Whereas the improvement in outcome for children with acute lymphoblastic leukemia has been gratifying, the poor outcome of patients who relapse warrants novel treatment approaches. Previously, we identified a characteristic relapse-specific gene expression and methylation signature associated with chemoresistance using a large cohort of matched-diagnosis relapse samples. We hypothesized that “reversing” such a signature might restore chemosensitivity. In the present study, we demonstrate that the histone deacetylase inhibitor vorinostat not only reprograms the aberrant gene expression profile of relapsed blasts by epigenetic mechanisms, but is also synergistic when applied before chemotherapy in primary patient samples and leukemia cell lines. Furthermore, incorporation of the DNA methyltransferase inhibitor decitabine led to reexpression of genes shown to be preferentially methylated and silenced at relapse. Combination pretreatment with vorinostat and decitabine resulted in even greater cytotoxicity compared with each agent individually with chemotherapy. Our results indicate that acquisition of chemo-resistance at relapse may be driven in part by epigenetic mechanisms. Incorporation of these targeted epigenetic agents to the standard chemotherapy backbone is a promising approach to the treatment of relapsed pediatric acute lymphoblastic leukemia.
Introduction
Relapsed acute lymphoblastic leukemia (ALL) is one of the leading causes of death among children with cancer. A hallmark of relapsed blasts is their intrinsic chemoresistance compared with what is observed at initial diagnosis.1,2 Given the frequent failure of conventional salvage chemotherapy, including intensified drug schedules and stem cell transplantation, in the treatment of relapsed ALL,3,4 innovative strategies are urgently needed.
In recent years, it has become clear that cancer can be driven by patterns of altered gene expression mediated not by mechanisms that affect the primary DNA sequence, but through the “epigenetic” processes of DNA-promoter methylation and histone modification.5,6 DNA methylation is catalyzed by DNA methyltransferases (DNMTs) and has been shown to be an important contributor to carcinogenesis, acting by silencing tumor suppressor genes in many tumor types, including hematologic malignancies.6,7 Chromatin structure is also regulated by the “histone code,” which refers to posttranslational modifications (ie, methylation, acetylation, phosphorylation, and ubiquitination) of key lysine residues on core histone proteins.8 These 2 epigenetic processes of DNA-promoter methylation and histone modifications are clearly interdependent and coordinated.9,,–12
DNMT inhibitors such as 5-azacitidine and decitabine have the potential to reverse promoter hypermethylation in tumor cells, leading to reexpression of aberrantly silenced genes and inducing tumor cell death.13 DNMT inhibitors have been demonstrated to be effective therapy for myelodysplastic syndrome, which is characterized by global promoter hypermethylation.14 Likewise, inhibition of histone deacetylases (HDACs) with HDAC inhibitors such as vorinostat can alter the balance in favor of histone acetyltransferases, resulting in an increased acetylation of histone H3K9 and H3K14 and gene transcription.15
Recently, we performed an integrated analysis to identify biological pathways underlying relapsed ALL using genome-wide gene expression arrays, single nucleotide polymorphism arrays, and DNA methylation arrays.16 We have identified a relapse-specific gene expression signature characterized by up-regulation of genes involved in regulation of the cell cycle and apoptosis (BIRC5, FOXM1, and GTSE1), DNA replication and repair (FANCD2), and nucleotide biosynthesis (TYMS, CAD, PAICS, ATIC, and DHFR), and by down-regulation of genes involved in sensitivity to thiopurines and alkylators (MSH6) and glucocorti-coids (BTG1 and NR3C1). In addition, our genome-wide methylation analysis revealed a distinctly higher cytosine-phosphate-guanine methylation level in the relapsed cohort compared with diagnosis,16 and for a subset of differentially methylated genes, concordant down-regulation of mRNA expression was observed, implicating epigenetic dysregulation in the acquisition of chemoresistance at relapse.
We hypothesized that there may be an existing drug that has an effect on gene expression that might mimic reversal of the relapse signature, which may therefore functionally restore chemosensitivity in leukemic blasts. We searched the Connectivity Map (cmap) database17,18 to “query” our relapse signature and identified the HDAC inhibitor vorinostat as the top candidate agent that could potentially endow a chemosensitive gene expression profile. We validated this finding by demonstrating reversal of the relapse signature in primary B-lymphoblastic leukemia patient samples and cell lines treated with vorinostat that correlated with modulation of key epigenetic histone modifications. We further questioned whether a DNMT inhibitor could reverse relapse-specific promoter hypermethylation and reexpress aberrantly silenced genes, and confirmed this in ALL cell lines treated with the DNMT inhibitor decitabine. Finally, we tested whether “epigenetic reprogramming” with each agent alone or with the combination of HDAC inhibitor and DNMT inhibitor may functionally restore chemosensitivity. By treating primary patient samples and cell lines with vorinostat and decitabine, we demonstrated in the present study enhanced chemosensitivity that was correlated with modulation of an aberrant relapse-specific signature. Our data suggest that incorporation of epigenetic agents into conventional treatment regimens may improve the outcome of relapsed childhood ALL.
Methods
Cells
Primary patient samples were collected from patients treated at the New York University Medical Center and from the Children's Oncology Group cell bank. Samples were collected under the respective center's institutional review board–approved cell-procurement protocols for children with ALL. Informed consent was obtained in accordance with the Declaration of Helsinki protocol. Of the total 7 samples, 4 were from initial diagnosis and 3 were collected at the time of relapse. Samples were enriched from diagnostic BM collections by Ficoll-Hypaque centrifugation and resuspended in fresh culture medium (RPMI 1640) containing 20% FBS; 0.01% insulin, transferrin, and sodium selenide (Sigma-Aldrich) solution; and 1% penicillin-streptomycin. The diagnosis of ALL was based on morphology and flow cytometric analysis of the immunophenotype.
The B-lineage leukemia cell lines Reh, RS4:11, and UOCB1; the B-lymphoma cell line Raji; and the B-myelomonocytic leukemia cell line MV4:11 were grown in RPMI1640 medium supplemented with 10% FBS, 10mM HEPES buffer, 1% penicillin/streptomycin under 5% CO2 at 37°C. All cell lines were purchased from the ATCC and were authenticated according to their protocols (http://www.atcc.org). Stock solutions of vorinostat (Cayman Chemical) and etoposide were prepared in DMSO, whereas doxorubicin, cytarabine, and decitabine (Sigma-Aldrich) were prepared in double-distilled water. Prednisolone (Pharmacia) was suspended in 0.9% NaCl. Drugs were serially diluted in RPMI and added to the culture medium at the indicated concentrations. Cells were incubated with chemotherapy for 24-48 hours.
Connectivity map
The cmap is a collection of genome-wide transcriptional expression data from cultured human cells treated with various bioactive small molecules. Using a nonparametric, rank-based, pattern-matching strategy based on the Kolmogorov-Smirnov statistic, this analysis provides a ranked order of individual treatment instances based on their similarity to a given gene expression profile. The current version of the cmap dataset (build02; www.broadinstitute.org/cmap) was used to “query” our relapse-specific gene expression signature. The relapse gene expression profile was derived from 49 diagnosis/relapse patient pairs analyzed on Affymetrix U133plus2.0 microarrays.16 Three hundred top-ranking genes (150 down-regulated and 150 up-regulated genes at relapse compared with diagnosis) were chosen based on a false discovery rate < 10% and a P value < .002. Because cmap contains gene expression signatures derived from the Affymetrix U133A platform, close to half of our probe-sets could not be analyzed. Therefore, the final list included 154 probe sets consisting of 56 up-regulated and 99 down-regulated genes (supplemental Table 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Gene expression analysis
RNA was isolated from 3 primary patient samples and 3 leukemia cell lines with or without treatment with 1μM vorinostat for 24 hours using RNeasy Mini Kits (QIAGEN), and quality was verified with an Agilent 2100 Bioanalyzer. In vitro transcription was completed with biotinylated UTP and CTP for labeling using the ENZO BioArray HighYield RNA Transcript Labeling kit (Enzo Diagnostics). Thirteen micrograms of labeled cRNA was fragmented and hybridized to Affymetrix U133Plus2 microarrays according to the Affymetrix protocol. Raw Affymetrix CEL files were processed with the standard Affymetrix probe modeling algorithm RMA. Background correction and quantile normalization were applied during the process. The processed data were stored in a matrix containing one intensity value per probe set in the gene cluster text (GCT) format file. Analyses were based on the GCT format files with a class label file created in the categorical class file (CLS) format. Different versions of the CLS files were created comparing different subsets of samples using applications of gene pattern. Two independent statistical methods, the χ2 test and random sampling, were used to test the significance of changes observed in the relapse-specific signature (154 probes) compared with the whole gene set (54 676 probes). Expression data discussed herein were deposited in the National Center for Biotechnology Information Gene Expression Omnibus (http://www.ncbi.nlm.gov/geo) as accession number GSE34880.
Quantitative RT-PCR analysis
To determine the relative expression of each gene of interest, total RNA was extracted using the RNeasy Mini Kit (QIAGEN), and RT-PCR was performed using the I-Script II complementary DNA Synthesis kit (Bio-Rad) and the PerfeCTA SYBR Green FastMix (Quanta Biosciences). Synthesis of PCR products was monitored by the DNA Engine Opticon System (MJ Research) and normalized to β2 microglobulin levels. Data were plotted relative to mRNA levels in control samples using the ΔCt or ΔΔCt method. PCR primers are listed in the supplemental data (supplemental Table 2). The Wilcoxon paired signed-rank test was used to test the significance of change.
Western blotting
Reh cells were treated with or without vorinostat (1μM) and cell lysates were prepared using the histone extraction protocol (acid extraction) following the manufacturer's instructions (Abcam). Lysates were probed with purified rabbit polyclonal anti-acetyl histone H3 at a 1:5000 dilution (06-599; Millipore) and the levels of acetyl-H3 were determined relative to a housekeeping gene, actin, at a 1:2000 dilution (Abcam). Signals were visualized using the Odyssey infrared imaging system (LI-COR).
ChIP
ChIP was carried out following the protocol provided by EZ-ChIP (Millipore) with a few modifications. Briefly, Reh cells (1 × 106) were grown in RPMI medium with 10% FBS with or without vorinostat (1μM) for 24 hours. Proteins were cross-linked to DNA with 1% formaldehyde added directly to the culture medium for 10 minutes at 37°C, followed by cell lysis with SDS. The cell lysates were sonicated to shear DNA to the length of 200-1000 bp. Chromatin solutions were precipitated overnight at 4°C using 2 μg of anti-H3K9ac (334481; QIAGEN), anti-H3K27me2 (ab24684; Abcam), anti H3K4me2/me3 (ab6000; Abcam), and anti-H3K9me3 (ab8898; Abcam). For the negative control, species-specific IgG was used. For the positive control, anti-RNA polymerase II (05-623; Millipore) was used. DNA from protein-associated complexes and corresponding input samples were recovered using the QIAquick PCR purification kit (QIAGEN), and assayed by real-time PCR under standard conditions. Primers were targeted to the transcription start site (TSS) and the upstream promoter regions of the genes of interest. Full details, including the primer sequences, are provided in supplemental Table 2.
Methylation-specific PCR
Genomic DNA was extracted from B-lineage leukemia cell lines (Reh and UOCB1) and B-lymphoma cell lines (Raji), and sodium bisulfite modification was performed using the Epitect bisulfite kit (QIAGEN) according to the manufacturer's protocol. Then, methylation-specific PCR (MSP) was performed as described previously.19 Completely methylated and unmethylated control DNA (Epitect PCR control DNA set; QIAGEN) was tested for each primer pair. PCR products were analyzed after electrophoresis on 2% agarose gels containing ethidium bromide. MSP primers are provided in supplemental Table 2.
Cell-viability assays
CellTiter-Glo Luminescent Cell Viability assays (Promega) were performed on primary patient samples and cell lines grown in the appropriate survival conditions. Briefly, cells were seeded in 96-well plates and treated with vorinostat and/or decitabine (0, 0.1, 0.5, 1, 2.5, and 5μM). After 24 or 48 hours of incubation, prednisolone, etoposide, doxorubicin, and cytarabine were added to the medium for an additional 24 hours of incubation. Finally, CellTiter-Glo reagent was added and luminescence was recorded using a Synergy HT multidetection microplate reader (BioTek Instruments). Drug-combination effects were analyzed with CalcuSyn software (Biosoft) using the combination index (CI) equation of Chou-Talalay.20 This application describes the drug interaction as: CI > 1.1, antagonism; CI = 0.9-1.1, additive; CI = 0.85-0.9, slight synergism; CI = 0.7-0.85, moderate synergism; CI = 0.3-0.7, synergism; CI = 0.1-0.3, strong synergism; and CI < 0.1, very strong synergism.
Results
Connectivity map analysis identifies vorinostat as the top candidate agent that could reverse the relapse-specific gene expression signature
After the identification of the relapse-specific drug-resistance signature, we searched the current version of the cmap database to identify agents that could potentially reverse this signature and restore chemosensitivity. All treatment instances from the database were ranked according to their negative connectivity scores with P < .05. Remarkably, compounds that ranked among the top were the HDAC inhibitors vorinostat and trichostatin A. The average connectivity score of the 12 treatment instances of vorinostat in various cancer cell lines in the cmap database was −0.659 (P = 0), whereas the 182 instances of trichostatin A had a connectivity score of −0.452 (P = 0; supplemental Figure 1). This analysis indicated that the genetic makeup of relapsed ALL might be epigenetically driven and, therefore, its reversal by HDAC inhibitors could potentially restore chemosensitivity.
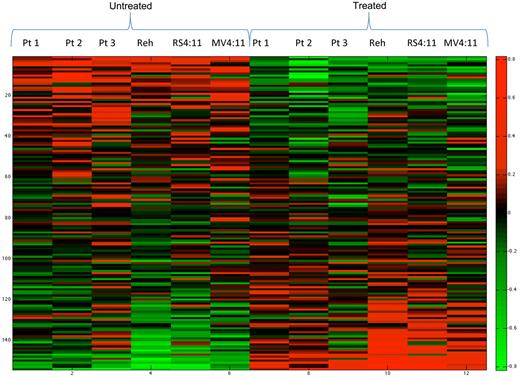
Gene expression microarrays and RT-PCR validates the cmap results
To validate and confirm the cmap findings, primary patient samples (n = 3) and leukemia cell lines (Reh, RS4:11, and MV4:11) were treated with 1μM vorinostat and incubated for 24 hours. RNA was extracted and gene expression profiling was performed using the Affymetrix U133Plus2 array. The expression of 38.7% (mean; 95% confidence interval across the 6 samples, 30.51%-46.18%) of genes differentially expressed at relapse was reversed after vorinostat treatment using the fold change of 0.8 and 1.2 for down- and up-regulated genes, respectively, and a P value < .05 (Figure 1). Details of individual genes and corresponding reversal on vorinostat treatment are provided in supplemental Table 1. To determine whether the relapse signature is enriched for genes that have an expression that is epigenetically regulated compared with the whole genome, we examined expression changes in genes using a more stringent fold change of 2. The expression of 17.8% (mean; 95% confidence interval across the 6 samples, 12.7%-22.8%) of the relapse-specific genes were reversed after vorinostat treatment, compared with only 12.8% (mean; 95% confidence interval across 6 samples, 8.8%-16.7%) genes were affected in the whole-genome analysis (P = .025 by χ2 test). This result was also validated using a random sampling method in which 10 000 random combinations showed that in only 185 instances could such a finding be attributable to chance alone (P = .019). These 2 independent methods showed a specific effect of vorinostat on the genes included in the relapse-specific signature. Microarray data were then validated by RT-PCR in a selected set of candidate chemoresistance genes from our previous study,16 which showed significant down-regulation of the expression of BIRC5, FOXM1, TYMS, and FANCD2 (genes up-regulated at relapse; Figure 2A), and an increase in the expression of NR3C1, HRK, and SMEK2 (genes down-regulated at relapse; Figure 2B).
Gene expression microarrays in primary B-lymphoblastic leukemia patient samples and cell lines reveal reversal of relapse-specific signature. Heat map showing the effect of vorinostat in reversing the relapse-specific gene expression profile. Rows represent individual genes (154 probes); relative overexpression is shown in red and underexpression in green. The first 3 columns are primary patient samples (1, 2, and 3), followed by the Reh, RS4:11, and MV4:11 cell lines, respectively, before treatment with vorinostat; the next 6 columns correspond to each sample after treatment.
Gene expression microarrays in primary B-lymphoblastic leukemia patient samples and cell lines reveal reversal of relapse-specific signature. Heat map showing the effect of vorinostat in reversing the relapse-specific gene expression profile. Rows represent individual genes (154 probes); relative overexpression is shown in red and underexpression in green. The first 3 columns are primary patient samples (1, 2, and 3), followed by the Reh, RS4:11, and MV4:11 cell lines, respectively, before treatment with vorinostat; the next 6 columns correspond to each sample after treatment.
Relative mRNA expression of genes differentially expressed at relapse after exposure to vorinostat. Quantitative RT-PCR validation of selected targets on 3 primary patient samples and Reh, RS4:11, and MV4:11 cell lines is shown. The x-axis represents the vorinostat concentration. The y-axis represents normalized ΔCT values (CT of gene of interest − CT of the housekeeping gene). CT indicates threshold cycles for amplification. Each experiment was performed in triplicate. Mean expression is indicated by the horizontal bars. P values correspond to Wilcoxon signed-rank test comparing the expression levels before and after treatment.
Relative mRNA expression of genes differentially expressed at relapse after exposure to vorinostat. Quantitative RT-PCR validation of selected targets on 3 primary patient samples and Reh, RS4:11, and MV4:11 cell lines is shown. The x-axis represents the vorinostat concentration. The y-axis represents normalized ΔCT values (CT of gene of interest − CT of the housekeeping gene). CT indicates threshold cycles for amplification. Each experiment was performed in triplicate. Mean expression is indicated by the horizontal bars. P values correspond to Wilcoxon signed-rank test comparing the expression levels before and after treatment.
Association of histone marks is correlated with vorinostat exposure as HDAC inhibitor
The biologic impact of vorinostat was validated by showing an increase in global histone acetylation at the protein level as measured by Western blot in Reh cells (Figure 3A). ChIP experiments were performed to examine the effect of vorinostat on specific activating (H3K4me2/3 and H3K9ac) and repressive (H3K9me3 and H3K27me3) histone marks that modulate gene expression. Chromatin from the vorinostat-treated and untreated Reh cells were immunoprecipitated with these Abs, and DNA was subjected to PCR amplification using primer sets designed to amplify the transcriptional start site and/or 5′ region of the genes of interest. We observed significant enrichment of the acetylation histone mark H3K9ac on the promoters of all of the genes tested (NR3C1, HRK, BIRC5, and FOXM1), indicating a direct effect of vorinostat in the accumulation of acetylated lysine 9 of histone H3 (Figure 3B). This observation was correlated with the transcriptional activation of NR3C1 and HRK in patient samples and cell lines after vorinostat treatment. In addition, we observed modest enrichment of H3K4me2/3 (activation mark) at the NR3C1 and HRK promoters, supporting the activation of these genes after vorinostat exposure. Of the repressive marks, we observed a decrease in the H3K9me3 mark on the promoters of all genes except FOXM1. The interplay of posttranslational methylation and acetylation at the same lysine residue (K9) further supports the effect of vorinostat in regulating the expression of NR3C1 and HRK, although this effect is not consistent with the observed down-regulation of BIRC5 and FOXM1. The H3K27me3 mark did not show significant modulation with vorinostat treatment in any of the genes tested (Figure 3B).
Histone modifications at the promoters of genes of interest. (A) Western blot analysis of acetyl-H3 (and actin loading control) in Reh cells with and without vorinostat exposure. (B) ChIP was carried out with Abs specific for key H3 modifications associated with transcriptional activation (K9ac and K4me2/3) and transcriptional repression (K9me3 and K27me3) and purified DNA was subjected to RT-PCR using primer sets designed to amplify the transcriptional start site and/or the 5′ region of NR3C1, HRK, BIRC5, and FOXM1. Each graph shows the modification of these marks after vorinostat exposure normalized to log input (1%) and the corresponding mRNA expression of the gene by quantitative RT-PCR. TSS indicates transcriptional start site.
Histone modifications at the promoters of genes of interest. (A) Western blot analysis of acetyl-H3 (and actin loading control) in Reh cells with and without vorinostat exposure. (B) ChIP was carried out with Abs specific for key H3 modifications associated with transcriptional activation (K9ac and K4me2/3) and transcriptional repression (K9me3 and K27me3) and purified DNA was subjected to RT-PCR using primer sets designed to amplify the transcriptional start site and/or the 5′ region of NR3C1, HRK, BIRC5, and FOXM1. Each graph shows the modification of these marks after vorinostat exposure normalized to log input (1%) and the corresponding mRNA expression of the gene by quantitative RT-PCR. TSS indicates transcriptional start site.
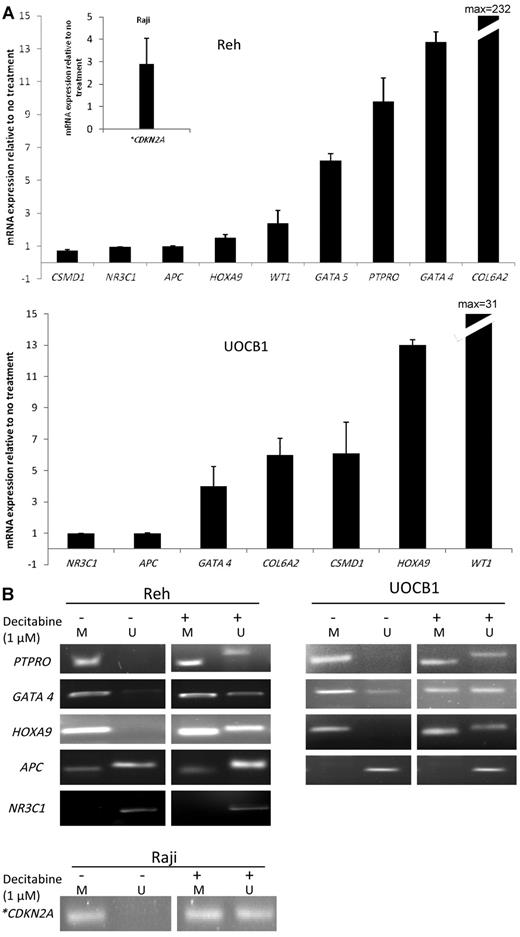
Treatment with the demethylating agent decitabine leads to reexpression of relapse-specific hypermethylated genes
Having identified the “methylome signature” of relapsed ALL previously,16 we sought to determine the impact of the demethylating agent decitabine in reexpression of relapse-specific silenced hypermethylated genes. Reh and UOCB1 cell lines were treated with 1μM decitabine and incubated for 48 (Reh) or 72 (UOCB1) hours. RNA was extracted and RT-PCR was performed on relapse-specific target genes. We focused on the genes that were identified from the integrated results of the cross-platform analysis (CDKN2A, COL6A2, PTPRO, and CSMD116 ) that were hypermethylated and down-regulated at relapse and focally deleted in a subset of samples. In addition, we examined other gene promoters that showed concordant hypermethylation and down-regulation in our relapse cohort, such as WT1, APC, GATA4, and HOXA9. We observed a 2- to 200-fold induction of expression of PTPRO, COL6A2, WT1, GATA4, and HOXA9 (Figure 4A). Reexpression of CDKN2A was examined in Raji (B-lymphoma cell lines) cells because both alleles are deleted in Reh cell lines,21 whereas its expression is lost in UOCB1 cell lines,22 and again observed a 2- to 4-fold induction in its expression. A 6-fold increase in expression of CSMD1 was observed in UOCB1 cells, whereas no change was observed in the Reh cell line. No change in the expression of APC was observed in either cell line tested. As a negative control, we tested the NR3C1 gene, which is down-regulated at relapse and was not found to be hypermethylated in our relapse cohort, although it has been shown to be hypermethylated in other cancer types.23 No change in the expression of NR3C1 was observed after decitabine treatment in either cell line.
Decitabine treatment of ALL cell lines shows reexpression of hypermethylated genes at relapse. (A) Real-time PCR was performed on Reh, UOCB1 (B-lineage), and Raji (lymphoma) cells treated with decitabine at a 1μM concentration for 48 hours (Reh and Raji) or 72 hours (UOCB1). Results are expressed relative to the levels observed at baseline without decitabine exposure. Each experiment was performed in triplicate. Error bars represent SD. (B) Determination of concordant changes in promoter methylation levels by MSP in Reh and UOCB1 cell lines. *CDKN2A mRNA expression levels and MSP were performed in Raji cells only.
Decitabine treatment of ALL cell lines shows reexpression of hypermethylated genes at relapse. (A) Real-time PCR was performed on Reh, UOCB1 (B-lineage), and Raji (lymphoma) cells treated with decitabine at a 1μM concentration for 48 hours (Reh and Raji) or 72 hours (UOCB1). Results are expressed relative to the levels observed at baseline without decitabine exposure. Each experiment was performed in triplicate. Error bars represent SD. (B) Determination of concordant changes in promoter methylation levels by MSP in Reh and UOCB1 cell lines. *CDKN2A mRNA expression levels and MSP were performed in Raji cells only.
MSP demonstrates the effect of decitabine on promoter hypermethylation and validates RT-PCR results
To demonstrate the direct effect of decitabine on promoter hypermethylation, MSP was performed with cell lines before and after treatment with decitabine. The PTPRO and HOXA9 genes were completely methylated in Reh and UOCB1 cell lines before treatment, and an enrichment of the unmethylated amplicon was observed after treatment with decitabine (1μM). The GATA4 promoter was preferentially methylated in both cell lines, although some unmethylation was also observed at baseline and this was significantly enriched after treatment with decitabine. The APC promoter was preferentially unmethylated in both Reh and UOCB1 cell lines, but had a faint methylation band in Reh cells at baseline. After decitabine treatment, the intensity of the methylation band was decreased and the unmethylated product was modestly increased in Reh cells, whereas it was unchanged in the UOCB1 cells. Preferential unmethylation of this promoter at baseline in these cell lines could be the reason for unaltered expression of this gene as determined by RT-PCR. The NR3C1 promoter was completely unmethylated before and after exposure to decitabine in both cell lines, which is the likely explanation for its insensitivity to decitabine treatment (Figure 4B). MSP for CDKN2A promoter performed in Raji cell lines showed enrichment of unmethylated product after decitabine exposure, which is consistent with the increase in expression shown by RT-PCR.
Pretreatment with vorinostat and/or decitabine induces chemosensitivity in primary patient samples and leukemia cell lines
Finally, to examine whether epigenetic priming translates to increased chemotherapy-induced cytotoxicity of leukemic blasts, we assessed cytotoxicity with a panel of chemotherapeutic agents commonly used in ALL therapy. Primary patient samples (n = 7) and Reh and RS4:11 cell lines were treated sequentially with increasing concentrations of vorinostat and/or decitabine at 0 hours, followed by application of conventional chemotherapeutic agents (prednisolone, doxorubicin, cytarabine, and etoposide) at various concentrations at 24 or 48 hours. Cytotoxicity assays were performed at 48 or 72 hours. Vorinostat alone induced 40%-60% of the cytotoxic effect at the maximal concentration of 2.5μM. An additive or synergistic effect was observed when cells were pretreated with vorinostat followed by chemotherapy in Reh and RS4:11 cell lines (CI = 0.5-1.05; supplemental Figure 2A-B). Similarly, decitabine alone induced 25%-40% of the cytotoxic effect at its maximal concentration used, and the addition of chemotherapy after decitabine pretreatment significantly increased the amount of cytotoxicity (CI = 0.34-0.9; supplemental Figure 2C-D). The 2 epigenetic drugs by themselves showed a mostly additive effect to moderate synergism (CI = 0.57-1.1), whereas pretreatment with both vorinostat and decitabine followed by prednisolone had the most robust cytotoxicity compared with any other combination, showing strong synergism (CI = 0.17-0.5; Figure 5A-D). As predicted from the cmap results, we did observe increased cytotoxicity in the relapse samples (n = 3) when vorinostat alone was followed by prednisolone (CI = 0.36-0.6) compared with the diagnosis samples (n = 4; CI = 0.43-1.0; Figure 5C-D), although the comparison was limited because of the small sample size. These data suggest that although both the diagnosis and relapse blasts can be sensitized to chemotherapy, the effect of vorinostat was more pronounced in the relapsed blast population. We did not see this effect with decitabine, with which the impact was equivalent at both initial diagnosis and relapse.
In vitro cell-viability assays in primary patient samples and cell lines (Reh and RS4:11). Summary graph representing the effect of all agents at 48-hour time point either individually or in combination in Reh cell lines (A), RS4:11 cell lines (B), relapse patient samples (C), and diagnosis patient samples (D) are shown. The x-axis represents the vorinostat and decitabine concentrations at 0, 0.1, 0.5, 1, 2.5, and 5μM and prednisolone at 0, 100, 200, 300, 400, and 500 μg/mL, respectively. The y-axis shows the percent survival.
In vitro cell-viability assays in primary patient samples and cell lines (Reh and RS4:11). Summary graph representing the effect of all agents at 48-hour time point either individually or in combination in Reh cell lines (A), RS4:11 cell lines (B), relapse patient samples (C), and diagnosis patient samples (D) are shown. The x-axis represents the vorinostat and decitabine concentrations at 0, 0.1, 0.5, 1, 2.5, and 5μM and prednisolone at 0, 100, 200, 300, 400, and 500 μg/mL, respectively. The y-axis shows the percent survival.
Discussion
ALL is the most common childhood cancer and the majority of children can be cured with current therapies; however, up to 20% of children relapse and their outcome remains dismal. Historically, there have been several obstacles to the successful treatment of relapsed ALL, and numerous efforts to improve outcome after relapse have been unsuccessful. Contemporary reinduction regimens have relied on significantly more aggressive approaches with higher doses and/or compacted drug schedules. These have not only failed to improve remission rates, but have also reached tolerability limits, with toxic death rates generally ranging from 3%-8%, but with reports of rates up to 19%.24 Therefore, further dose intensification is not a viable option for improving outcome. One of the major challenges faced at relapse is intrinsic chemoresistance.1,2 The results of the present study indicate that the chemo-resistance that drives relapse in ALL may be reversible by epigenetic reprogramming with DNMT and HDAC inhibitors. Our results indicate that vorinostat reverses significantly the expression of genes that are differentially regulated at relapse, some of which are linked to tumor formation and progression, and, most importantly, may have a role in chemoresistance. Of particular interest are BIRC5 and FOXM1, which are associated with a wide range of cancers25,,–28 and were up-regulated in our relapse signature. We demonstrated that expression of both of these genes could be decreased after vorinostat exposure. Improving chemosensitivity by performing knock-down experiments of BIRC5 has been shown by us26 and others29 and has further supported its role in chemoresistance. Similarly, down-regulation of genes such as NR3C1 and BTG1 have been linked previously to glucocorticoid resistance,30 and we observed herein increased expression of these genes after vorinostat treatment. In addition, up-regulation of genes involved in nucleotide biosynthesis and folate metabolism identified in the late-relapse (relapse > 36 months from diagnosis) cohort, such as TYMS, CAD, and DHFR, was reversed by treatment with vorinostat. The effect of HDAC inhibition on BIRC5, TYMS, and DHFR expression in B-ALL patient samples and cell lines is consistent with the results of previous studies in a variety of other tumor types.31,–33 Therefore, we have demonstrated that many genes differentially expressed at relapse compared with diagnosis are epigenetically regulated and can be reprogrammed with HDAC inhibitors. This reversal of gene expression results functionally in enhanced chemosensitivity of leukemic blasts.
Posttranslational modifications of histone tails, especially acetylation and methylation on lysine residues, play a pivotal role in regulating gene expression by controlling the access of key regulatory factors and complexes to chromatin.34,35 Although HDAC inhibitors are known to activate gene expression by antagonizing HDACs and opening up the chromatin structure, their effect on global gene expression patterns remains elusive and needs further investigation. Whereas our ChIP experiments offer an explanation for the vorinostat-mediated activation of repressed genes such as NR3C1 and HRK, we did not observe enrichment of repressive histone marks as a possible mechanism of vorinostat-induced down-regulation of BIRC5 and FOXM1. Conversely, we observed reciprocal interaction of acetylation and methylation marks at lysine 9 on histone H3, which is in agreement with previous studies showing their mutual exclusivity.35 In light of several reports suggesting the effect of these agents on various nonhistone proteins and transcription factors, we speculate that down-regulation of these genes may be mediated by an intermediate transcriptional regulator restored by HDAC inhibitor exposure. For example, p21 expression increases with vorinostat treatment in a dose-dependent manner,36 which in turn might repress FOXM1.37 The resultant decrease in the levels of FOXM1 may affect the levels of BIRC5, CCNB1, and FANCD2, as described previously.38 The fact that similar alterations of gene expression patterns were seen repeatedly and consistently in different primary patient samples and cell lines strongly favors its unique and specific action. Recently, Stumpel et al has also demonstrated HDAC inhibitor–mediated down-regulation of a subset of hypomethylated proto-oncogenes and resultant chemosensitivity in MLL-rearranged ALL, which supports our findings (although clear underlying mechanisms remain undetermined).39 Future studies involving ChIP sequencing might provide further insight to understand this complex network.
Genome-wide methylation assays have identified many cancer-related genes as substrates of DNMTs leading to epigenetic silencing. In the present study, we were able to show reexpression of many genes that were hypermethylated at relapse by both RT-PCR and concordant promoter hypomethylation by MSP. Of these, CDKN2A, PTPRO, and CSMD1 have been identified previously as tumor suppressors in many cancers,40,41 and reactivation with demethylating agents is a logical approach. Furthermore, WT1 and APC are inhibitors of the β-catenin/TCF/LEF complex and were differentially down-regulated and hypermethylated in the relapse cohort. In the present study, we have demonstrated a significant up-regulation of WT1 after decitabine exposure. However, there was no significant baseline hypermethylation of APC in the Reh and UOCB1 cell lines, and therefore, our results failed to demonstrate a decitabine effect. Finally and most importantly, not only was aberrant gene expression reprogrammed by these 2 agents, but combination treatment with vorinostat and decitabine synergized with standard chemotherapy agents to result in enhanced chemosensitivity. A larger sample size would be needed to further compare the effect of these agents on the diagnosis versus relapsed blasts.
The combination of vorinostat and decitabine has been tested previously in human leukemia and showed evidence of cell growth inhibition and gene silencing.42 Recently, Kalac et al also reported a highly synergistic combination of HDAC inhibitor (panobinostat) and DNMT inhibitor (decitabine) and association with unique gene expression and epigenetic profiles in large B-cell lymphoma.43 Although newer HDAC and DNMT inhibitors are under active investigation, in the present study, we focused on vorinostat and decitabine not only because they are Food and Drug Administration–approved, but also because phase 1 trials using these agents have shown their safety in the pediatric population.44,45 Reversal of the gene expression and methylation signature in our study was seen with 1μM concentrations of vorinostat and decitabine, respectively, a plasma concentration shown to be clinically achievable and tolerable in these phase 1 clinical trials. Ravandi et al reported this combination to be well tolerated in a phase 1 study in hematologic malignancies in adults.46 Additional support for the feasibility of this combination has been described in adults with solid tumors and non-Hodgkin lymphoma.47 Moreover, it has been shown in previous studies that apoptosis induced by these epigenetic agents is specific to the malignant cell population and has comparatively little or no activity against their normal counterparts (nonmalignant cells),48,–50 suggesting that incorporating these agents episodically in the standard reinduction chemotherapy for the treatment of relapsed ALL is feasible.
Overall, the results of the present study reveal an attractive approach to reversing the drug resistance gene signature to restore chemosensitivity in relapsed ALL and we validated this approach in preclinical assays. The data described herein have led to a multi-institutional phase 1 clinical trial evaluating the feasibility and safety of using the combination of these epigenetic agents that is set to accrue patients through the Therapeutic Advances in Childhood Leukemia and Lymphoma Consortium (http://www.clinicaltrials.gov as NCT01483690). Gene expression and methylation arrays and subsequent validation studies will be undertaken as part of correlative biology assays for this clinical protocol. Our data provide a strong rationale for undertaking such a trial to improve the cure rates in relapsed childhood ALL, which otherwise has a dismal prognosis.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Matthias Karajannis, Julia Meyer, and Laura Hogan for reviewing the manuscript and Rana Lamisa for technical assistance.
This research was supported by the National Institutes of Health (5 R01CA 140729-02 to W.L.C.), the New York University Cancer Center (support grant 5 P30 CA16087-30 and R21 CA161688 to M.J.B. and P.B. and K12 NCI CA96028 to M.J.B.), the Pediatric Cancer Foundation, an Ira Sohn Foundation fellowship grant, and the Leukemia & Lymphoma Society.
National Institutes of Health
Authorship
Contribution: T.B. and D.J.M. designed and performed the research, collected, analyzed, and interpreted the data, performed the statistical analysis, and wrote the manuscript; J.W. analyzed and interpreted the data and performed the statistical analysis; E.A.R., M.J.B., and P.B. designed the research and wrote the manuscript; and W.L.C. designed and directed the research, analyzed and interpreted the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: William L. Carroll, MD, NYU Cancer Institute, Smilow 1201, 522 First Ave, New York, NY 10016; e-mail: william.carroll@nyumc.org.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal