Abstract
Purpose - Predicting outcome in patients with ALL has been traditionally based on pre-treatment characteristics such as age, white blood cell count (WBC) and cytogenetics. Minimal residual disease is a surrogate to the complex interaction of disease biology and therapy and its role in assigning risk is well-established. Many prior studies in patients with ALL have used molecular markers of MRD with few studies evaluating the role of multi-parameter flow cytometry (MFC) in the adult population.
We investigated the predictive value of MRD assessed by MFC among 340 patients with ALL treated between March 2004 and March 2014 using regimens including the hyperCVAD backbone.
Methods - Among 340 patients with B-ALL treated in this period 323 (95%) achieved complete remission (CR) or CR without platelet recovery (CRp) and were included in this study. Median age was 52 (Range, 15-84). Median WBC was 9.35 x109/L (Range, 0.4-658.1 x109/L). Cytogenetics were normal in 62 (18%), Philadelphia+ in 146 (43%), 11q23/rearranged MLL in 14 (4%), aneuploid in 45 (13%), hyperdiploid in 29 (9%), hypodiploid in 13 (4%), insufficient metaphases/ not done in 31 (9%). MRD by MFC was assessed with a sensitivity of 0.01%, using a 15-marker, 4-color panel in the first half of the study and subsequently a 6-color panel. Bone marrow specimens for MRD assessment were obtained at the time of achievement of CR and at approximately 3 month intervals thereafter.
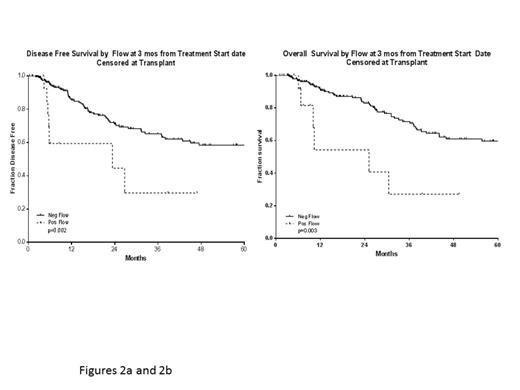
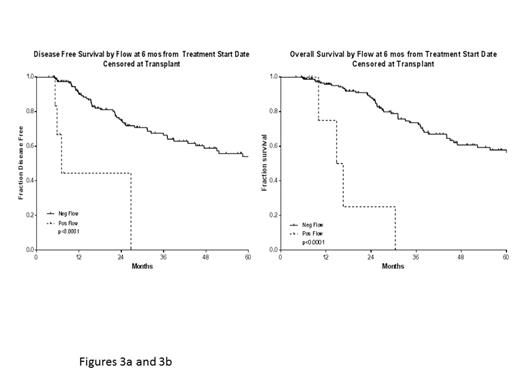
Results - 260 patients had available samples at CR and 166 (64%) became MRD negative. Achieving MRD negative status at CR was associated with a statistically significant improvement in disease-free survival (P =0.004) and overall survival (P=0.03). 215 patients were evaluated for MRD at approximately 3 months and 201 (93%) became negative. Achieving MRD negative status at approximately 3 months was also associated with a statistically significant improvement in DFS (P=0.002) and OS (P=0.003). 166 patients were evaluated for MRD at approximately 6 months and 160 (96%) became negative. Achieving MRD negative status at approximately 6 months was also associated with a statistically significant improvement in DFS (P<0.0001) and OS (P<0.0001). Figure below demonstrates the DFS and OS by MRD status at CR (Figure 1a and 1b), at 3 months (Figure 2a and 2b), and at 6 months (Figure 3a and 3b) with patients censored at the time of undergoing an allogeneic stem cell transplant or last follow-up. On multivariate analysis including age, WBC at presentation, cytogenetics (standard vs. high risk), and MRD status at CR, 3 months and 6 months, achieving an MRD negative status at CR was an independent predictor of DFS (P<0.05).
Conclusion – Achievement of an MRD negative state assessed by MFC is an important predictor of DFS and OS in patients with ALL
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal