Abstract
The meeting with the family of a hospitalized patient dying with advanced cancer or hematologic disease in which the limitation of life-sustaining interventions is discussed can be a challenge, particularly for junior physicians. A successful conclusion to this discussion involves an outcome in which the family, without coercion or manipulation, comes to accept that the appropriate care has been provided to their loved one, while the caregivers are enabled to provide care that is goal-directed and patient-centered. This type of result can be achieved through an approach in which patient-focused recommendations are offered in the context of diligent efforts to establish and sustain trust, thoughtful preparation, and respectful discussions with the family.
The patient's story*Mr R is a 60-year-old man who was diagnosed with multiple myeloma 4 years ago when he presented with anemia and rib pain. He was subsequently treated with high-dose induction chemotherapy followed by autologous stem cell transplantation and did well until 18 months ago when he was found to have new lytic lesions in his plevis. Since then he has been treated with various chemotherapeutic agents without a sustained response. Eight days ago he was admitted to the hospital with a left lower lobe pneumonia. He had obtained some initial improvement with broad-spectrum antibiotics, but over the past 5 days the pneumonia has progressed on his chest x-rays and he has required increasingly higher concentrations of supplemental oxygen (now on 50% venti-mask). Consequently, it is anticipated that he will require mechanical ventilation in the next 24 to 36 hours. His course has also been complicated by acute renal failure with anuria, and the renal service predicts he will require dialysis within 2 to 3 days. As Mr R is now very lethargic and minimally conversant, the medical team meets with his wife and children to discuss his level of care and the appropriateness of a transfer to the intensive care unit for ventilatory support and the initiation of dialysis.
Introduction
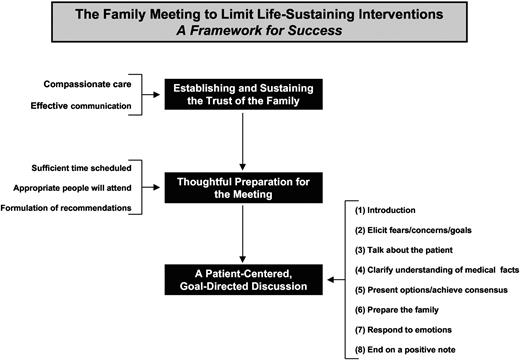
During the hospital course of a critically ill patient with advanced cancer or hematologic disease who ultimately dies, a pivotal event is often the meeting the physician has with the family to discuss the withholding or withdrawal of life-sustaining interventions.1,2 A successful conclusion to this conversation would include an outcome in which the family, without coercion or manipulation, comes to accept that the appropriate care has been provided to their dying loved one, while the medical team is simultaneously released to provide care that, from their perspective as professional caregivers, is goal-directed and comfort-centered.3 Achieving this kind of outcome is not a given and can be challenging, particularly for physicians who are in the early stages of their careers.1,4 Derived from personal experience, observations of exceptional caregivers, and a review of the literature, this article will describe some of the principles and preparations, as well as a recommended protocol, for achieving a successful family meeting (Figure 1). This article specifically focuses on the hospitalized patient lacking decision-making capacity. However, many of the features of this approach can also be adapted to the hospitalized patient who is competent to make decisions, as well as to end-of-life conversations with patients and their families in the outpatient setting.5
Principles for success
To speak effectively to families about limiting life-sustaining treatments for a dying patient who lacks decision-making capacity, an approach is favored in which care in its fullest sense, as distinct from only efforts at cure, is relentlessly sustained; intentional efforts are made to build trust; and decision-making is patient-centered. As outlined here, this approach provides a solid basis for mutually respectful end-of-life discussions with families about their loved one.
We never withhold or withdraw care
Although we may withhold cardiopulmonary resuscitation or withdraw mechanical ventilation or discontinue dialysis, at no time do we withhold, withdraw, or discontinue “care.”6 In other words, we can continue to do good and meaningful things (ie, care) for patients and their loved ones, even when cure is not possible and death is certain. And for many patients and families what is most often feared as death approaches is abandonment by the physicians and nurses—the withdrawal of effort, attention, compassion, and presence.7,8 It is therefore essential that the messages we provide, whether spoken or otherwise, never convey the sense that we have given up on or lost interest in the patient.9-11 In this regard it is important to never speak about “stopping,” “discontinuing,” or “ending” care, but to instead always frame these conversations in terms of actively pursing different, but achievable, goals of care.
The withholding and withdrawal of life-sustaining interventions is a process
To treat the decision to forgo life-sustaining treatments as one that merely involves an ad hoc, single, 10- to 15-minute conversation with the family is to invite difficulty with the patient's loved ones. Instead, the withholding and withdrawal of life-sustaining interventions must be seen as a process of trust-building, achieved by providing compassionate care and through effective communication.12,13 Seen in this way, the meeting to discontinue life-sustaining treatments is the culmination of a very intentional process, rather than an isolated event. Implicit in this is the recognition that trust should never be assumed, but earned; it can also be lost. Therefore, mentally stepping back, and patiently giving the family the time to witness the effort and dedication provided by the physicians and nurses, as they do their best to care for the patient, does much to demonstrate that the medical care team is deserving of the family's trust. And sustaining that trust includes honestly acknowledging mistakes and the uncertainties of care. Further, communication between the medical care team and the family of a critically ill loved one is effective when it is consistent and understandable; frequent and timely; honest and truthful; and always goal-directed and patient-centered.4,13 It also includes a sincere effort to listen respectfully, with a genuine curiosity, so as to understand the story and perspectives of both the patient and the family.6,14,15 In the intensive care unit (ICU) setting, intentional efforts, initiated early (within 72 hours of admission to the ICU), to effectively engage families in discussions about the direction and goals of care and the milestones indicative of recovery, promote an earlier transition to palliative care for dying patients, without an increase in mortality.13 I have also found that inviting families to join attending rounds is very often a helpful way of fostering trust and facilitating communication.6 This opportunity to participate in rounds, however, is a privilege, and should be revoked if the process and the work of rounds are disrupted by the presence of the family.
Decision-making must be patient-centered
The fears, anger, frustrations, and anticipated grief of the family need to be identified, acknowledged, and accommodated.16 In the end, however, the emotions, and any dysfunction within the family, cannot be allowed to drive end-of-life decisions for a dying patient. The same is true for members of the medical care team as well. Specifically, clinician assessments about the appropriate level of care for a critically ill or dying patient are likely to be distorted by a mindset in which patient death is seen as a personal failure or care is only understood as efforts aimed at cure. More is not necessarily better. In fact, for patients with advanced cancer, more aggressive medical treatment (eg, mechanical ventilation or resuscitation) is often associated with worse patient quality of life and worse bereavement adjustment.17
Instead, decision-making regarding a life-sustaining intervention for the patient who lacks capacity needs to emerge from the answers to 3 sequential questions.18,19 First, is the treatment medically appropriate and/or beneficial to the patient at this time? In this regard, the physician is under no ethical or legal obligation to provide treatments that are clinically inappropriate or physiologically ineffective.20 Second, if it is both appropriate and potentially beneficial, is this treatment that the patient would have desired and accepted in the current situation? When an advance directive is unavailable or unhelpful (which is often the case), this determination must involve a careful understanding of the patient's goals and values and an appreciation of how the patient lived his/her life. Lastly, if the treatment is both appropriate and potentially beneficial, but it is unclear what the patient would have accepted, is the treatment in the patient's best interest? This involves an assessment of whether the intervention provides meaningful benefits to the patient that outweigh its burdens. Professional, familial, and wider societal values all contribute to this determination.
Preparations for success
The reality is that spontaneous or unplanned meetings with the family to limit life-sustaining interventions do occur and can certainly be successful. However, attention to details such as scheduling an adequate amount of time, ensuring that the right people will be present, and coming to the meeting with a thoughtful recommendation increase the chances of achieving success with the family.
Schedule sufficient time
Given the approach that will be recommended, the family meeting should be scheduled for at least 30 minutes (although depending on the circumstances and if all goes well, it may end sooner), but routinely should not last longer than an hour.21 It has been my experience that if a consensus about the direction of care has not been reached in an hour, then it is unlikely it will be achieved at that time. To continue the meeting beyond that point is to run the risk of frustration and anger on the part of everyone. Better to end the meeting and re-group on another day. In addition, due to the preparation required, the length of the meeting, and the nature of the issues discussed, spontaneous, unplanned meetings at the bedside or in the hallway are not ideal.
Ensure that the appropriate people will attend
In terms of the family, it is essential to have not only the decision-maker(s) (legal or otherwise) attend, but to also have present all relevant “stakeholders” in the family, particularly that person who because of his or her status or influence in the family may exercise a veto over any decision that might be made. The physician leading this conversation, as a rule, should not plan to do this conversation alone, but should have at least 1 other member of the physician/nurse care team also present. This helps to send the message that the effort to change the direction of care is the consensus of the entire team and not just the decision of a single person. And where appropriate, it can also be helpful to include the patient's primary care provider(s), relevant consulting services, pastoral care, and social work in the meeting. In the end, the more multidisciplinary the meeting, the more likely it is to be successful.2,22
Formulate recommendation/options
In my nearly 20 years of experience as an attending physician in the ICU at tertiary hospital caring for very sick patients, I have found that it is important to come to the meeting with a well-thought-out, specific recommendation, or defined set of options for the family that would be open to modification and negotiation during the meeting, depending on the specific situation. This should be developed based on a thorough understanding of all the patient's relevant medical issues, including prognosis, and whatever knowledge is available about the patient's goals and values, the internal dynamics of the family, and the family's preferred role in decision-making.2 Treatments and interventions that are medically inappropriate, ineffective, or lacking in benefit, while open for discussion, should not be presented as options for care. And when the only meaningful option is comfort care, there should be no hesitation in presenting it as such.
It is also important to formulate the treatment recommendations with input from the nurses, housestaff, and other involved medical services. In this regard, it can be very helpful to, in advance, discuss with the critical care service the benefits and burdens of a transfer to the ICU. Not only does this multidisciplinary input enhance the quality of the recommendations offered to the family, it also ensures that all the relevant medical caregivers are “on the same page” and thus able to provide a consistent message to the family about the changes in the direction of care.2 In addition, premeeting consultations with support service such as palliative care, pastoral care, and/or social work can be valuable in informing the medical team about institutional, community, and spiritual supports/resources that are available and might be helpful to the family.23 These services may also be helpful in facilitating the discussion during the family conference, particularly when the clinicians may be uncomfortable or inexperienced with these types of conversations. Obviously, whatever plan is developed should be consistent with the policies of the institution and any relevant legal statues.
A recommended protocol for success
In the approach presented (Figure 1) and others similar to it,21,24 the conversation focuses initially on the family before getting to the “agenda” of the medical team (ie, a recommendation to change the direction of care).25 Throughout the meeting the patient's loved ones are informed, supported, and affirmed; the life and values of the patient are reviewed; and an effort is made to end on a positive note. Suggestions for how this might be done are listed in Table 1. In this approach the physician plays a collaborative role in the decision-making process, fostering a discussion that culminates in a patient-centered physician recommendation.26 This contrasts with family conferences in which the physician merely provides information about the patient's condition or facilitates a conversation about the values and goals of the patient, but in either situation refrains from making definitive recommendations about the direction of care.26 Readers are directed to the recent paper by White and colleagues for a more extensive description, with comparisons, of these various approaches.26 Although specific situations may compel one role over the others, the issue of whether one approach is the most ethically appropriate or clinically effective is beyond the scope of this article. However, recent empirical data indicate that physicians most often assume a collaborative role in these end-of-life conversations,26 and the limited studies we do have in this area suggest the majority of surrogates of critically ill patients do desire recommendations about the direction of care from the physicians.27
A recommended protocol for success: suggested ways of saying and doing it
| Introductions |
| “I want to thank you for taking the time to meet with us. I know the last several days have been difficult for the family. Today I want to update you on Mr R's medical condition and then, together with you, decide where we go next in caring for him. However, before we do that, I would like to have everyone introduce themselves, stating your relationship to Mr R.” |
| Eliciting fears, concerns, and goals |
| “As we sit here, what is your biggest fear?” |
| “What is weighing most heavily on your heart right now?” |
| “At this time, what is most important to you?” |
| “Do have any concerns about the care we have provided or the way we have treated you?” |
| [The responses of the family may provide opportunities to offer empathic statements.] |
| Getting the family to talk about the patient |
| “I know a lot about Mr R's medical condition, but I really don't know who he was as a person. Please tell me what made him special or unique or different.” |
| “What things were important to him?” |
| “What activities or hobbies did he enjoy?” |
| Determining/clarifying the family's understanding of the medical facts |
| “I know the nurses and physicians have tried to keep the family informed about what has been going on with Mr R. However, we may have confused you or even forgot to mention something. Can you [eg, the wife] tell me your understanding of what is going on with your husband?” |
| [Their understanding is accurate.] “You are correct. He came to the hospital with a pneumonia that was caused by….” [It is valuable to restate things to ensure that there is no confusion.] |
| [Their understanding is inaccurate.] “To what you have said let me add a couple of things….” |
| Presenting recommendations and achieving a consensus on the direction of care |
| “We are at a point where I can say his chances of ever getting well enough to leave the hospital are very, very small. Based on what you told me about the kind of person he was, and the way he lived his life, it is my sense that he might not want to be placed on ventilator, when there is little chance of recovery? What are your thoughts on that?” |
| “It is the conclusion of the medial team, after careful thought, that the chances of Mr R leaving the hospital and doing things he use to enjoy are very small. What do think he would tell us to do if he were here now?” |
| “You mentioned earlier that he has been through a lot and that you don't want him to suffer unnecessarily if it does not look like he will get better. I must say that transferring him to the ICU, putting him on a ventilator, starting dialysis, and subjecting him to CPR does run the risk of increasing his suffering without a guarantee that he will necessarily become well enough to return home. Based on that, I believe we should focus on making sure that he is comfortable and that he does not suffer. How does that sound to you?” |
| Preparation of the family |
| “Going forward, if his heart stops beating we will not attempt to restart it and if he runs into breathing problems we will not put him on a ventilator. Instead, we will keep him on this floor and focus on making sure he is comfortable. We will watch him closely for any signs of distress and will be sure to treat him immediately. To help us do that we will consult the palliative care team. Does this seem clear to you?” |
| A response to the question “How long will it take?”: “From my experience, it may take a day or 2 before he dies. Patients, however, sometimes will remain with us a little longer than we anticipate, and therefore it is important to be prepared for that.” |
| “I want to stress that as you go through this, the nurses and doctors will be with you.” |
| Experiencing the emotions of the moment |
| A response to “We really thought he was going to get better.”: “After having such high expectations, all this must be incredibly frustrating and disappointing to you.” |
| A response to “He was such a good man. Why should this happen to him.”: “I agree, all this seems so unfair.” |
| As the loved ones are weeping and grieving: “I share your sadness that he will not be with us anymore.” |
| The challenges of decision-making: “Making these kinds of decisions for loved ones are never easy.” |
| [Remember the value of silence.] |
| Ending on a positive note |
| “Before we close, please tell me something special or funny or memorable about Mr R.” |
| “I know that prayer is important to you. I therefore would like to have the chaplain give us a prayer.” |
| “I sincerely thank you for being here today and for helping us make these difficult decisions.” |
| Introductions |
| “I want to thank you for taking the time to meet with us. I know the last several days have been difficult for the family. Today I want to update you on Mr R's medical condition and then, together with you, decide where we go next in caring for him. However, before we do that, I would like to have everyone introduce themselves, stating your relationship to Mr R.” |
| Eliciting fears, concerns, and goals |
| “As we sit here, what is your biggest fear?” |
| “What is weighing most heavily on your heart right now?” |
| “At this time, what is most important to you?” |
| “Do have any concerns about the care we have provided or the way we have treated you?” |
| [The responses of the family may provide opportunities to offer empathic statements.] |
| Getting the family to talk about the patient |
| “I know a lot about Mr R's medical condition, but I really don't know who he was as a person. Please tell me what made him special or unique or different.” |
| “What things were important to him?” |
| “What activities or hobbies did he enjoy?” |
| Determining/clarifying the family's understanding of the medical facts |
| “I know the nurses and physicians have tried to keep the family informed about what has been going on with Mr R. However, we may have confused you or even forgot to mention something. Can you [eg, the wife] tell me your understanding of what is going on with your husband?” |
| [Their understanding is accurate.] “You are correct. He came to the hospital with a pneumonia that was caused by….” [It is valuable to restate things to ensure that there is no confusion.] |
| [Their understanding is inaccurate.] “To what you have said let me add a couple of things….” |
| Presenting recommendations and achieving a consensus on the direction of care |
| “We are at a point where I can say his chances of ever getting well enough to leave the hospital are very, very small. Based on what you told me about the kind of person he was, and the way he lived his life, it is my sense that he might not want to be placed on ventilator, when there is little chance of recovery? What are your thoughts on that?” |
| “It is the conclusion of the medial team, after careful thought, that the chances of Mr R leaving the hospital and doing things he use to enjoy are very small. What do think he would tell us to do if he were here now?” |
| “You mentioned earlier that he has been through a lot and that you don't want him to suffer unnecessarily if it does not look like he will get better. I must say that transferring him to the ICU, putting him on a ventilator, starting dialysis, and subjecting him to CPR does run the risk of increasing his suffering without a guarantee that he will necessarily become well enough to return home. Based on that, I believe we should focus on making sure that he is comfortable and that he does not suffer. How does that sound to you?” |
| Preparation of the family |
| “Going forward, if his heart stops beating we will not attempt to restart it and if he runs into breathing problems we will not put him on a ventilator. Instead, we will keep him on this floor and focus on making sure he is comfortable. We will watch him closely for any signs of distress and will be sure to treat him immediately. To help us do that we will consult the palliative care team. Does this seem clear to you?” |
| A response to the question “How long will it take?”: “From my experience, it may take a day or 2 before he dies. Patients, however, sometimes will remain with us a little longer than we anticipate, and therefore it is important to be prepared for that.” |
| “I want to stress that as you go through this, the nurses and doctors will be with you.” |
| Experiencing the emotions of the moment |
| A response to “We really thought he was going to get better.”: “After having such high expectations, all this must be incredibly frustrating and disappointing to you.” |
| A response to “He was such a good man. Why should this happen to him.”: “I agree, all this seems so unfair.” |
| As the loved ones are weeping and grieving: “I share your sadness that he will not be with us anymore.” |
| The challenges of decision-making: “Making these kinds of decisions for loved ones are never easy.” |
| [Remember the value of silence.] |
| Ending on a positive note |
| “Before we close, please tell me something special or funny or memorable about Mr R.” |
| “I know that prayer is important to you. I therefore would like to have the chaplain give us a prayer.” |
| “I sincerely thank you for being here today and for helping us make these difficult decisions.” |
Primarily one person should lead this discussion, with the other medical caregivers providing moral support, observing the dynamics of the meeting, and sharing comments as appropriate. In addition, members of the care team should be dispersed, if feasible, throughout the room, because having all of the medical providers clustered together can send a subtle message of “us against them.” In addition, when possible, pagers and cell phone should be turned off or silenced during the meeting to limit interruptions. Although this is framed as taking place in a single meeting, the steps outlined below may, by design or necessity, actually occur over more than 1 meeting. And admittedly, in many ways, the end-of-life discussion is ideally a rolling conversation that occurs frequently, if not daily, if there is ongoing communication with the family about the goals and direction of care.
Introductions
Begin with a brief introduction about the purpose and goal of the meeting, thanking the family for taking the time and making the effort to be present. These meetings will often involve people who may be new or unfamiliar to the medical team and thus in that setting it is helpful to have everyone give their name and relationship to the patient. When the number of loved ones is large, I find it helpful to write down their names and then refer to each person by name as the opportunity arises during the conversation.
Elicit fears, concerns, and goals
After the introductions, begin the conversation by asking the family to share their greatest fear, concern, or burden, or what is most important to them at this time. This is valuable to do for several reasons. First, by letting the family “go first,” it sends an unspoken message of respect. Second, it provides an opportunity for the family to therapeutically express feelings and emotions (fear, guilt, anticipated grief, loss, disappointment) that have been repressed, but which need to be released. Third, the responses of the family may provide opportunities for expressions of empathy that allow the medical team to further connect with the family.28,29 Fourth, the family may offer information that will enable you to frame your recommendation(s) in a way that speaks to what is most important to them at that time. Lastly, there may be unstated anger over some perceived, or real, insult, disrespect, or lapse in care. It is important to identify this anger because it may distract or consume the family in ways that limit their openness to the recommendations of the medical team. Consequently, it can be very helpful to simply ask if the family is satisfied with the care that the patient has received.
Have the family talk about the patient
During the course of a patient's illness, families often focus so intently on the medical issues that they come to lose sight of who their loved one was and what has been meaningful, important, and valuable to the patient. This loss of patient focus by the family can distort decision-making. It therefore can be very valuable to refocus the family by asking them to talk about the patient, with particular attention to those things that were important to and/or unique, special, or different about their loved one. This information about the patient can also be helpful to the medical team. By providing some sense of who the patient was and what he/she means to the family, it helps to humanize the patient to the physicians and nurses and thus enables them to better connect and empathize with the family. In addition, what has been learned about the values, goals, and life choices of the patient can often be used to present the recommendation(s) for care in patient-centered terms that are more likely resonate with the family.
Determine/clarify the family's understanding of the medical facts
Even when there have been sincere efforts to inform the family about the patient's medical condition, it should not be assumed that they have a complete or accurate understanding of what has occurred to the patient and/or the patient's current clinical status.30,31 I therefore next ask a family member, typically the primary decision-maker or that person who has been most attendant at the bedside, to describe his/her understanding of what has occurred to their loved one and the current medical status of the patient. This provides an opportunity to clarify any misconceptions or misunderstandings the family might have about the patient's medical condition. By having the family describe the patient's medical condition, it may also have the added benefit of having them say verbally what they may have been trying diligently to not acknowledge to themselves.
Present recommendations and achieve a consensus on the direction of care
Having given the family the opportunity to be heard first, one is now in a position to present the recommendation(s) of the care team. If indicated, the information learned from the initial conversation with the family should be used to shape what is actually offered to the family. Of more importance is the fact that this information can often be effectively used to frame the options for the family in a way that would have meaning and relevance to them, particularly when comfort care is the only appropriate option. If several options are presented they should be ranked from the most to the least appropriate. Most families do not view the withholding of prognostic information as an appropriate way of sustaining their hope,32-34 and thus the clinicians should not shy away from talking honestly and openly about their best determination of the patient's prognosis. If a living will is available, now is the time to introduce it into the conversation. And throughout this phase of the discussion, the decision should be framed for the family in terms of the goals/values or best interest of the patient. Further, the decision should be presented as something that is shared, rather than a burden that is solely on the family.35
If the family is initially resistant to the recommendation(s) of the medical team, then efforts should be made to patiently continue the discussion, without displaying frustration, attempting to understand and then respond to the family's concerns. Table 2 presents some common comments by families and suggested responses. When the resistance persists, the goal should then be to negotiate a compromise in which the family does not feel marginalized or dismissed, while the care team is enabled to go forward with a sense that they have begun to move in a direction of more comfort-centered care. If a consensus cannot be achieved, another meeting may be required, and/or the institution's procedures for conflict resolution may need to be initiated.
Suggested responses to specific statements by the family
| Statements by the family . | Comments . | Suggested physician responses . |
|---|---|---|
| “My dad was always a fighter.” | Families want, and need to be assured that every appropriate effort has been made to restore the health of their loved one. | “Not all fights are meant to be won. Accepting this, but recognizing that your father was a fighter, the key question is, have we done everything we could to make it possible for him to win this fight? I can assure you we have.” |
| “My dad would want us to do everything.” | “Doing everything” should be understood as doing everything that is medically appropriate. There is no obligation to provide, at the demands of family members, treatments that are medially ineffective or lacking physiological benefit. | “I can assure you that we have done everything possible to make your father better. To make sure we have not missed anything, we consulted … and did the following studies … (briefly/succinctly list major problems and efforts made to address them). Although we are not able to make him better, we will do everything possible to make sure he is comfortable and does not suffer.” |
| “I am not ready to let my husband go.” | Expressions of anticipated grief or loss at this time are normal. An effective response is one that compassionately acknowledges the emotions the family is experiencing, while suggesting some things that might help them cope with their loss. | “When you love someone as you certainly do, the time will never feel right to let him go. But I do believe there are things you can hold on to, like memories of shared experiences; the pride you both enjoyed around your children or grandchildren; or your hope in seeing him in heaven (if they have that belief).” |
| “We know that things are hopeless, but we believe a miracle will occur.” | In responding to a family that has this belief, the goal is not to present arguments that intellectually overwhelm the family. Instead, through patient and respectful discussions, the family is provided with information and fresh perspectives that they can use to reshape their thinking and understanding of the current situation. This effort begins by attempting to understand the meaning and significance of a miracle to the family (see DeLisser36 and Feudtner37 ). | “Miracles can mean different things to different people. What does a miracle mean to you? What would a miracle look like?” |
| As a subsequent or follow-up question ask: | ||
| “Assuming that a miraculous healing might not occur, are there other things that you would like to hope for? |
| Statements by the family . | Comments . | Suggested physician responses . |
|---|---|---|
| “My dad was always a fighter.” | Families want, and need to be assured that every appropriate effort has been made to restore the health of their loved one. | “Not all fights are meant to be won. Accepting this, but recognizing that your father was a fighter, the key question is, have we done everything we could to make it possible for him to win this fight? I can assure you we have.” |
| “My dad would want us to do everything.” | “Doing everything” should be understood as doing everything that is medically appropriate. There is no obligation to provide, at the demands of family members, treatments that are medially ineffective or lacking physiological benefit. | “I can assure you that we have done everything possible to make your father better. To make sure we have not missed anything, we consulted … and did the following studies … (briefly/succinctly list major problems and efforts made to address them). Although we are not able to make him better, we will do everything possible to make sure he is comfortable and does not suffer.” |
| “I am not ready to let my husband go.” | Expressions of anticipated grief or loss at this time are normal. An effective response is one that compassionately acknowledges the emotions the family is experiencing, while suggesting some things that might help them cope with their loss. | “When you love someone as you certainly do, the time will never feel right to let him go. But I do believe there are things you can hold on to, like memories of shared experiences; the pride you both enjoyed around your children or grandchildren; or your hope in seeing him in heaven (if they have that belief).” |
| “We know that things are hopeless, but we believe a miracle will occur.” | In responding to a family that has this belief, the goal is not to present arguments that intellectually overwhelm the family. Instead, through patient and respectful discussions, the family is provided with information and fresh perspectives that they can use to reshape their thinking and understanding of the current situation. This effort begins by attempting to understand the meaning and significance of a miracle to the family (see DeLisser36 and Feudtner37 ). | “Miracles can mean different things to different people. What does a miracle mean to you? What would a miracle look like?” |
| As a subsequent or follow-up question ask: | ||
| “Assuming that a miraculous healing might not occur, are there other things that you would like to hope for? |
Prepare the family for what will occur
Once the family has accepted the change in the direction of care, they should then be given a precise and understandable description of what this means and how it will occur. It should be emphasized that throughout the process comfort will be the primary goal and that the staff will respond immediately to any signs of distress. When something like mechanical ventilation, pressors, dialysis, or artificial nutrition and hydration is withheld or withdrawn, families will invariably ask how long it will take for their loved one to die. The response to this question should be an honest, reasonable estimate, while explicitly acknowledging the uncertainty of these kinds of predictions.32-34 In this regard it is more helpful to speak in terms of “minutes to hours” or “hours to days,” rather than offering a specific time.38 As noted previously, families fear abandonment, either physically or emotionally, by the medical team. Therefore it is vital to emphasize to the family that the commitment and attention of the physicians and nurses to their well-being and the care of the patient will not only continue, but also increase.10,11
Don't be afraid to experience the emotions of the moment
Family meetings to limit or discontinue life-sustaining interventions are more often than not infused with much sadness and grief. As you witness the tears and pain of the family, it is easy to be moved emotionally or even overwhelmed by their loss. Many physicians, particularly young physicians, will find this very discomforting, especially as they sense they might be losing control. Often, the response to this discomfort is to over-talk the situation and/or quickly end the meeting, before they “lose it.” In these moments of intense emotion, it is okay to slow things down, to say nothing and to simply allow the emotion to take over the room. If there is nothing to say, or one does not know what to say, then a few seconds of silence is perfectly fine.38 And if tears come, that is o.k., too. On the other hand it can be helpful to both the family and the staff to explicitly name and acknowledge the emotions and feelings that are being experienced and expressed as well as affirm support for the family. These opportunities to express empathy are often missed by physicians during family conferences,28 but are certainly welcomed and helpful to the families.29
End on a positive note
Finally, it is important to end the meeting in some uplifting or upbeat way. For me this most often involves asking the family to share something personal, special, humorous, quirky, or memorable about the patient and then encouraging them to go forward, reflecting on this and similar aspects of the patient's life. In addition, if the family has given evidence that prayer is important to them, I may also ask one of the loved ones or, if present, the chaplain or their clergy, to offer a brief prayer. I also offer the services of the institution's pastoral care department and/or encourage them, if appropriate, to access the spiritual resources in their faith community.39,40 As the conference closes, acknowledge the difficulty of the situation and the decisions made,35 again thanking the family for participating in the meeting. There is evidence that providing the family with targeted written material on bereavement at the end of the meeting may decrease the subsequent emotional burdens experienced by the family.21
Concluding comments
This review has focused on the challenges that families face in deciding, in conjunction with the medical team, the direction of care for a dying loved one who lacks decision-making capacity. The burdens on families of having to make these decisions can be eased, often very significantly, if patients have had prior, meaningful discussions about end-of-life issues with their loved ones. Given this, a diagnosis of a malignancy, particularly if it is associated with intensive treatments such stem cell transplants or aggressive chemotherapeutic regimens, should be a prompt for clinician-initiated planning for end-of-life care that is based on the goals and values of the patient.2,4,38 To do this is not to deny the potential for a cure or remission, but only to be prepared for all possibilities. This can involve a process of conversation and reflection on the part of the patient that begins with and is informed by the clinician, and continues with the patient's family and loved ones. Ideally, the process concludes with an advance directive (or some written documentation in the medical records) that summarizes the goals and direction of care as defined by the patient.
Finally, in using any recipe, great chefs will not only add additional ingredients to reflect their taste and style, but are prepared to adapt and improvise when specified ingredients are unavailable. They also recognize that sometimes, despite doing exactly what the recipe calls for, the item being prepared will, inexplicably, fail to turn out right. The same is also true for this recipe for a successful family meeting. In other words, develop an approach that is comfortable and authentic for you; families may not allow you to follow the formula outlined here, and so you must be prepared to adapt and improvise; and there will be instances where, even in the best of hands, success is elusive. However, your approach is more likely than not to succeed if patient-focused recommendations are offered in the context of respectful and sincere discussions, preceded by diligent efforts at building and sustaining trust.
This is a fictional case for illustrative purposes. Any similarity to an actual case is coincidental.
Acknowledgments
The author appreciates the helpful reviews and comments provided by the following colleagues from the University of Pennsylvania Health System: Mark Mikkelsen, MD (Pulmonary, Allergy and Critical Care Division) and chaplains Ralph Ciampa and John Ehman (Pastoral Care).
Authorship
Contribution: H.M.D. reviewed the literature and wrote the paper.
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Horace M. DeLisser, MD, Pulmonary, Allergy and Critical Care Division, SVM-Hill Pavilion, Rm 410B, 380 S University Ave, Philadelphia, PA 19104-3945; e-mail: delisser@mail.med.upenn.edu.