TO THE EDITOR:
Anti–platelet factor 4 (PF4) antibodies have a central role in the pathophysiology of thrombosis and thrombocytopenia in heparin-induced thrombocytopenia (HIT)1,2 and vaccine-induced immune thrombotic thrombocytopenia (VITT).3-7 Here, we present the case of a patient with recurrent thrombosis and thrombocytopenia, secondary to a persistent anti-PF4/polyanion monoclonal antibody due to an underlying neoplastic condition, which we refer to as monoclonal gammopathy of thrombotic/thrombocytopenic significance (MGTS). The implications of these findings for the investigation of unexplained thrombophilia are discussed.
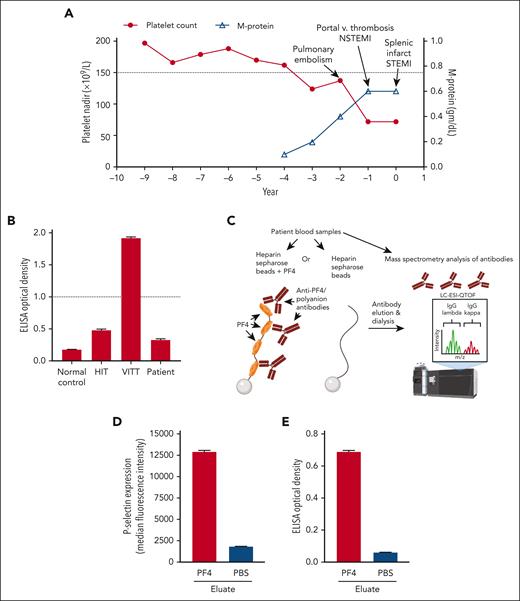
A 64-year-old man presented for evaluation of recurrent thrombotic episodes. His medical history included segmental and subsegmental pulmonary emboli, portal vein thrombosis, non-ST elevation myocardial infarction, splenic infarction, and ST elevation myocardial infarction (Figure 1A). Extensive investigations performed did not support a thrombophilia diagnosis (supplemental Table 1 and supplemental Materials; available on the Blood website). His platelet counts were noted to be frequently decreased during these hospitalizations (<150 × 109/L; Figure 1A). He had a history of thrombosis in the absence of heparin administration, breakthrough thrombosis even while on anticoagulation (apixaban/warfarin), as well as adverse reactions to heparin on occasions when it was used, as noted in supplemental Materials. Investigation for HIT revealed positive PF4/polyanion HIT enzyme-linked immunosorbent assay (ELISA) (1.983 optical density) and serotonin release assay (SRA) (95% serotonin release).
Trending of laboratory variables and affinity purification of the anti-PF4/polyanion antibody. (A) Nadir platelet count (closed circles) and peak serum monoclonal protein (M-protein) levels (open triangles) for each year of clinical data prior to and including the year of presentation to Mayo Clinic are shown on the left and right y-axes, respectively. The lower limit of the normal platelet reference range is depicted by a dotted line (150 × 109/L). (B) HIT, VITT (Ad26.COV2.S-associated), normal control, and patient samples were run in an uncomplexed PF4 (VITT) ELISA. The dotted line represents the positive cutoff of the assay. (C) Experimental scheme for affinity purification of anti-PF4/polyanion antibodies is shown. (D-E) Eluates from PF4/heparin or phosphate-buffered saline (PBS)/control beads were evaluated for their ability to activate PF4-treated platelets (D) and bind PF4/polyanion targets (E). Mean and 1 SD of triplicate measurements are presented in (B), (D), and (E), and (A) presents single measurements of nadir platelet counts and M-protein level. m/z, mass-to-charge ratio; STEMI; ST elevation myocardial infarction; NSTEMI, non-ST elevation myocardial infarction.
Trending of laboratory variables and affinity purification of the anti-PF4/polyanion antibody. (A) Nadir platelet count (closed circles) and peak serum monoclonal protein (M-protein) levels (open triangles) for each year of clinical data prior to and including the year of presentation to Mayo Clinic are shown on the left and right y-axes, respectively. The lower limit of the normal platelet reference range is depicted by a dotted line (150 × 109/L). (B) HIT, VITT (Ad26.COV2.S-associated), normal control, and patient samples were run in an uncomplexed PF4 (VITT) ELISA. The dotted line represents the positive cutoff of the assay. (C) Experimental scheme for affinity purification of anti-PF4/polyanion antibodies is shown. (D-E) Eluates from PF4/heparin or phosphate-buffered saline (PBS)/control beads were evaluated for their ability to activate PF4-treated platelets (D) and bind PF4/polyanion targets (E). Mean and 1 SD of triplicate measurements are presented in (B), (D), and (E), and (A) presents single measurements of nadir platelet counts and M-protein level. m/z, mass-to-charge ratio; STEMI; ST elevation myocardial infarction; NSTEMI, non-ST elevation myocardial infarction.
Platelet counts were available for almost a decade prior to presentation, and nadir counts were above the lower limit of the normal reference range until ∼4 years prior to presentation (Figure 1A). Periodic infusions of intravenous immunoglobulin were associated with transient increases in platelet counts (supplemental Figure 1). One of the intravenous immunoglobulin infusions was used in the setting of splenic infarction, and others were administered due to concern for thrombosis in the setting of worsening thrombocytopenia. Four years prior, he was noted to have an immunoglobulin G (IgG) κ monoclonal gammopathy of undetermined significance (MGUS, 0.1 g/dL) during evaluation for back pain. Monoclonal protein (M-protein) MGUS levels showed a gradual but significant increase from 0.1 g/dL to 0.6 g/dL during the 4-year period. No clonal plasma/B-cell populations were identified on bone marrow biopsy. A positron emission tomography scan did not show any evidence of malignancy or bone lesions indicative of multiple myeloma. Numerous HIT ELISA and SRAs obtained in the 2 years prior to presentation showed consistent positivity in both assays (ELISA: mean 2.12 optical density, standard deviation [SD] [0.25], n = 16; SRA: mean 95% [8%], n = 11). Patient antibodies, like HIT antibodies, did not recognize uncomplexed PF4 in a recently developed VITT-specific ELISA8 (Figure 1B). Based on this picture, we hypothesized that the MGUS antibody had PF4/polyanion specificity and an evaluation of the anti-PF4 antibody was undertaken.
Anti-PF4/polyanion antibodies were affinity purified from the patient sample using PF4-treated heparin Sepharose beads (as described in the supplemental Materials) and evaluated by liquid chromatography electrospray ionization quadrupole time-of-flight mass spectrometry (LC-ESI-QTOF MS; Figure 1C). Eluates from the PF4-heparin beads activated platelets (Figure 1D) and recognized PF4/polyanion targets in ELISA (Figure 1E), while eluates from control beads (heparin Sepharose beads not treated with PF4) did not. Immunofixation electrophoresis was performed on the native sample to confirm the presence of an IgG κ monoclonal antibody (supplemental Figure 2), and testing on eluates revealed a similarly migrating restricted monoclonal IgG κ band in PF4-heparin eluates but not control eluates (supplemental Figure 3).
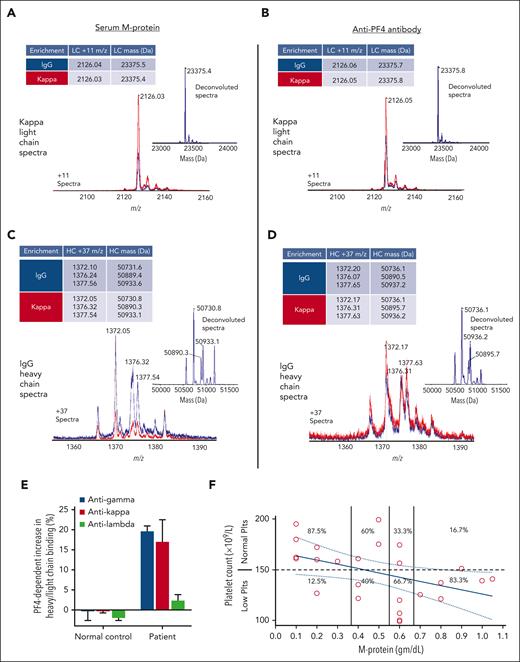
LC-ESI-QTOF MS performed on the native serum and isolated anti-PF4/polyanion antibodies demonstrated near-identical mass between the κ light chain of the M-protein in serum (MGUS; Figure 2A) and the monoclonal anti-PF4/polyanion antibody in PF4-heparin bead eluates (Figure 2B; eg, 2126.03 vs 2126.05 and 23 375.4 vs 23 375.8). No λ light chains were seen. Similarly, glycosylated IgG heavy chains were highly similar in mass between the MGUS (Figure 2C) and the monoclonal anti-PF4/polyanion antibody (Figure 2D). Eluates from control beads did not reveal any antibody, arguing against nonspecific binding of the patient’s MGUS antibody to heparin-Sepharose beads (supplemental Figure 4), and a monoclonal antibody from a different patient with multiple myeloma undergoing therapy (with an M-protein level of 0.4 g/dL) was not affinity purified by these techniques (supplemental Figure 5B). Consistent with these findings, γ heavy chain and κ light chain, but not λ light chain, showed significant increase in PF4-dependent binding to normal donor platelets (Figure 2E).
M-protein and monoclonal anti-PF4/polyanion antibody light and heavy chains have identical mass spectrometry profiles. (A) Displayed are LC-ESI-QTOF MS light chain (LC) +11 (m/z) distributions of serum proteins and (B) anti-PF4/polyanion antibodies isolated from the patient’s serum using PF4-treated heparin Sepharose beads, as described. In the spectra, red represents the +11 m/z distribution of all κ containing immunoglobulins, and blue represents the +11 m/z LC distribution of κ chains associated with an IgG heavy chain (HC). The number above each peak indicates the identified chain’s +11 m/z ratio. The x-axis depicts m/z ratios, and the height of the peak shows the identified antibodies’ relative abundance. Each subpanel contains an inset depicting the deconvoluted spectra with the molecular mass of the identified immunoglobulin LC and a table summarizing the major LC m/z values and deconvoluted masses. Similar to (A) and (B), (C) and (D) display the +37 m/z HC distribution and deconvoluted spectra for the immunoglobulin γ (G) HC spectra from MGTS patient serum and anti-PF4 antibody enriched eluate, respectively. The various peaks in (C) and (D) depict differentially glycosylated forms of the HC immunoglobulin. (E) PF4-dependent binding of patient IgG HC (γ) and κ/λ LCs to normal donor platelets were evaluated. Mean and 1 SD of triplicate measurements are presented. (F) Platelet counts (y-axis) were correlated with M-protein levels (x-axis). M-protein intervals were qualitatively grouped into 4 intervals and the percentage of normal (≥150 × 109/L) and low (<150 × 109/L) platelet counts are displayed for each interval. M-protein and platelet count represented by each data point were obtained on the same day of testing, except on 2 occasions when they were drawn within 48 hours of each other.
M-protein and monoclonal anti-PF4/polyanion antibody light and heavy chains have identical mass spectrometry profiles. (A) Displayed are LC-ESI-QTOF MS light chain (LC) +11 (m/z) distributions of serum proteins and (B) anti-PF4/polyanion antibodies isolated from the patient’s serum using PF4-treated heparin Sepharose beads, as described. In the spectra, red represents the +11 m/z distribution of all κ containing immunoglobulins, and blue represents the +11 m/z LC distribution of κ chains associated with an IgG heavy chain (HC). The number above each peak indicates the identified chain’s +11 m/z ratio. The x-axis depicts m/z ratios, and the height of the peak shows the identified antibodies’ relative abundance. Each subpanel contains an inset depicting the deconvoluted spectra with the molecular mass of the identified immunoglobulin LC and a table summarizing the major LC m/z values and deconvoluted masses. Similar to (A) and (B), (C) and (D) display the +37 m/z HC distribution and deconvoluted spectra for the immunoglobulin γ (G) HC spectra from MGTS patient serum and anti-PF4 antibody enriched eluate, respectively. The various peaks in (C) and (D) depict differentially glycosylated forms of the HC immunoglobulin. (E) PF4-dependent binding of patient IgG HC (γ) and κ/λ LCs to normal donor platelets were evaluated. Mean and 1 SD of triplicate measurements are presented. (F) Platelet counts (y-axis) were correlated with M-protein levels (x-axis). M-protein intervals were qualitatively grouped into 4 intervals and the percentage of normal (≥150 × 109/L) and low (<150 × 109/L) platelet counts are displayed for each interval. M-protein and platelet count represented by each data point were obtained on the same day of testing, except on 2 occasions when they were drawn within 48 hours of each other.
Treatment with rituximab was first pursued (375 mg/m2 × 4 doses) and was not associated with a significant change in platelet count, M-protein level (supplemental Figure 6A), or HIT ELISA and SRA results (supplemental Figure 6B). The patient was treated several months later with daratumumab (1800 mg) and dexamethasone (8 mg) with a schedule of 4 weekly infusions followed by 3 infusions at 2-week intervals. A subtle decrease in HIT ELISA (Supplemental Figure 7A) and PF4-dependent p-selectin expression assay titers (supplemental Figure 7B) was noted, which rebounded. Two platelet counts obtained during treatment were transiently above 150 × 109/L (supplemental Figure 7C). During treatment, M-protein levels decreased from a pretreatment level of 1.05 g/dL to a nadir of 0.7 g/dL and gradually rose to 0.8 g/dL in the posttreatment period (supplemental Figure 7C). M-protein and platelet counts obtained over the prior 5 years were compared (Figure 2F). The likelihood of observing a normal platelet count (>150 × 109/L) decreased from 88% to 60%, 33%, and 17% at MGUS levels of <0.4 g/dL, 0.4 to 0.5 g/dL, 0.6 g/dL, and >0.6 g/dL, respectively (Figure 2F). Five months after the last daratumumab infusion, anti-PF4/polyanion antibodies demonstrated a subtle increase in strength in both HIT ELISA (supplemental Figure 8A), and PF4-dependent p-selectin expression assay (supplemental Figure 8B) testing and was associated with a platelet count of 130 × 109/L and SRA result of 100%.
We describe a patient with recurrent thrombosis and thrombocytopenia due to a monoclonal anti-PF4/polyanion “HIT-like” antibody, which to the best of our knowledge is the first such conclusive case reported. In 1 prior report published as a conference abstract, a 62-year-old man with a monoclonal IgG κ antibody and a history of chronic thrombocytopenia presented with thrombosis after treatment with unfractionated heparin.9 In a second report, a “VITT-like” antibody that was HIT ELISA-positive and activated PF4-treated, but not heparin-treated platelets (and thus, VITT-like), was described in a patient with recurrent thrombosis and thrombocytopenia.10 The authors stated that “κ-light chain IgG monoclonal band (equal to paraprotein) strongly cross-reacted with immobilized PF4/heparin complexes in an ELISA (optical density >2.0)”; however, no data were shown, and this “VITT-like” antibody was not characterized further.10
Increased risk of arterial and venous thrombosis in MGUS has been described even with low levels of MGUS proteins,11-13 and thrombosis associated with thrombocytopenia can be the presenting symptom/sign of MGUS.14 Here, we leveraged recent technological advances in the use of mass spectrometry for the study of multiple myeloma15-18 and VITT19 and provide strong evidence that the MGUS antibody and anti-PF4/polyanion antibody in our patient are synonymous. Consistent with the antibody having different characteristics relative to VITT, the patient received an adenoviral vector-based COVID-19 vaccine (Ad26.COV2.S) followed by 2 mRNA vaccine boosters (BNT162b2) without any adverse effects. Additional studies to confirm the pathogenesis of this antibody in a murine HIT model20 are indicated. Although the patient has not had breakthrough thrombosis for ∼1.5 years since commencing dual anticoagulant and antiplatelet therapy with apixaban and clopidogrel, continued strong positivity in HIT ELISA and platelet functional testing poses a high thrombotic risk. Review of the patient’s history of M-protein levels suggests a “threshold effect” at around 0.4 g/dL, greater than which platelet counts are more likely to decrease into the thrombocytopenic range and thrombosis risk increases. Thus, one approach may be to institute a disease management strategy using plasma cell-directed therapies until a 0.4 g/dL M-protein level is attained. Additional plasma cell-directed therapies such as bortezomib are being considered. Lenalidomide, with its associated thrombotic risk,21 may be less appropriate in this setting. The phenomenon described here could explain the pathogenesis of thrombosis in some patients with an MGUS/myeloma diagnosis. Thus, findings consistent with recurrent thrombosis associated with thrombocytopenia in the setting of a monoclonal antibody should prompt investigation for a monoclonal anti-PF4 antibody/MGTS.
Acknowledgments
This work was supported, in part, by National Institutes of Health, National Heart, Lung, and Blood Institute grants HL158932 (A.P.), HL148120 (R.W.), and HL130724 (D.W.); and a Mayo Clinic intramural grant from the Advanced Diagnostic Laboratory (A.P.).
Authorship
Contribution: A.P., J.K.S., M.S., and D.M. conceived the study; A.P. and D.M. defined the experimental plan; A.J.K., N.P.S., M.C.K., B.S., S.B.D., and E.E.M. performed research studies; N.P.S. and E.E.M. assisted with data collection and confirmation; M.A.H., M.S., and S.K. provided clinical correlates and input; R.W. and D.W. provided helpful research input/critique; A.J.K., N.P.S., J.K.S., M.S., D.M., and A.P. authored the first draft of the manuscript and figures; and all authors provided input and approved the final version.
Conflict-of-interest disclosure: A.P. reports pending/issued patents (Mayo Clinic, Retham Technologies, and Versiti Blood Center of Wisconsin), equity ownership in and serving as an officer of Retham Technologies, and member of the advisory board of Veralox Therapeutics. D.M. has pending/issued patents (Dow Corning, Eastman Kodak, and Mayo Clinic) and is an inventor of the “Mass-Fix” mass spectrometry-based assay for the detection of monoclonal gammopathy. The remaining authors declare no competing financial interests.
Correspondence: Anand Padmanabhan, Department of Laboratory Medicine and Pathology, Mayo Clinic, 200 1st St SW, Rochester, MN 55905; e-mail: padmanabhan.anand@mayo.edu; and David Murray, Department of Laboratory Medicine and Pathology, Mayo Clinic, 200 1st St SW, Rochester, MN 55905; e-mail: murray.david@mayo.edu.
References
Author notes
∗A.J.K., J.K.S., and M.S. contributed equally to this study.
Data will be made available upon reasonable request to corresponding author.
The online version of this article contains a data supplement.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal