In this issue of Blood, Martínez-Cingolani et al identified that human thymic stromal lymphopoietin (TSLP), previously shown to be induced during skin inflammation, stimulates myeloid-related BDCA-1+ peripheral blood dendritic cells (DCs) to rapidly gain phenotypic characteristics of human epidermal Langerhans cells (LCs).1
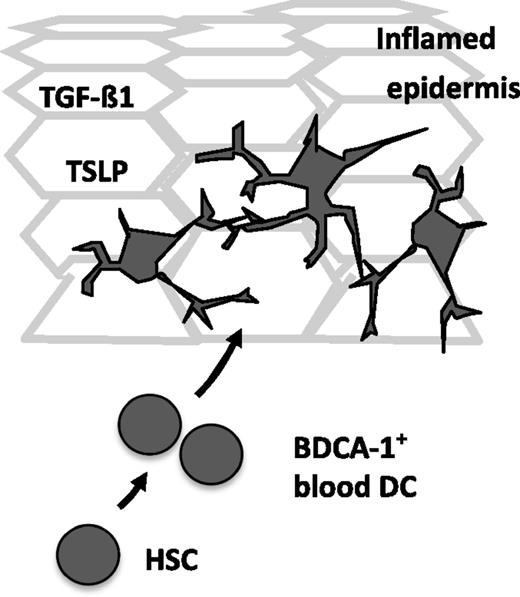
Hypothetical model of inflammatory LC differentiation. Epidermal keratinocytes express high levels of TSLP under inflammatory conditions. TGF-β1 is expressed by keratinocytes and was previously shown to promote LC differentiation. Martínez-Cingolani et al demonstrated that upon combined short-term stimulation with TSLP plus TGF-β1, human BDCA-1+ peripheral blood DCs acquire LC characteristics.1 They found that TSLP plus TGF-β1 synergistically promote LC differentiation from these cells. Whereas LCs undergo local proliferation in steady-state conditions, bone marrow–derived BDCA-1+ peripheral blood DCs may contribute to the pool of LCs during inflammation.
Hypothetical model of inflammatory LC differentiation. Epidermal keratinocytes express high levels of TSLP under inflammatory conditions. TGF-β1 is expressed by keratinocytes and was previously shown to promote LC differentiation. Martínez-Cingolani et al demonstrated that upon combined short-term stimulation with TSLP plus TGF-β1, human BDCA-1+ peripheral blood DCs acquire LC characteristics.1 They found that TSLP plus TGF-β1 synergistically promote LC differentiation from these cells. Whereas LCs undergo local proliferation in steady-state conditions, bone marrow–derived BDCA-1+ peripheral blood DCs may contribute to the pool of LCs during inflammation.
LCs were first identified in the late 19th century by Paul Langerhans as the nerve cells of the skin. Still today, most recently published hematopoiesis trees neglect DC family members such as LCs. This seems surprising considering it is long known that DCs are of hematopoietic origin. Moreover, LCs are regarded as prototypic DCs from peripheral tissues which historically served most critical in establishing the DC paradigm for the initiation of T-cell immune responses. Why is it then that LCs are often lacking from hematopoiesis trees? First, fundamental studies in mice recently abandoned LCs as close relatives of the DC family, and lifelong LC replenishment in adult individuals occurs independently of bone marrow hematopoiesis (reviewed in Malissen et al2 ). In fact, LC networks in transplanted human limbs are of donor origin even years after transplantiation.3 It was recently shown that the epidermal LC network is established prenatally from yolk sac precursors in a similar manner as shown for microglia and certain macrophage subsets.4 Second, despite common murine DC progenitors that have been identified, the exact origination of these cells from hematopoietic stem cells still remains unknown. Importantly, LCs undergo considerable turnover during skin inflammation and this increased demand is met at least partially by bone marrow–derived circulating blood precursor cells. In particular, cell sorting previously revealed that murine monocytes are capable of differentiating into LCs in vivo.5 Key questions remained unresolved: what are the intermediate stages of DC subset development from hematopoietic stem cells? What is the nature of the LC precursors in human peripheral blood potentially giving rise to LCs under inflammatory conditions? What are the inflammatory signals that may convert such a human blood–derived precursor into an LC?
Human peripheral blood contains monocyte subsets as well as minute populations of circulating DCs, among them myeloid cell–related BDCA-1+ (CD1c+) and BDCA-3+ DCs as well as plasmacytoid DCs (reviewed in Ziegler-Heitbrock et al6 ). Martínez-Cingolani et al1 demonstrated that BDCA-1+ peripheral blood DCs undergo rapid differentiation into LC-like DCs in response to the inflammatory factor TSLP in synergism with the previously identified LC differentiation stimulus transforming growth factor-β1 (TGF-β1).2 Other candidate DC precursor cell populations (including phenotypically similar cells isolated from tonsils, blood monocytes, BDCA-3+ blood DCs) lacked similar LC differentiation potential in response to TSLP plus TGF-β1 despite expressing functional TSLP receptor complexes. Moreover, higher percentages of LCs were present in cultures of BDCA-1+ DCs as compared with cultures of monocytes, even under conditions previously optimized for obtaining LC-like cells from monocytes (ie, granulocyte macrophage–colony-stimulating factor plus interleukin-4 and TGF-β1).7 TSLP was previously identified as a factor induced in lesional skin from atopic dermatitis/eczema patients.8 The critical novel point made by the current study was that TSLP synergizes with TGF-β1 for driving LC differentiation and that such a TSLP/TGF-β1–dependent LC precursor is included within the (potentially heterogenous) population of BDCA-1+ blood DCs (see figure). The authors elegantly identified TSLP as a potential LC differentiation factor when they initially performed microarray gene profiling of blood DCs stimulated with TSLP, leading to the identification of an LC signature. Based on these observations, they then added TSLP alone, or together with TGF-β1, to cultures of candidate LC precursors. The authors subsequently identified BDCA-1+ blood DCs as the main precursors capable of differentiating into LCs under these conditions. Indeed, the authors confirmed that these LCs are characterized by hallmark markers for LCs such as high levels of CD1a, Langerin (CD207), and CCR6, as well as the ultrastructural presence of numerous intracellular Birbeck granules and by the lack of other markers such as CD11b and CD209 (DC-Sign) affiliated with dermal/interstitial DCs and inflammatory dendritic epidermal cells (IDECs).
LCs represent a unique DC subset that performs long-lasting interactions with epithelial cells in the steady-state epidermis. Interestingly, TSLP-induced LCs lacked the expression of E-cadherin, typically expressed at high levels by LCs. During skin allergy or infection, TSLP is expressed at high levels by apical keratinocytes within the inflamed epidermis and is released by activated mast cells. TSLP might facilitate LC differentiation in inflamed skin and the lack of epithelial adhesion molecules might allow these cells to rapidly egress from the epidermis to skin-draining lymph nodes. The lineage relationship of these TSLP-induced LCs to other inflammatory DCs such as IDECs (reviewed in Segura and Amigorena9 ) remains to be analyzed. Moreover, alternative inflammatory signals might also lead to the generation of LCs. For example, the TGF-β family member Activin-A, induced by keratinocytes during inflammation and wound healing, promotes LC differentiation from human monocytes.10 The absence/low expression of these inflammatory signals in the steady-state epidermis may indicate that the factors inducing LC differentiation during inflammation or in the steady-state epidermis differ. LCs were functionally implicated in tolerance induction, skin inflammation, and cancer; therefore, deciphering these LC-inducing signals is of substantial clinical interest. Apart from providing in vitro models for the study of LCs, these findings might lead to the identification of novel molecular targets for pharmacologic interference with skin diseases. Moreover, knowledge of these LC-instructive factors and the nature of blood precursors of LCs might allow for the improved generation of LCs for cell therapy applications and for gaining novel insights into the pathogenesis of monocyte/DC/LC-related neoplasms.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal