Genetic studies have been early introduced for the classification of acute myeloid leukemia (AML), but specific molecular lesions [e.g., t(8;21), inv(16), t(15;17)] define only a fraction of patients. In the genomic era, many mutations and cytogenetic abnormalities and their combinations have been described in AML; their diversity contributes to the heterogeneity of pathomorphologic presentations. While certain mutations are restricted to individual classical morphologic subtypes, pathognomonic lesions are difficult to find. Therefore, to date, molecular mutations or cytogenetic abnormalities have been used to assess prognosis rather than define disease sub-entities according to molecular pathogenesis, likely a future standard in AML diagnosis.
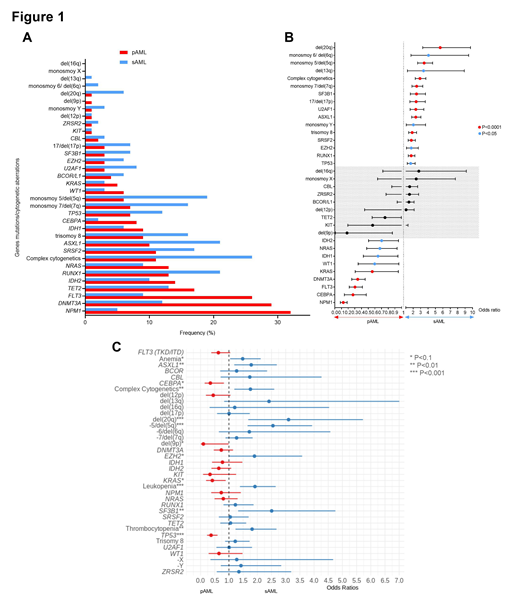
Balanced translocations are prototypic founder lesions, however, founder somatic vs. subclonal mutations have not been used to define subtypes of AML. Molecular classification may better reflect the pathogenesis of AML than morphologic/clinical subtypes e.g., secondary (sAML) vs. primary AML (pAML) or AML with normal (ncAML) vs. abnormal cytogenetics (acAML). This work describes the results of a large and comprehensive analysis of genomic landscape and cytogenetics in AML. Initially, 6788 cases were analyzed, including 4867 from our institutions (Cleveland Clinic Foundation and Munich Leukemia Laboratory, n=4862) fortified by publically deposited cases (n=1926) to define gene signatures and succession of mutations distinguishing pAML vs. sAML. While data for core-binding factor AML, MLL gene rearrangement leukemia, acute promyelocytic leukemia and therapy-related AML have also been analyzed (n=1094), we focused on remaining sAML (n=876) vs. pAML (n=4808) and within these entities (ncsAML, n=367; acsAML, n=509 vs. ncpAML, n=2856 and acpAML, n=1952). Although, sAML and pAML showed usual clinical differences, a reliable diagnostic algorithm could not be constructed using supervised analytic approaches and thus we aimed at identification of molecular biomarkers with prognostic and diagnostic value. Abnormal cytogenetics were present in 57% of AML including complex: 13%, +8; 11%: -5/del(5q): 8%; and -7del7q: 8%. Deep NGS for the 25 top mutated genes was applied and correlated with clinical and cytogenetic parameters (Fig.1A-B). We then defined/compared mutational landscape in acAML and ncAML separately. AcsAML showed more complex karyotypes (58% vs. 40% in acpAML, P<.0001). Similarly, acpAML patients had increased percentages of DNMT3A (18% vs. 11%, P=.007), FLT3 (17% vs. 8%, P=.0002), NPM1 (10% vs. 4%, P=.004), KRAS (7% vs. 3%, P=.01), with less frequent hits in ASXL1 (13% vs. 21%, P=.001) and SF3B1 (3.5% vs. 7%, P=.01) as compared to acsAML. Mutations significantly enriched in ncpAML vs. ncsAML involved: DNMT3A (37% vs. 14%, P<.0001), TET2 (18% vs. 11%, P=.01), CEBPA (10% vs. 3%, P=.004). Less enriched in pAML were mutations in ASXL1, RUNX1, SF3B1, SRSF2, and U2AF1. Logistic regression analysis showed various distinctive features between sAML and pAML (Fig.1C). Using a modified PyClone pipeline, we also recapitulated clonal hierarchy of ncAML to identify founder molecular events restricted to ncpAML vs. ncsAML. Indeed, founder lesions were differently distributed: DNMT3A (23% vs. 8%, P=.0003) and TET2 (9% vs. 3%, P=.02) mutations occurred more in ncpAML, while U2AF1 (0.5% vs. 6%, P<.0001), SRSF2 (2% vs. 7%, P=.01) and STAG2 (5% vs. 13%, P=.001) in ncsAML. Secondary hits/combinations were not random; e.g, DNMT3A and NPM1 were the most common in ncpAML (vs. ncsAML: 28% vs. 7%, P<.0001 and 11% vs. 4%, P=0.02) while ASXL1 (16% vs. 3%, P<.0001), SRSF2 (14% vs. 4%, P<.0001) and RUNX1 (10% vs. 4%, P=0.02) in ncsAML. Unique clonal succession patterns were proven to affect survival; e.g., ancestral DNMT3A hits showed worse OS compared to secondary/subclonal DNMT3A lesions (median: 13.3 vs. 20.1 months, P=.04).
Using combined data sets of mutations and cytogenetic abnormalities and clinical parameters, we then constructed supervised and unsupervised analyses to identify signatures of pAML vs. sAML: discordant cases between the molecular and the classic diagnostic assignment of sAML vs. pAML were investigated and a novel molecular classification irrespective of the pAML and sAML derivation has been created to include founder and secondary mutations combinations and concordance of the outcomes.
Advani:Abbvie: Research Funding; Kite Pharmaceuticals: Consultancy; Amgen: Research Funding; Pfizer: Honoraria, Research Funding; Macrogenics: Research Funding; Glycomimetics: Consultancy, Research Funding. Meggendorfer:MLL Munich Leukemia Laboratory: Employment. Nazha:Daiichi Sankyo: Consultancy; Tolero, Karyopharma: Honoraria; MEI: Other: Data monitoring Committee; Incyte: Speakers Bureau; Abbvie: Consultancy; Novartis: Speakers Bureau; Jazz Pharmacutical: Research Funding. Sekeres:Millenium: Membership on an entity's Board of Directors or advisory committees; Syros: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees. Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Maciejewski:Alexion: Consultancy; Novartis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal