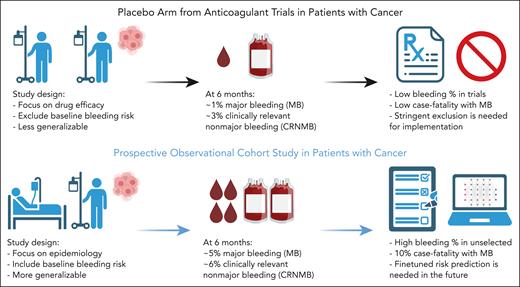
In this issue of Blood, Englisch et al have identified that ambulatory patients with cancers who are receiving systemic therapy are at high risk of clinically relevant bleeding (CRB).1 In this prospective observational cohort study conducted at the Medical University of Vienna, Austria, the authors have reported a 10% cumulative incidence of CRB at 6 months (including 5% major bleeding [MB] and 6% clinically relevant nonmajor bleeding [CRNMB]) in a group of 791 patients with predominantly solid tumors, regardless of baseline anticoagulation or antiplatelet. Notably, this estimate is significantly higher than the 3% to 4% pooled CRB incidence in the placebo arm of primary thromboprophylaxis clinical trials (1%-2% MB and 2%-3% CRNMB) (see figure).2
Comparison of bleeding estimates in randomized controlled trials vs prospective observational cohort studies. Figure created with BioRender.com.
Comparison of bleeding estimates in randomized controlled trials vs prospective observational cohort studies. Figure created with BioRender.com.
Cancer-associated thrombosis secondary to venous thromboembolism (VTE) has become increasingly well characterized in recent years. Several validated clinical risk assessment models can be used to identify patients at >9% risk of overall VTE within 6 months.3-5 However, despite efficacy evidence from randomized controlled trials and guideline recommendations, oncologists rarely assess for VTE risks or prescribe pharmacologic thromboprophylaxis in the ambulatory setting. One of the often identified barriers to implementation is the potential bleeding risk among unselected patients with unique tumor or therapy types.6 To address this knowledge deficit, Englisch et al have carefully monitored patients with cancer for potential bleeding events during routine oncology outpatient visits for 2 years. By combining self-reported bleeding questionnaires, electronic chart reviews, and independent adjudications, the authors provide novel and high-quality epidemiological estimates for patients meeting either MB or CRNMB criteria according to the current International Society on Thrombosis and Haemostasis (ISTH) definitions.7,8
There are several noteworthy points. First, without exclusion criteria, the high CRB rate (10% at 6 months) in this observational study emphasizes the oncologists’ fear of bleeding. Currently, there are no available validated risk assessment tools for bleeding in patients with cancer without anticoagulation. Therefore, ongoing implementation studies aimed at primary thromboprophylaxis must not only use appropriate VTE risk assessment tools, but also carefully apply the same stringent exclusion criteria from anticoagulant trials. Second, the authors report a high incidence of tumor bleeding (30%) mainly from oropharyngeal or pulmonary site. As a novel category of bleeding exclusive to patients with cancer, the current ISTH definition for bleeding likely needs to be revised and restandardized in the cancer population. Third, among tumor subtypes, those with head and neck cancers had a particularly high 6-month CRB incidence of 24% compared with other high-risk types like lung (9%) and gastrointestinal (9%) cancers. Since many patients with head and neck cancer receive concurrent chemoradiation with weekly oncology visits, the increased health care exposure may have led to higher self-reported bleeding. In a way, this study reminds us that “patient relevant” bleeding may not be the same as “clinically relevant” bleeding. Finally, the case-fatality rates associated with CRB and MB in this study are 5% and 10%, respectively, which are similar to the reported rates in previous anticoagulant studies.9
The findings of this study provide further clarity on the epidemiology of cancer-associated hemostatic imbalance. It highlights the importance of carefully addressing bleeding along with thrombosis in patients with cancer. However, future studies are needed to generalize the CRB findings in more heterogenous populations, including those from nonacademic centers, rural areas, underserved communities, and racially diverse backgrounds. In addition to reaching a new consensus for clinical and research definitions for CRB in patients with cancer, we need multicenter studies with larger sample sizes to derive and validate novel bleeding risk assessment models to complement the existing thrombosis models. Furthermore, we should leverage artificial intelligence and electronic health record tools to automate risk stratifications. Finally, we need to test novel antithrombotic agents that minimize bleeding risk such as factor XI inhibitors. These combined efforts will ultimately reshape our approach to primary thromboprophylaxis for patients with cancer.
Conflict-of-interest disclosure: A.L. declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal