Abstract
Abstract 3090
Several biologic markers have been identified which predict an unfavorable course in CLL. Reduced-intensity conditioning (RIC) allogeneic transplant may be able to overcome some of these. This retrospective analysis evaluates the effect of cytogenetics, including metaphase cytogenetics, on outcomes with RIC-allogeneic SCT.
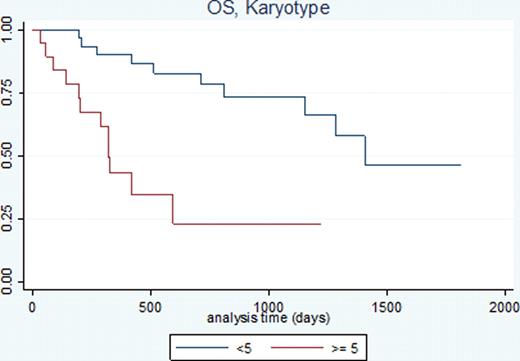
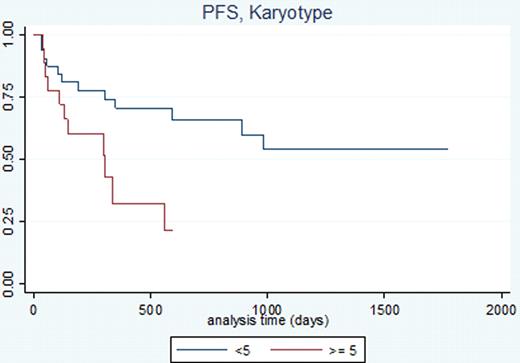
From 2005–2011, 51 RIC-allogeneic SCTs were performed at The Ohio State University for CLL. There were 38 males (74.5%) and 13 females (25.5%) with a median age of 58 (range 37–73). The median interval between diagnosis and SCT was 48 months (range 9–270). Before SCT, a median 4 lines of chemotherapy were given (range 1–11). One patient was in CR at the time of SCT, 39 were in PR, and 11 had stable or progressive disease; the median CMI was 3 (range 0–7). Fifty-nine percent of patients had del17; 53% had 3 or more abnormalities on metaphase cytogenetics, and 37% had 5 or more abnormalities. The source was PBSC in 48 (94%), BM in 1 (2%) and CB in 2 (4%). Of the PB or BM SCTs, 19 donors (39.6%) were related and 29 (60.4%) were volunteer; 45 (92%) were matched and 4 (8%) had a 1 allele mismatch. There were 21 (41%) pairs with an ABO mismatch and 16 (31.4%) pairs with a gender mismatch. Conditioning was Flu/Bu +/− ATG in 42 patients (82.2%), FluCamTBI in 6 (11.8%), FluCy in 1 (2%), and FluCyTBI-based in 2 receiving CB (4%). Following transplant, 34 (66.6%) developed AGVHD (gr 1–2: 28, gr 3–4: 6) and 27 of 48 evaluable patients (56.3%) developed CGVHD (limited: 7, extensive: 20). With a median follow-up of 17.3 months (range 1–60), the estimated 3-year OS and PFS following transplant were 56.5% and 42.9% respectively. Table 1 lists variables which had a p-value of ≤0.1 on univariate analysis. The presence of del13 and ≥5 karyotype abnormalities remained significant on multivariate analysis for OS while ≥5 karyotype abnormalities and conditioning with an alemtuzumab-containing regimen were significant for PFS (Table 2). The estimated 3 year OS for patients with del13 was 32.2% and 23% for patients with ≥5 karyotype abnormalities, compared with 72.7% and 73.5% for those without, respectively. The estimated 3-year PFS was 21.5% for patients with ≥5 karyotype abnormalities and 0% for patients with an alemtuzumab-containing regimen and 53.9% and 49.3% for those without, respectively.
Variables included in multivariate analysis model.
| Variable . | logrank p-value . | PFS . |
|---|---|---|
| OS . | ||
| Age ≥55 | 0.0072* | … |
| Del13 ≥4.7% | 0.0039* | |
| Del17p ≥5.7% | 0.0019* | 0.0878 |
| Karyotype abnormalities ≥5 | 0.0002* | 0.0138* |
| Karyotype abnormalities ≥3 | 0.0186* | 0.0623 |
| Largest node ≥4 cm | 0.0277* | … |
| Marrow involvement ≥50% | 0.0752 | … |
| Alemtuzumab conditioning | … | 0.0001* |
| GVHD prophylaxis | 0.0001* | 0.0374* |
| HLA mismatch | <0.0001* | … |
| Variable . | logrank p-value . | PFS . |
|---|---|---|
| OS . | ||
| Age ≥55 | 0.0072* | … |
| Del13 ≥4.7% | 0.0039* | |
| Del17p ≥5.7% | 0.0019* | 0.0878 |
| Karyotype abnormalities ≥5 | 0.0002* | 0.0138* |
| Karyotype abnormalities ≥3 | 0.0186* | 0.0623 |
| Largest node ≥4 cm | 0.0277* | … |
| Marrow involvement ≥50% | 0.0752 | … |
| Alemtuzumab conditioning | … | 0.0001* |
| GVHD prophylaxis | 0.0001* | 0.0374* |
| HLA mismatch | <0.0001* | … |
statistically significant at p<0.05
Multivariate analysis of OS, PFS.
| OS . | |||
|---|---|---|---|
| Variable . | HR . | 95% CI . | p-value . |
| Del13q | |||
| <4.7% | 1 | ||
| ≥4.7% | 3.58 | 1.36 to 9.42 | 0.01 |
| Karyotype | |||
| <4 | 1 | ||
| ≥5 | 5.16 | 1.97 to 13.56 | 0.001 |
| PFS | |||
| Variable | HR | 95% CI | p-value |
| Conditioning | |||
| no alemtuzumab | 1 | ||
| alemtuzumab | 9.8 | 3.28 to 29.29 | 0 |
| Karyotype | |||
| <4 | 1 | ||
| ≥5 | 4.35 | 1.67 to 11.28 | 0.002 |
| OS . | |||
|---|---|---|---|
| Variable . | HR . | 95% CI . | p-value . |
| Del13q | |||
| <4.7% | 1 | ||
| ≥4.7% | 3.58 | 1.36 to 9.42 | 0.01 |
| Karyotype | |||
| <4 | 1 | ||
| ≥5 | 5.16 | 1.97 to 13.56 | 0.001 |
| PFS | |||
| Variable | HR | 95% CI | p-value |
| Conditioning | |||
| no alemtuzumab | 1 | ||
| alemtuzumab | 9.8 | 3.28 to 29.29 | 0 |
| Karyotype | |||
| <4 | 1 | ||
| ≥5 | 4.35 | 1.67 to 11.28 | 0.002 |
OS and PFS by Karyotype
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal