups, one-half of the patients died.
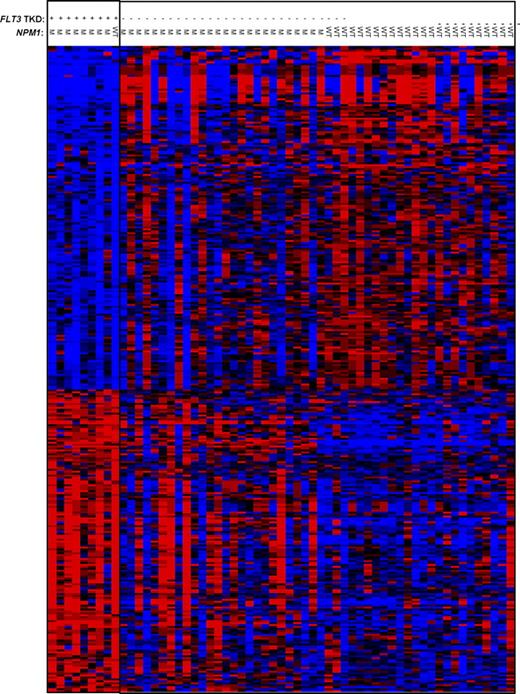
A gene-expression signature differentiating FLT3-TKD and FLT3-WT CN-AML
Gene-expression microarray analysis was performed on patient samples for which sufficient RNA material was available. We identified a signature consisting of 333 probe sets differentially expressed (P < .001) between FLT3-TKD+ and FLT3-WT patients (Figure 2; Table S1). Of the 9 FLT3-TKD+ patients included in the gene expression profiling analysis, 8 were NPM1-mutated. The single FLT3-TKD+ patient with NPM1-WT had a gene-expression signature that more strongly resembled the expression signatures of the FLT3-TKD+ patients with mutated NPM1 than it did the expression signatures of the FLT3-WT patients with NPM1-WT (Figure 2). FLT3-WT/NPM1-mutated patients were heterogeneous with respect to expression of the identified signature; some had a pattern of expression resembling the FLT3-TKD+ patients, whereas others had a pattern resembling the FLT3-WT patients with NPM1-WT (Figure 2). These observations imply that the identified FLT3-TKD signature is not solely driven by the mutated NPM1 status of the majority of FLT3-TKD+ patients.
Heat map of the FLT3-TKD–associated gene signature. Expression values of the 333 probe sets in the signature are represented by color, with blue indicating expression below and red expression above the median value for the given probe set. For display purposes, the expression values of the probe sets were centered so that each probe set has the same median expression value. Rows represent probe sets (Table S2, identification of probe sets) and columns represent patients. Patients are grouped by FLT3-TKD (+) and FLT3-WT (−) status. NPM1 status is indicated as mutation positive (M) or wild-type (WT).
Heat map of the FLT3-TKD–associated gene signature. Expression values of the 333 probe sets in the signature are represented by color, with blue indicating expression below and red expression above the median value for the given probe set. For display purposes, the expression values of the probe sets were centered so that each probe set has the same median expression value. Rows represent probe sets (Table S2, identification of probe sets) and columns represent patients. Patients are grouped by FLT3-TKD (+) and FLT3-WT (−) status. NPM1 status is indicated as mutation positive (M) or wild-type (WT).
The 333 probe sets represent 214 unique, named genes, of which 103 were overexpressed and 111 underexpressed in patients with FLT3-TKD relative to FLT3-WT patients. Among the 35 genes with 2-fold or higher expression in FLT3-TKD patients compared with FLT3-WT were VNN1 and C3AR1, involved in trafficking and homing, respectively; PTPN6 (also called SHP1), a negative regulator of activated FLT3; LFNG, involved in Notch signal transduction; and HOXB6, involved in development and hematopoiesis (Tables 3 and S1). Among the 31 genes underexpressed in FLT3-TKD patients with 2.0-fold or higher expression in FLT3-WT patients were MPO; RHOH, a negative regulator of signal transduction; and MLLT3 (also known as AF9), a transcription factor involved in t(9;11)(p22;q23), a recurrent translocation in AML (Tables 3 and S1). Furthermore, several genes in the signature with less than a 2-fold difference in expression between FLT3-TKD and FLT3-WT have been previously linked to FLT3-WT and/or FLT3-ITD biology, including LYN, a SRC family kinase,33,34 and TCF3, involved in Wnt signaling35 (Table S1).
Genes differentially expressed 2-fold or greater in the FLT3-TKD signature
| Gene symbol . | Description . | Fold change . |
|---|---|---|
| Overexpressed in FLT3-TKD patients | TKD/WT | |
| VNN1* | Vanin 1 | 5.64 |
| TREM1 | Triggering receptor expressed on myeloid cells 1 | 4.87 |
| HOXB6 | Homeobox B6 | 4.34 |
| CACNA2D4* | Calcium channel, voltage-dependent, α2/Δ subunit 4 | 4.07 |
| VNN2 | Vanin 2 | 3.67 |
| C3AR1 | Complement component 3a receptor 1 | 3.62 |
| EPB41L3* | Erythrocyte membrane protein band 4.1-like 3 | 3.42 |
| EVI2A | Ecotropic viral integration site 2A | 3.02 |
| PKM2 | Pyruvate kinase, muscle | 2.95 |
| OSCAR | Osteoclast-associated receptor | 2.92 |
| ITGAX | Integrin, αX (complement component 3 receptor 4 subunit) | 2.91 |
| CD93 | CD93 molecule | 2.87 |
| GNS* | Glucosamine (N-acetyl)-6-sulfatase (Sanfilippo disease IIID) | 2.82 |
| UPB1 | Ureidopropionase, β | 2.81 |
| ADAM8* | ADAM metallopeptidase domain 8 | 2.70 |
| SLC16A3* | Solute carrier family 16, member 3 (monocarboxylic acid transporter 4) | 2.50 |
| CD300LB | CD300 molecule-like family member b | 2.45 |
| MYO1G | Myosin IG | 2.43 |
| HAVCR2 | Hepatitis A virus cellular receptor 2 | 2.40 |
| ARHGEF3 | ρ guanine nucleotide exchange factor (GEF) 3 | 2.32 |
| MMP19 | Matrix metallopeptidase 19; similar to matrix metalloproteinase-19 precursor (MMP-19) (matrix metalloproteinase RASI) (MMP-18) | 2.29 |
| PTPN6 | Protein tyrosine phosphatase, non-receptor type 6 | 2.26 |
| CD300A* | CD300a molecule | 2.24 |
| CARD14 | Caspase recruitment domain family, member 14 | 2.23 |
| TCIRG1 | T-cell, immune regulator 1, ATPase, H+ transporting, lysosomal V0 subunit A3 | 2.22 |
| CD300C | CD300c molecule | 2.12 |
| ACSL4 | Acyl-CoA synthetase long-chain family member 4 | 2.11 |
| SLC11A1* | Solute carrier family 11 (proton-coupled divalent metal ion transporters), member 1 | 2.11 |
| LFNG | Lunatic fringe homolog (Drosophila) | 2.09 |
| CTSD | Cathepsin D (lysosomal aspartyl peptidase) | 2.09 |
| CSF2RA | Colony stimulating factor 2 receptor, α, low-affinity (granulocyte-macrophage) | 2.08 |
| TNFRSF1A | Tumor necrosis factor receptor superfamily, member 1A | 2.05 |
| ST8SIA4 | ST8 α-N-acetyl-neuraminide α-2,8-sialyltransferase 4 | 2.05 |
| F12 | Coagulation factor XII (Hageman factor) | 2.03 |
| PSCA | Prostate stem cell antigen | 2.01 |
| Underexpressed in FLT3-TKD patients | WT/TKD | |
| GYPA | Glycophorin A (MNS blood group) | 5.75 |
| ERAF | Erythroid associated factor | 5.49 |
| HEMGN | Hemogen | 5.41 |
| MPO* | Myeloperoxidase | 5.31 |
| XK | X-linked Kx blood group (McLeod syndrome) | 5.24 |
| IL8 | Interleukin 8 | 5.15 |
| ALAS2 | Aminolevulinate, Δ-, synthase 2 (sideroblastic/hypochromic anemia) | 5.05 |
| EPB42 | Erythrocyte membrane protein band 4.2 | 4.42 |
| PRDX2* | Peroxiredoxin 2 | 3.98 |
| C1QTNF4 | C1q and tumor necrosis factor-related protein 4 | 3.73 |
| HBA1; HBA2* | Hemoglobin, α1; hemoglobin, α2 | 3.52 |
| ADD2 | Adducin 2(β) | 3.34 |
| HBA1 | Hemoglobin, α1 | 3.34 |
| PIP5K1B | Phosphatidylinositol-4-phosphate 5-kinase, type I, β | 3.33 |
| GYPC | Glycophorin C (Gerbich blood group) | 3.32 |
| MLLT3* | Myeloid/lymphoid or mixed-lineage leukemia (trithorax homolog, Drosophila); translocated to 3 | 3.26 |
| KLF1 | Kruppel-like factor 1 (erythroid) | 3.11 |
| GPR125 | G protein-coupled receptor 125 | 3.01 |
| GFI1B | Growth factor independent 1B (potential regulator of CDKN1A, translocated in CML) | 2.79 |
| RHOH | ras homolog gene family, member H | 2.76 |
| KEL | Kell blood group, metalloendopeptidase | 2.75 |
| BPGM | 2,3-bisphosphoglycerate mutase | 2.68 |
| FECH | Ferrochelatase (protoporphyria) | 2.42 |
| FAM46C | Family with sequence similarity 46, member C | 2.31 |
| PAIP1* | Poly(A) binding protein interacting protein 1 | 2.26 |
| PRKD3* | Protein kinase D3 | 2.23 |
| MLF1IP | MLF1 interacting protein | 2.16 |
| PGM2L1 | Phosphoglucomutase 2-like 1 | 2.11 |
| MGC4172 | Short-chain dehydrogenase/reductase | 2.08 |
| EGFL8; LOC653870 | EGF-like-domain, multiple 8; similar to palmitoyl-protein thioesterase 2 | 2.07 |
| TSPAN5 | Tetraspanin 5 | 2.07 |
| Gene symbol . | Description . | Fold change . |
|---|---|---|
| Overexpressed in FLT3-TKD patients | TKD/WT | |
| VNN1* | Vanin 1 | 5.64 |
| TREM1 | Triggering receptor expressed on myeloid cells 1 | 4.87 |
| HOXB6 | Homeobox B6 | 4.34 |
| CACNA2D4* | Calcium channel, voltage-dependent, α2/Δ subunit 4 | 4.07 |
| VNN2 | Vanin 2 | 3.67 |
| C3AR1 | Complement component 3a receptor 1 | 3.62 |
| EPB41L3* | Erythrocyte membrane protein band 4.1-like 3 | 3.42 |
| EVI2A | Ecotropic viral integration site 2A | 3.02 |
| PKM2 | Pyruvate kinase, muscle | 2.95 |
| OSCAR | Osteoclast-associated receptor | 2.92 |
| ITGAX | Integrin, αX (complement component 3 receptor 4 subunit) | 2.91 |
| CD93 | CD93 molecule | 2.87 |
| GNS* | Glucosamine (N-acetyl)-6-sulfatase (Sanfilippo disease IIID) | 2.82 |
| UPB1 | Ureidopropionase, β | 2.81 |
| ADAM8* | ADAM metallopeptidase domain 8 | 2.70 |
| SLC16A3* | Solute carrier family 16, member 3 (monocarboxylic acid transporter 4) | 2.50 |
| CD300LB | CD300 molecule-like family member b | 2.45 |
| MYO1G | Myosin IG | 2.43 |
| HAVCR2 | Hepatitis A virus cellular receptor 2 | 2.40 |
| ARHGEF3 | ρ guanine nucleotide exchange factor (GEF) 3 | 2.32 |
| MMP19 | Matrix metallopeptidase 19; similar to matrix metalloproteinase-19 precursor (MMP-19) (matrix metalloproteinase RASI) (MMP-18) | 2.29 |
| PTPN6 | Protein tyrosine phosphatase, non-receptor type 6 | 2.26 |
| CD300A* | CD300a molecule | 2.24 |
| CARD14 | Caspase recruitment domain family, member 14 | 2.23 |
| TCIRG1 | T-cell, immune regulator 1, ATPase, H+ transporting, lysosomal V0 subunit A3 | 2.22 |
| CD300C | CD300c molecule | 2.12 |
| ACSL4 | Acyl-CoA synthetase long-chain family member 4 | 2.11 |
| SLC11A1* | Solute carrier family 11 (proton-coupled divalent metal ion transporters), member 1 | 2.11 |
| LFNG | Lunatic fringe homolog (Drosophila) | 2.09 |
| CTSD | Cathepsin D (lysosomal aspartyl peptidase) | 2.09 |
| CSF2RA | Colony stimulating factor 2 receptor, α, low-affinity (granulocyte-macrophage) | 2.08 |
| TNFRSF1A | Tumor necrosis factor receptor superfamily, member 1A | 2.05 |
| ST8SIA4 | ST8 α-N-acetyl-neuraminide α-2,8-sialyltransferase 4 | 2.05 |
| F12 | Coagulation factor XII (Hageman factor) | 2.03 |
| PSCA | Prostate stem cell antigen | 2.01 |
| Underexpressed in FLT3-TKD patients | WT/TKD | |
| GYPA | Glycophorin A (MNS blood group) | 5.75 |
| ERAF | Erythroid associated factor | 5.49 |
| HEMGN | Hemogen | 5.41 |
| MPO* | Myeloperoxidase | 5.31 |
| XK | X-linked Kx blood group (McLeod syndrome) | 5.24 |
| IL8 | Interleukin 8 | 5.15 |
| ALAS2 | Aminolevulinate, Δ-, synthase 2 (sideroblastic/hypochromic anemia) | 5.05 |
| EPB42 | Erythrocyte membrane protein band 4.2 | 4.42 |
| PRDX2* | Peroxiredoxin 2 | 3.98 |
| C1QTNF4 | C1q and tumor necrosis factor-related protein 4 | 3.73 |
| HBA1; HBA2* | Hemoglobin, α1; hemoglobin, α2 | 3.52 |
| ADD2 | Adducin 2(β) | 3.34 |
| HBA1 | Hemoglobin, α1 | 3.34 |
| PIP5K1B | Phosphatidylinositol-4-phosphate 5-kinase, type I, β | 3.33 |
| GYPC | Glycophorin C (Gerbich blood group) | 3.32 |
| MLLT3* | Myeloid/lymphoid or mixed-lineage leukemia (trithorax homolog, Drosophila); translocated to 3 | 3.26 |
| KLF1 | Kruppel-like factor 1 (erythroid) | 3.11 |
| GPR125 | G protein-coupled receptor 125 | 3.01 |
| GFI1B | Growth factor independent 1B (potential regulator of CDKN1A, translocated in CML) | 2.79 |
| RHOH | ras homolog gene family, member H | 2.76 |
| KEL | Kell blood group, metalloendopeptidase | 2.75 |
| BPGM | 2,3-bisphosphoglycerate mutase | 2.68 |
| FECH | Ferrochelatase (protoporphyria) | 2.42 |
| FAM46C | Family with sequence similarity 46, member C | 2.31 |
| PAIP1* | Poly(A) binding protein interacting protein 1 | 2.26 |
| PRKD3* | Protein kinase D3 | 2.23 |
| MLF1IP | MLF1 interacting protein | 2.16 |
| PGM2L1 | Phosphoglucomutase 2-like 1 | 2.11 |
| MGC4172 | Short-chain dehydrogenase/reductase | 2.08 |
| EGFL8; LOC653870 | EGF-like-domain, multiple 8; similar to palmitoyl-protein thioesterase 2 | 2.07 |
| TSPAN5 | Tetraspanin 5 | 2.07 |
The gene was represented by multiple probe sets in the identified signature. The displayed fold change is the average (geometric mean) of all the probe sets for the gene.
Gene ontologies associated with the FLT3-TKD signature
To gain further insight into the biologic importance of the gene-expression signature and uncover functional patterns associated with FLT3-TKD, we identified overrepresented gene ontology (GO) terms among the 215 known genes that made up the expression signature. Thirty-two GO terms (P ≤ .005) were enriched among the 103 genes overexpressed in FLT3-TKD patients (Figure S2). These included terms related to the cellular membrane (Figure S2A) and to transmembrane transport (eg, symporter activity and monocarboxylic acid transporter activity; Figure S2B,C). Analyzing the 111 underexpressed genes associated with FLT3-TKD, 28 GO terms were overrepresented (P ≤ .005, Figure S3). Included among these highly enriched ontologies were regulation of transcription, RNA metabolism, and positive regulation/activation of c-JUN n-terminal kinase (JNK) activity (Figure S3B).
Discussion
This study evaluates the prognostic impact of FLT3-TKD in younger adults diagnosed with de novo CN-AML in the absence of FLT3-ITD and reports the first Affymetrix-derived gene-expression signature differentiating FLT3-TKD and FLT3-WT. The frequency of FLT3-TKD in our patient set is consistent with previous reports in CN-AML, as is the finding of higher WBC counts and percentages of BM blasts in association with FLT3-TKD+ patients relative to FLT3-WT patients.13,15,24 We show that FLT3-TKD is associated with reduced remission duration relative to FLT3-WT patients in our patient cohort with de novo CN-AML.
A recent Medical Research Council (MRC) study suggested that FLT3-TKD presence was an indicator of better prognosis among AML patients.24 In an analysis restricted to CN-AML patients, Mead et al24 observed a trend for FLT3-TKD+ patients to have longer OS. Reasons for the outcome differences among CN-AML patients related to FLT3-TKD in our study and the aforementioned MRC study24 include, but are likely not limited to, sampling variability, the fact that in the Mead et al24 study, OS of CN-AML patients was evaluated comparing FLT3-TKD+ with FLT3-TKD− patients, inclusive of patients with FLT3-ITD, (see Figure 4B in Mead et al24 ), whereas our comparison group did not contain FLT3-ITD+ patients, and differences in post-CR intensification therapies, which included allogeneic transplantation in the MRC study24 and autologous transplantation in the CALGB study.
In our multivariable analysis, FLT3-TKD predicted worse DFS after controlling for NPM1 mutation status and percentage of BM blasts. The impact of FLT3-TKD on DFS in the presence of other prognostic markers such as BAALC and ERG was less clear. We observed for the first time a significant association between the presence of FLT3-TKD and low BAALC expression, which has previously been shown to confer more favorable prognosis than high BAALC expression in CN-AML.11 Among patients with low BAALC, those with FLT3-TKD had significantly reduced DFS. Thus, testing for FLT3-TKD may further refine molecular classification of a subset of CN-AML patients who do not harbor FLT3-ITD and have low BAALC expression.
In addition, Mead et al24 reported that a higher percentage of FLT3-TKD mutations contributed to a better cumulative index of relapse and OS compared with patients with a lower percentage of FLT3-TKD mutations.24 However, in the 14 CALGB samples for which DNA was available to perform the fluorescence-based quantification assay, we observed no differences in DFS or OS between patients having high or low FLT3-TKD percentages.
We also gained insights into the biologic mechanisms potentially underlying CN-AML with FLT3-TKD from gene-expression profiling and ontology analyses. Because AML is a disease thought to arise from at least 2 mutational hits, one affecting a signaling protein such as FLT3 and another involving a transcription factor,36 our finding of highly overrepresented GOs associated with transcription and RNA metabolism in the FLT3-TKD signature is not unexpected. These ontologies were associated with genes significantly underexpressed in FLT3-TKD+ CN-AML. However, more surprising were the enriched ontologies associated with sym- or trans-porter activity of mainly monocarboxylates in the genes significantly overexpressed in FLT3-TKD+ CN-AML. Monocarboxylates, such as butyrate and valproate, are known to have multiple cellular effects, including alterations in gene transcription via chromatin remodeling by histone deacetylases.37,38 Inconsistent with this increase in expression of monocarboxylate transporters in association with FLT3-TKD, we observed underexpression in FLT3-TKD+ relative to FLT3-WT patients of the PTPLAD1 gene, also called HSPC121, a butyrate-induced transcript whose protein product is involved in regulation of JNK and MAPK activities. This tentatively implies that proteins involved with monocarboxylate transport might not be functioning properly and perhaps their overexpression could be regarded as an attempt to compensate for their abnormal functions. In addition, the underexpression of genes involved in negative regulation of proliferation and survival signaling pathways is consistent with the observation of higher WBC counts and percentages of BM and blood blasts in patients with FLT3-TKD.
Several genes whose protein products are potential targets of small molecule drugs were observed as differentially expressed between FLT3-TKD and FLT3-WT patients. C3AR1, overexpressed in FLT3-TKD+ patients, encodes the C3a anaphylatoxin receptor, an important inflammatory mediator in the innate and adaptive immune systems that has been reported to be an enhancer of hematopoietic stem/progenitor cell homing-related responses to the SDF1/CXCR4 axis.39 VNN1, which was the most overexpressed gene in our set of FLT3-TKD+ patients, promotes trafficking of hematopoietic cells to the thymus, exerts a dominant control over innate immune response40 and plays a role in oxidative-stress response via its pantetheinase activity.41 Targeting of C3AR1 or SDF1/CXCR4, for which inhibitors are available (SB290157 and AMD3100, respectively) or possibly inhibitors to VNN1 pantetheinase activity may provide additional clinical benefit, perhaps more so in the postautologous transplantation setting, although further basic research is needed to support or refute this.
Significant overexpression of LYN, encoding a SRC family tyrosine kinase having cell context-dependent signaling roles, in the FLT3-TKD signature is also of interest, because recent in vitro data have suggested that targeting LYN may be clinically beneficial in AML patients with mutationally activated FLT3.34 However, LYN was also reported to enhance etoposide-mediated apoptosis.42 Because induction treatment of patients studied by us included etoposide, it is not unreasonable to postulate that LYN overexpression might have contributed to the 100% CR rate in the FLT3-TKD+ patients. Lastly, in our dataset, the underexpression of genes that positively regulate JNK activity in the FLT3-TKD+ patients suggests that JNK activity may be aberrant in FLT3-TKD+ patients. However, it has been demonstrated that FLT3 activity induces constitutive phosphorylation and activation of JNK, and this plays a significant role in enhanced proliferation and survival of leukemic blasts.43 Hence, it would appear that, if JNK activity is sufficiently increased in AML with mutationally activated FLT3, this might signal the cell to down-modulate the expression of redundant JNK positive regulatory mechanisms, as was observed in our analysis. A recent study on AML cell lines and primary leukemic blasts with activated FLT3 via FLT3 overexpression or FLT3-ITD demonstrated that inhibition of JNK activity reduces proliferation, induces apoptosis, and sensitizes cells to daunorubicin.43 However, cytarabine, one of the 3 agents that also included daunorubicin, used during induction in CALGB 9621 and 19808 treatment protocols, is most efficient in cells that are rapidly cycling; the high CR rate of CN-AML patients with FLT3-TKD may be attributed in part to the presumed increase in JNK activity. Thus, if one is to pursue the implementation of JNK inhibitors in combination with conventional chemotherapeutics for the treatment of FLT3-TKD associated AML, our data would suggest that a thorough investigation of the optimal timing of JNK inhibitors with or without cytarabine would be needed.
In conclusion, this study shows that for younger adults with de novo CN-AML lacking FLT3-ITD, having FLT3-TKD mutations in D835/I836 is associated with worse DFS than that of similar patients without FLT3-TKD. Therefore, CN-AML patients with FLT3-TKD may benefit from more aggressive postinduction therapies, such as allogeneic transplantation or novel molecularly targeted therapeutic approaches. Large phase III clinical trials, such as the one currently in development to investigate midostaurin (PKC412, Novartis), a selective FLT3 inhibitor, in combination with an intensive chemotherapy regimen, is likely to provide additional insights. Finally, although it is recognized that confirmation of our data and additional functional data are necessary, the gene-expression signature presented here appears to be informative of pathways that warrant further exploration as potential targets for development of novel therapies.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank The Ohio State University Comprehensive Cancer Center's Nucleic Acid and Microarray Shared Resources for their outstanding services. The authors gratefully acknowledge sample processing and storage services provided by Donna Bucci of the Cancer and Leukemia Group B Leukemia Tissue Bank at The Ohio State University Comprehensive Cancer Center, Columbus, Ohio.
This work was supported in part by the National Institutes of Health (grants CA101140, CA114725, CA077658, CA016058, CA102031, CA096887, CA089341, CA041287, and CA098933) and the Coleman Leukemia Research Foundation.
Authorship
Contribution: S.P.W., A.S.R., M.D.R., G.M., K.M., and C.D. Bloomfield contributed to the design and analysis of this study and the writing of this manuscript, and all authors agreed on the final version; S.P.W., P.P., C.L., C.D. Baldus, and J.W. carried out laboratory-based research; F.R. was the CALGB hematopathology cadre leader; A.S.R. and M.D.R. performed statistical analyses; and B.L.P., J.E.K., R.A.L., M.A.C., G.M., and C.D. Bloomfield were involved directly or indirectly in care of patients and/or sample procurement.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Susan P. Whitman, Division of Hematology and Oncology, Comprehensive Cancer Center, The Ohio State University, 2001 Polaris Parkway, Columbus, OH 43240; e-mail: susan.whitman@osumc.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal