Abstract
Abstract 4123
Deletion 17p is the principal predictor of poor outcome in CLL pts after conventional chemotherapy. Several reports have shown better outcomes with NST. However, questions have risen as to the relevance of NST, in particular, to the extent that various selection biases lead to selection of only the “best” pts for this procedure.
Our primary goal is to update our NST experience with 17p-, and to report how often pts underwent transplantation and, within the limits of retrospective analysis, the reasons they did not.
We reviewed NST outcomes for 17p- CLL pts transplanted between 2005 (when FISH became routinely performed at our institution) and 2010. Given the poor outcome after conventional FCR, a diligent effort started in 2007 by the Leukemia Service to refer pts to transplant sooner rather than later. Therefore, in a sub-analysis, we reviewed the number of 17p- CLL pts who were referred to Transplant Consult service since 2007 and assess the reasons for no transplant. Prognostic factors were evaluated using Cox's regression model. Multivariate analysis was not possible given sample size limitation.
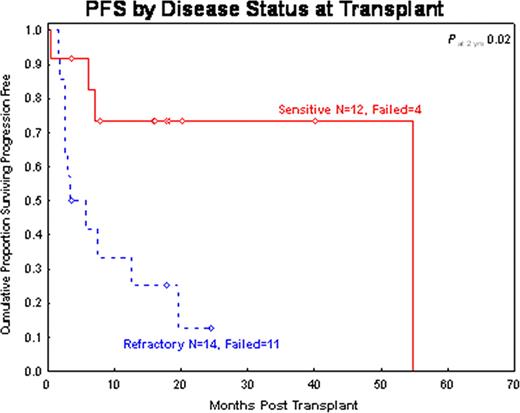
Outcome of NST in 17p- CLL pts. Twenty-six pts were transplanted at our institution between 2005 and 2010. Median age (range) was 56 yrs (37–73). At NST, 15 pts (58%) had a β2m >3; 21/24 (87%) had stage Binet B/C; 4 pts (15%) had Richter's; 16/25 (64%) were FDG-avid; median prior chemotherapies (range) was 4(2–14), and 14 pts (54%) had refractory disease. 13 pts (50%) had complex cytogenetic abnormalities (in addition to 17p-). IgVH was unmutated in 11/12 (92%) pts tested, 14/15 (93%) were ZAP-70+. Prior to their transplantation, 24 pts (92%) were exposed to FCR, 11 (42%) to CFAR/OFAR, 7 (27%) to Hyper-CVAD, and 17 (65%) to alemtuzumab. With a median follow-up of 18 months (range, 3 – 60), the 2-year OS and PFS rates were 62% and 38%, respectively. On univariate analysis, determinants of outcomes included disease status, and β2m at NST, and year of transplant. All but one pt with chemosensitive disease had β2m >4 compared with 50% of pts with chemoresistant disease. Chemosensitivity was associated with significantly higher PFS (73% vs. 12%, p=0.02, Figure below) and a trend for higher OS (91% vs. 45%, p= 0.09). PFS was also significantly higher for transplants performed after 2007 (44% vs. 20%, p=0.03). β2m>4 was associated with lower 18 m OS (36% vs. 71%, p=0.05) in chemoresistant pts, but did not significantly impact PFS (38% vs. 14%, p=0.5). Two yrs follow-up was not reached for β2m >4 in this group.
Transplant consults and transplantation rate : Between September 2007 and March 2010, 59 pts with 17p- CLL received a Transplant Service consult. Twenty of these 59 pts (34%) did receive their transplant at the time of this analysis, whereas 39 (66%) did not. Reasons for not receiving transplants included: 1) Death with salvage pre-transplant chemo (n=14, 36%); 2) Pt and/or physician became uninterested after achieving good response to salvage chemo (n=14, 36%); 3) lost follow-up after the initial consult (n=3, 8%); 4) age >75 (n=2, 5%); 5) insurance denial (n=3, 8%); 6) no donor (n=1, 2%); 7) other (n=2, 5%).
NST is plausibly more effective in 17p- CLL pts when recipients have chemosensitive disease. If, as suggested by our analysis, at most 34% of pts receive this procedure, methods to extend the transplant's applicability are needed. Perhaps the most effective method would be to use NST as consolidation after initial response to conventional chemotherapy. Such a strategy would allow more pts to have chemosensitive disease at NST, and would decrease the death rate in heavily pre-treated pts during their pre-transplant cytoreductive therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal