To the editor:
Clonal hematopoiesis of indeterminate potential (CHIP) is an age-related condition in which somatic mutations associated with hematologic malignancy are found in the blood of individuals without recognized hematologic abnormalities.1-4 It is associated with malignant and nonmalignant outcomes, including death from cardiovascular disease and increased all-cause mortality.1,2 Because CHIP is asymptomatic, stem cells harboring myeloid driver mutations could be unknowingly transferred from donor to recipient during allogeneic hematopoietic stem cell transplantation (HSCT), the only curative therapy for many hematologic malignancies.
Here, we consider one of several potential implications of donor-engrafted CHIP, a phenomenon in which stem cells from donors with CHIP are directly transferred to recipients during transplantation. The current paradigm of risk for donor-engrafted CHIP centers on donor cell leukemia, a complication affecting 0.1% of transplant recipients, in which a new hematologic malignancy develops from donor-engrafted cells.5-8 Nonmalignant outcomes of donor CHIP, such as hematopoietic dysfunction, immunologic impairment, and cardiovascular disease, have not been considered. In fact, if donor-engrafted CHIP is similar to CHIP in native hematopoiesis, nonmalignant consequences may be more common than donor cell leukemia and may manifest earlier after transplantation, thereby contributing significantly to transplant-related morbidity. As a proof of concept, we asked whether some recipients with persistent unexplained cytopenias after transplantation received grafts from donors with CHIP clones that might impair hematopoietic function without causing rapid evolution of hematologic malignancy.
We evaluated 552 patients who underwent allogeneic HSCT for any cause at the Dana-Farber Cancer Institute (DFCI) between 1 January 2013 and 31 August 2016. All patients provided written consent according to protocols approved by the institutional review board at DFCI. Eighty-nine patients (16%) met the following inclusion criteria: (1) >95% donor hematopoietic chimerism, (2) at least 1 cytopenia (white blood cell count, <2 × 109/L; absolute neutrophil count, <1 × 109/L; hemoglobin, <12 g/dL; or platelets, <100 × 109/L) present in at least 2 consecutive evaluations after posttransplant day 100, and (3) bone marrow examination showing no evidence of relapsed malignancy. Of these patients, 93% (n = 83) had an identifiable cause of their cytopenia(s) (“explained”), whereas 7% (n = 6) had no identifiable cause (“unexplained”; supplemental Tables 1 and 2, available on the Blood Web site).
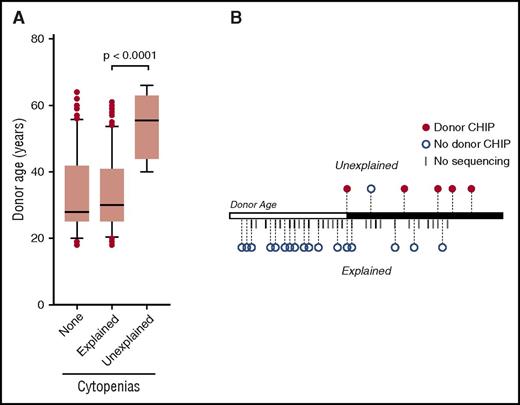
Donor age was significantly higher among recipients with unexplained cytopenias compared with those with explained cytopenias (median age, 55 vs 30 years; P < .0001; Figure 1A), whereas donor age was similar in recipients with explained cytopenias compared with those without cytopenias (median age, 30 vs 28 years; P = .98). There was no significant difference in stem cell mobilization efficiency between those donors whose recipients developed unexplained cytopenias compared with similar donors (age 40 years or older) whose recipients developed explained cytopenias (median, 4.5 × 106 vs 6.5 × 106 CD34+ cells/kg; P = .23). We therefore asked whether the association between unexplained cytopenias and older donor age was linked to CHIP in the donor stem cell product that was directly transmitted to the recipient during transplantation.
Age distribution of cytopenias and donor CHIP. (A) Donor age in HSCT recipients with >95% chimerism after day 100 based on the presence of persistent cytopenias with (explained) and without (unexplained) identified cause. Box limits indicate the 25th and 75th percentiles, whiskers extend to the 10th and 90th percentiles, and dots represent outliers. (B) Donor age distribution among patients with cytopenias. Donor age is plotted on a single axis, with the white portion representing age <40 years and the black portion representing age 40 years and older (overall range, 15-72 years). Patients who underwent next-generation sequencing as part of their evaluation are represented by circles (red, donor CHIP; blue, no donor CHIP). Patients who did not undergo sequencing are represented by hatch marks.
Age distribution of cytopenias and donor CHIP. (A) Donor age in HSCT recipients with >95% chimerism after day 100 based on the presence of persistent cytopenias with (explained) and without (unexplained) identified cause. Box limits indicate the 25th and 75th percentiles, whiskers extend to the 10th and 90th percentiles, and dots represent outliers. (B) Donor age distribution among patients with cytopenias. Donor age is plotted on a single axis, with the white portion representing age <40 years and the black portion representing age 40 years and older (overall range, 15-72 years). Patients who underwent next-generation sequencing as part of their evaluation are represented by circles (red, donor CHIP; blue, no donor CHIP). Patients who did not undergo sequencing are represented by hatch marks.
For all 6 recipients with unexplained cytopenias, we sequenced DNA prepared from whole bone marrow or peripheral blood using an amplicon-based panel targeting 95 genes recurrently mutated in hematologic malignancies.9 Five of 6 recipients harbored mutations in DNMT3A, and in all 5 cases we confirmed donor origin of mutations by sequencing DNA prepared from archived donor stem cell products consisting of granulocyte colony-stimulating factor–mobilized peripheral blood (Table 1). In contrast, 24 of 83 patients (29%) with explained cytopenias underwent clinical next-generation sequencing as part of their evaluation, and sequencing was negative in all cases (Figure 1B). These findings are consistent with the association of CHIP with older age in nondonor cohorts, and show that CHIP is present in stem cell donors despite rigorous health screening and can engraft in recipients.
Characteristics of patients with donor-engrafted HSC clones
| Recipient . | Donor source . | Age at HSCT, y . | Donor age, y* . | Donor-engrafted mutation . | Time of detection, mo . | Donor VAF, %† . | VAF at detection, %‡ . | Clonal evolution . | Additional mutation(s) . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | MUD | 57 | 40 | DNMT3A T862N | 18 | 5.9 | 4.4 | Yes | ASXL1, TP53 |
| 2 | MRD | 67 | 59 | DNMT3A Q356X | 13 | 1.6 | 4.0 | No | None |
| 3 | MRD | 51 | 53 | DNMT3A R882H | 4 | 2.6 | 2.6 | No | None |
| 4 | MRD | 68 | 66 | DNMT3A S786X | 6 | 1.5 | 3.7 | No | None |
| 5 | MRD | 63 | 62 | DNMT3A R729Q | 30 | 6.4 | 11.1 | No | None |
| Recipient . | Donor source . | Age at HSCT, y . | Donor age, y* . | Donor-engrafted mutation . | Time of detection, mo . | Donor VAF, %† . | VAF at detection, %‡ . | Clonal evolution . | Additional mutation(s) . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | MUD | 57 | 40 | DNMT3A T862N | 18 | 5.9 | 4.4 | Yes | ASXL1, TP53 |
| 2 | MRD | 67 | 59 | DNMT3A Q356X | 13 | 1.6 | 4.0 | No | None |
| 3 | MRD | 51 | 53 | DNMT3A R882H | 4 | 2.6 | 2.6 | No | None |
| 4 | MRD | 68 | 66 | DNMT3A S786X | 6 | 1.5 | 3.7 | No | None |
| 5 | MRD | 63 | 62 | DNMT3A R729Q | 30 | 6.4 | 11.1 | No | None |
HSC, hematopoietic stem cell; MRD, matched related donor; MUD, matched unrelated donor; VAF, variant allele fraction.
Age of donor at time of HSCT.
VAF of the indicated mutation in donor product collected at the time of HSCT.
VAF of the indicated mutation at the time of detection in the recipient blood or bone marrow after HSCT.
CHIP is associated with an elevated relative risk of progression to hematologic malignancy, but the absolute annual risk of progression is low. During myeloid leukemogenesis, clinical progression is linked to clonal expansion and evolution.10-12 We therefore hypothesized that donor CHIP can engraft in recipients without undergoing rapid clonal expansion or evolution. To test this hypothesis, we evaluated the dynamics of clonal engraftment in 4 cases by sequencing peripheral blood at regular intervals after transplantation (range 3-12 samples over 1-3 years). We observed that donor-engrafted CHIP was detectable at all early time points (range of first assessment, 44-109 days) and that none of the donor-engrafted clones showed evidence of genetic evolution within the first year. In 3 recipients, the overall donor-engrafted clone size remained stable throughout the duration of study. In a fourth recipient, we saw eventual development of 2 additional driver mutations (TP53 and ASXL1) that were not present in the stem cell product. Concomitant with this genetic progression, the overall DNMT3A clone size expanded from a variant allele fraction of 8.6% to 29.8%, but without evidence of clinical or morphological progression (supplemental Figure 1). These data suggest that transfer of readily detectable CHIP clones from hematopoietically competent donors may cause clinically significant impairment of graft function without driving rapid leukemic transformation in transplant recipients.
Taken together, our results show that CHIP occurs in HSCT donors, engrafts in recipients, and can expand and undergo clonal genetic evolution after transplantation without causing rapid development of hematologic malignancy. The striking enrichment of donor-engrafted CHIP in patients with unexplained cytopenias after HSCT suggests that donor CHIP may be associated with graft dysfunction even at early time points. Our findings highlight the consistencies between CHIP in native and transplant hematopoiesis and challenge our current conception of the prevalence and potential risks posed by donor-engrafted CHIP. Several outstanding questions remain.
What is the frequency of CHIP in the transplant donor population? Even focusing on a well-defined subset of recipients, our results suggest that CHIP may be substantially more common than expected among older stem cell donors. Although initial reports showed that CHIP is rare in healthy individuals under 50 years of age, more sensitive sequencing technology can detect small CHIP clones (0.1%-2%), showing that CHIP is more prevalent and affects younger individuals than previously recognized.13 Moreover, stem cell enrichment strategies such as growth factor mobilization or direct bone marrow harvest may modify the apparent frequency or biological consequences of CHIP in stem cell donors.
Which donors are most at risk? Previous studies have shown that advancing donor age is associated with inferior outcomes in HSCT recipients.14 We hypothesize that this association is driven primarily by the subset of older donors with CHIP; indeed, in the 5 cases of donor-engrafted CHIP reported here, all donors were 40 years or older at the time of transplantation. The presence of CHIP may thus be an age-independent predictor of donor hematopoietic fitness, enabling exclusion of “at-risk” donors while exonerating older donors without CHIP and ensuring that viable donors are not unnecessarily excluded as candidates.
What is the spectrum of clinical implications of donor-engrafted CHIP in transplant recipients? Outcomes associated with CHIP have been elucidated in distinct populations, including healthy individuals and patients with cancer receiving cytotoxic therapy.15-17 The enrichment of donor-engrafted CHIP among HSCT recipients with unexplained cytopenias suggests a possible causal association with impaired graft function, and raises the possibility that other transplant-specific manifestations of CHIP may not yet be identified. For example, Tet2-deficient clonal hematopoiesis has recently been directly linked to derangements in inflammatory cytokine expression, macrophage function, and innate immune trafficking.18 As such, the spectrum of consequences associated with donor-engrafted CHIP in HSCT recipients could be broad, including impairment of graft function or alteration of immune function resulting in an increased risk of infection, graft-versus-host disease, or relapse.
In summary, our findings suggest a new paradigm of donor-attributable risk in allogeneic HSCT. We propose that a thorough understanding of the frequency of CHIP in the donor population and its impact on transplantation outcomes could have significant implications on clinical decision-making. However, a comprehensive evaluation of the frequency of donor CHIP and its impact on HSCT outcomes is required before deployment of systematic screening in clinical practice.
The online version of this article contains a data supplement.
Authorship
Acknowledgments: The authors thank the Connell O’Reilly Cell Manipulation Facility and the Ted and Eileen Pasquarello Tissue Bank for provision of samples. The authors thank John Dick for provision of resources and materials for Droplet Digital polymerase chain reaction validation.
This work was supported by grants from the National Institutes of Health (National Cancer Institute [NCI] K08 CA204734 [R.C.L.], National Heart, Lung, and Blood Institute 5T32HL116324 [C.J.G.], NCI R01CA183559 [R.S. and J.R.], NCI R01CA183560 [J.R. and R.S.], and NCI 5P01CA14106 [R.S., J.H.A. and J.R.]), the Marie Lundin Cancer Research Trust (R.C.L.), and the Jock and Bunny Adams Research and Education Endowment (J.H.A.).
Contribution: C.J.G. designed the research, performed research, analyzed data, and wrote the paper; J.A.K. performed research, analyzed data, and edited the paper; F.C.K. analyzed data and edited the paper; V.H. contributed patient samples, provided access to data, contributed to study design, and edited the paper; S.N., E.P.A., J.R., R.S., and J.H.A. contributed patient samples, contributed to study design, and edited the paper; and R.C.L. designed the research, performed research, analyzed data, and edited the paper.
Conflict-of-interest disclosure: S.N. reports consulting for Kite Pharma and travel funded by Celyad, SA. V.H. reports consulting for Jazz Pharmaceuticals. J.R. reports consulting for Biothera, Novartis, Biogen Idec, Delinia, Clarus Ventures, Amgen, Draper Laboratories, and RA Capital. R.C.L. reports consulting for Takeda Pharmaceuticals and research funding from MedImmune. The remaining authors declare no competing financial interests.
Correspondence: R. Coleman Lindsley, Dana-Farber Cancer Institute, 450 Brookline Ave, D-2058, Boston, MA 02115; e-mail: coleman_lindsley@dfci.harvard.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal