We recently demonstrated that plasma lipoproteins play a major role in regulating the function of the hemostatic system by either inhibiting or promoting the self-association of von Willebrand factor (VWF) into large fibers and bundles that are hyperadhesive for platelets. Such fibers can form on the surface of activated endothelium such as during thrombotic microangiopathies. We showed that high-density lipoprotein (HDL) attenuates VWF self-association and reduces the formation of VWF-platelet thrombi, both in vitro and in mice (PMID:26552698). By contrast, low-density lipoprotein (LDL) enhances VWF self-association and promotes the formation of VWF-platelet thrombi ( Blood, in press). Consequently, wild-type mice with elevated plasma LDL display intense and prolonged VWF-platelet thrombosis in stimulated mesenteric microvessels, exceeding even the thrombosis observed in ADAMTS13-deficient mice with normal LDL levels. All the lipoproteins of low density carry apolipoprotein (apo) B100 and comprise fractions of very low density (VLDL), intermediate density (IDL), and low density (LDL). The LDL fraction comprises two subfractions: small-dense (sd) LDL and large-buoyant (lb) LDL. Epidemiologic studies suggest that sd-LDL is the most atherogenic subfraction (PMID:33586462). Another atherogenic lipoprotein also carries apoB-100, Lp(a), in which the apoB-100 is complexed with apo(a). Here, we sought to determine the effect of LDL subfraction(s) on VWF self-association. We isolated LDL, sd-LDL and lb-LDL from healthy donor plasma by sequential KBr density centrifugation. Lp(a) was purified from patients with high circulating Lp(a) (>50 mg/dL) as described by Mueller et al. (PMID:35650291).
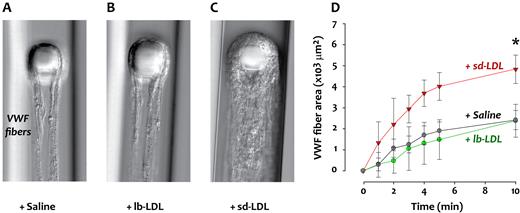
We first tested these lipoproteins in microfluidic devices adapted from the design of Herbig and Diamond (PMID:26178390). In these devices, high shear stress and flow acceleration are generated around a 30-um-wide pillar within a 60-um-wide flow channel and induce the attachment and self-association of VWF into fibers on and around the pillar. We quantified VWF fiber accumulation from differential interference contrast (DIC) images. Of all the lipoprotein fractions, sd-LDL was the most potent in accelerating VWF strand accumulation (see figure). The effect of lipoproteins in this device correlated with their impact on microvascular thrombosis in vivo. We infused apoB100-containing lipoproteins into wild-type mice (3-4 weeks old) before inducing VWF-platelet thrombi deposition in the mesenteric microvasculature with ionophore. All the apoB100 lipoproteins enhanced microvascular thrombosis [we did not test Lp(a), which had no effect in the microfluidic channel], but sd-LDL was by far the most potent; the treated mice had twice the number of large thrombi (>30-um diameter) as the mice treated with an equivalent quantity of lb-LDL. The effect also persisted for much longer before returning to baseline with the sd-LDL. We have explored possible reasons why sd-LDL is so much more potent. Compared to the other apoB-containing lipoproteins, sd-LDL is smaller and denser, with a greater surface curvature. Whether this fact changes accessibility to sites on apoB100 is not known. We also compared the lipidomes and proteomes of sd-LDL and lb-LDL for clues to the difference. Compared to lb-LDL, sd-LDL contained a much higher content of cholesterol and cholesterol esters per particle. The proteomes of the two particles were also different, with several proteins being more abundant in lb-LDL, in particular apoC-III, apoE, apoA-IV, and apoC-II. Only apoF was significantly more abundant in sd-LDL. We are currently testing to determine if any of these difference accounts for the differences between the two LDL subfractions in promoting VWF self-association.
In summary, we show that the lipoprotein associated with the greatest atherosclerotic burden and most cardiovascular disease is also the one with the most potent effect in promoting a prothrombotic state by enhancing VWF self-association. These findings have important implications for the development of the atherosclerotic lesion, the formation of the thrombus after the lesion ruptures, and for the microvascular dysfunction often observed after revascularization.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal