Abstract
Interleukin-2 (IL-2) and IL-15 exert similar biological actions, which largely reflect the fact that their receptors share common β and γ subunits; in contrast, distinct subunits are required for high-affinity binding of either cytokine to a heterotrimeric receptor complex. Human neutrophils are known to express both the β and γ subunits of the IL-2/IL-15 receptor complex, and we now report that they also constitutively express messenger RNA transcripts encoding the IL-15 receptor chain, suggesting that they possess functional, heterotrimeric IL-15 receptors. Accordingly, we show that in neutrophils, IL-15 elicits several functional responses. In particular, neutrophils synthesize and release IL-8 in response to IL-15, but not to IL-2. Moreover, a nuclear factor-κB (NF-κB) DNA-binding activity was enhanced in nuclear extracts of IL-15–treated neutrophils, which could be supershifted by antibodies to p50 or RelA. Again, no detectable effect of IL-2 was observed on this response. In peripheral blood lymphocytes (PBL), however, both IL-2 and IL-15 were potent inducers of NF-κB activation. Conversely, neither IL-15 nor IL-2 elicited the formation of activator protein-1 (AP-1) DNA-binding complexes in neutrophils, even though both cytokines were found to activate these DNA-binding activities in PBL. Collectively, these observations establish neutrophils as a useful cellular model to discriminate between the actions of IL-15 and IL-2. More importantly, this is the first demonstration that IL-15 has the ability to induce NF-κB and AP-1 activation, which further emphasizes the potential relevance of this newly discovered cytokine to immune and inflammatory processes.
INTERLEUKIN-15 (IL-15) IS A recently discovered cytokine whose known biological actions are strikingly similar to those of IL-2.1-4 A likely explanation for this apparent redundancy is that the receptors for both cytokines share common β and γ subunits (IL-2Rβ and IL-2Rγ, respectively), which mediate intracellular signaling, and which together form an intermediate affinity receptor complex.1,2,5-7 In contrast, high-affinity binding of either IL-15 or IL-2 to a heterotrimeric receptor complex is mediated by distinct α chains. Whereas IL-2Rα is specific for IL-2,2,5 a structurally related protein (termed IL-15Rα) was recently cloned that specifically binds IL-15.8
IL-15 has been shown to act on various cells of the immune system, including T lymphocytes, B lymphocytes, natural killer (NK) cells,1-4 and more recently, peripheral blood neutrophils (PBN).9 In the latter instance, IL-15 was observed to induce cytoskeletal rearrangements, to enhance phagocytosis, to increase the synthesis of several cellular proteins, and to delay apoptosis.9 Under identical conditions, however, IL-2 failed to affect any of these responses in neutrophils.9Although these different effects of IL-15 and IL-2 stand in apparent contrast with observations made in other cell types, they nonetheless correlate well with the fact that individual IL-2R subunits are selectively expressed in neutrophils. In this regard, studies from various laboratories have established that human neutrophils constitutively express messenger RNA (mRNA) transcripts encoding the IL-2Rβ and IL-2Rγ, as well as the corresponding proteins on their surface,10-14 but that IL-2Rα surface expression is undetectable in these cells.11-14 Conversely, the ability of IL-15 to directly elicit or to enhance a series of cellular processes in these cells has led some authors to postulate that neutrophils must express specific IL-15R components.9
In the current study, we identified one such component as the IL-15R α chain, whose mRNA was detected in resting neutrophils by RT-PCR; we also confirmed that neutrophils constitutively express mRNA transcripts encoding IL-2Rβ and IL-2Rγ. Consistent with the presence of a high-affinity IL-15 receptor complex in neutrophils, we observed that IL-15 induces the production of IL-8 in these cells. Moreover, we report for the first time that IL-15 has the ability to activate the transcription factors, nuclear factor-κB (NF-κB), and (depending on the cell type) activator protein-1 (AP-1), a finding that opens new perspectives as to the potential involvement of IL-15 in inflammatory and immune processes.
MATERIALS AND METHODS
Antibodies and reagents.
Rabbit antisera to human c-Rel (#1136, raised against an internal sequence downstream from the nuclear localization signal), p65 RelA (#1207, against the N-terminal region), p50 NFκB1 (#1141, against the N-terminal region), and p52 NFκB2 (#1267, against the N-terminal region) were a generous gift from Dr N.R. Rice (NCI-Frederick Cancer Research and Development Center, Frederick, MD). The specificity of these antisera has already been extensively characterized.15,16 Purified antibodies raised against RelB, and against proteins of the Jun and Fos families, were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). An oligonucleotide containing tandemly repeated NF-κB sites identical to those of the HIV promoter (5′-gatcaGGGACTTTCCgctgGGGACTTTCC-3′) was kindly provided by G. Trinchieri (Wistar Institute, Philadelphia, PA). An oligonucleotide containing a consensus AP-1 sequence (5′-cgcttgaTGAGTCAgccggaa-3′) was from Promega Corporation (Madison, WI, USA). Ficoll-Paque, T4 polynucleotide kinase, and poly (dI-dC) were from Pharmacia (Uppsala, Sweden); [γ-32 P]-ATP was from ICN (Cleveland, OH). RPMI 1640 was from GIBCO/BRL (Gaithersburg, MD), and low-endotoxin FCS (< 6 pg/mL) from Hyclone (Logan, UT). Recombinant human (rh) IL-15 was purchased from Genzyme (Cambridge, MA) (and kindly provided by Dr R. Zambello, Department of Clinical Medicine, University of Padova, Italy), and from R&D Systems (Minneapolis, MN); rh IL-2 was obtained from both Genzyme and R&D Systems. Acetylated bovine serum albumin (BSA), cycloheximide, diisopropyl fluorophosphate (DFP), lipopolysaccharide (LPS), and phenylmethanesulphonyl fluoride (PMSF) were from Sigma-Aldrich (St Louis, MO). Aprotinin, 4-(2-aminomethyl)benzenesulfonyl fluoride (AEBSF), leupeptin, and pepstatin A were from Boehringer-Mannheim (Mannheim, Germany). All other reagents were molecular biology grade, and all buffers and solutions were prepared using pyrogen-free clinical grade water.
Cell isolation and culture.
PBN were isolated from healthy donors under endotoxin-free conditions by a modification of the method of Boyum,17 as described earlier.18 As determined by Wright staining and nonspecific esterase cytochemistry, the final neutrophil suspensions consistently contained fewer than 0.5% monocytes; neutrophil viability exceeded 98% after up to 3 hours in culture, as determined by trypan blue exclusion. Peripheral blood mononuclear cells (PBMC) were plated in uncoated plastic culture wells for 2 hours to promote the adherence of monocytes; nonadherent cells were gently washed out, yielding a highly enriched lymphocyte population, hereafter referred to as peripheral blood lymphocytes (PBL). Purified cell populations were resuspended in RPMI 1640 supplemented with 10% low-endotoxin fetal calf serum (FCS), and allowed to equilibrate for 15 minutes at 37°C, before stimulation with IL-15, IL-2, or LPS.
Electrophoretic mobility shift assays (EMSA).
Neutrophils or PBL (5 × 106 cells/mL) were incubated in a water bath (37°C, under agitation) in the presence or absence of the stimuli for the indicated times. Incubations were stopped by transferring aliquots of the cell suspensions into precooled tubes containing equivalent volumes of ice-cold RPMI 1640 supplemented with DFP (2 mmol/L, final concentration), before centrifugation at 2,000g for 2 minutes at 4°C. Cells were resuspended in ice-cold relaxation buffer (10 mmol/L piperazine-N, N′-bis-[2-ethanesulfonic acid] [PIPES], pH 7.30, 10 mmol/L NaCl, 3.5 mmol/L MgCl2, 0.5 mmol/L ethyleneglycoltetracetic acid [EGTA], 0.5 mmol/L EDTA, 1 mmol/L dithiothreitol [DTT]) supplemented with an antiprotease cocktail (1 mmol/L DFP, 1 mmol/L PMSF, 1 mmol/L AEBSF, and 10 μg/mL each of aprotinin, leupeptin, and pepstatin A, final concentrations). After a 10-minute incubation on ice, cells were disrupted by nitrogen cavitation, using a modification of a previously published procedure19 that we described elsewhere.20Nuclear extracts were subsequently prepared and analyzed in EMSA as described.20
Reverse transcriptase-polymerase chain reaction (RT-PCR) analyses.
Neutrophils or PBMC (5 × 106 cells/mL) were cultured in polystyrene flasks at 37°C under a 5% CO2atmosphere. Total RNA was extracted as described previously,18 and analyzed by RT-PCR as reported earlier.21 Amplified PCR products were size-fractioned on 1.5% agarose gels; gels were stained with ethidium bromide and photographed.
Determination of immunoreactive IL-8.
Neutrophils (106 cells/300 μL) were cultured in 24-well culture plates at 37°C under a 5% CO2 atmosphere, in the presence or absence of the stimuli, for the indicated times. Culture supernatants were collected, centrifuged (2,000g, 5 minutes, 4°C) to remove intact cells, snap-frozen in liquid nitrogen, and stored at −70°C. When cell-associated IL-8 was measured, 0.5 mL of ice-cold phosphate-buffered saline (PBS) was added to the wells, and neutrophils were gently scraped and combined with the small cellular pellet resulting from the centrifugation of culture supernatants. Cells were then centrifuged (2,000g, 5 minutes, 4°C); the resulting pellets were resuspended in 300 μL of cold lysis buffer (PBS supplemented with 0.5% NP-40, 5 mmol/L EDTA, 1 mmol/L AEBSF, 1 mmol/L PMSF, and 10 μg/mL each of aprotinin, leupeptin, and pepstatin A), vigorously vortexed for 30 seconds, and centrifuged (15,000g, 10 minutes, 4°C) to remove insoluble material. The resulting supernatants were snap-frozen in liquid nitrogen and stored at −70°C before analysis. The IL-8 concentration of the culture supernatants or of the corresponding cell lysates was determined using a specific enzyme-linked immunosorbent assay (ELISA), as previously described.22 The detection limit for IL-8 using this assay was 20 pg/mL. Alternatively, a commercial ELISA kit (R&D Systems) was used to measure IL-8 protein.
RESULTS
IL-15, but not IL-2, stimulates IL-8 synthesis and release in human neutrophils.
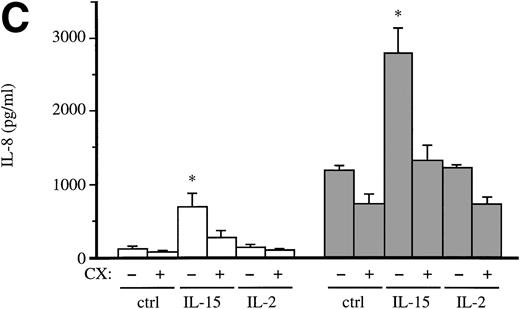
In a recent report, Girard et al9 convincingly established that several neutrophil responses are differentially elicited by IL-15 and IL-2. In particular, IL-15, unlike IL-2, was found to enhance the synthesis of distinct cellular proteins.9 This prompted us to investigate the effect of IL-15 and IL-2 towards a well characterized neutrophil function, ie, the ability to generate chemokines such as IL-8.23 Cells were cultured in the presence or absence of IL-15 or (as a positive control) 1 μg/mL LPS for varying lengths of time; culture supernatants were collected, and their IL-8 content was analyzed by ELISA. As shown in Fig 1A, 20 nmol/L IL-15 (250 ng/mL) promoted the release of IL-8 from human neutrophils, albeit to a lesser extent than LPS. This effect of IL-15 was concentration-dependent, a threshold effect being observed using 8 nmol/L (100 ng/mL) of the cytokine (Fig 1B). By contrast, IL-2 (up to 5000 U/mL, ie, ∼23 nmol/L) invariably failed to exert any significant effect on this response (P = .13 versus unstimulated cells in 6 independent experiments), as shown in Fig 1B. To gain further insight into the mechanisms whereby IL-15 promotes IL-8 release, cells were pretreated with cycloheximide, before stimulation with IL-15 or IL-2 and subsequent determination of IL-8 production. Figure 1C shows that IL-15 potently induced the synthesis of IL-8, and that both IL-8 synthesis and release were inhibited by cycloheximide in IL-15–treated cells, indicating that de novo protein synthesis is required for this response. By contrast, IL-2 neither affected the total production, nor the release of IL-8 in the same experiments (Fig 1C). Finally, it is worthy of mention that pretreatment of our IL-15 stocks with polymyxin B failed to prevent the ability of the cytokine to promote IL-8 release in neutrophils, thereby making it unlikely that endotoxin contamination might contribute to the activating properties of IL-15 reported above.
Effect of IL-15 and IL-2 towards the production of IL-8 in human neutrophils. (A) Cells (106/300 μL) were cultured at 37°C in the presence or absence (–) of 250 ng/mL IL-15 (ie, 20 nmol/L) or 1 μg/mL LPS for the indicated times (in hours). Culture supernatants were collected, and their IL-8 concentration was determined using a specific ELISA. Results are expressed as mean ± standard error of mean (s.e.m.) of duplicate determinations for each experimental condition. Depicted in this panel is a representative experiment; the ability of 20 nmol/L IL-15 to induce IL-8 release was observed in seven independent experiments (P = .002 versus unstimulated cells). (B) Neutrophils (106/300 μL) were cultured for 9 hours at 37°C in the presence or absence of increasing concentrations of either IL-15 (closed squares) or IL-2 (open squares). The IL-8 content of the resulting culture supernatants was then determined by ELISA. Values are the mean ± s.e.m. of duplicate determinations for each experimental condition. This experiment is representative of at least three. (C) Neutrophils (106/300 μL) were cultured for 20 minutes at 37°C in the presence of 10 μg/mL cycloheximide (CX) or its diluent (DMSO), before stimulation with 250 ng/mL IL-15 (ie, 20 nmol/L), 103 U/mL IL-2 (∼5 nmol/L), or diluent control (ctrl), for 8 hours at 37°C. Cell-free culture supernatants and the corresponding cell pellets were collected, and their respective IL-8 concentrations were determined by ELISA. Values are the mean ± s.e.m. of averaged duplicate determinations from three independent experiments. Open bars, IL-8 release; shaded bars, total IL-8 production (ie, released + cell-associated). *, P < .04 relative to control cells, using Student’s t-test for paired data; CX treatment also yielded significantly lower (P < .05) values relative to the matched controls for all conditions tested.
Effect of IL-15 and IL-2 towards the production of IL-8 in human neutrophils. (A) Cells (106/300 μL) were cultured at 37°C in the presence or absence (–) of 250 ng/mL IL-15 (ie, 20 nmol/L) or 1 μg/mL LPS for the indicated times (in hours). Culture supernatants were collected, and their IL-8 concentration was determined using a specific ELISA. Results are expressed as mean ± standard error of mean (s.e.m.) of duplicate determinations for each experimental condition. Depicted in this panel is a representative experiment; the ability of 20 nmol/L IL-15 to induce IL-8 release was observed in seven independent experiments (P = .002 versus unstimulated cells). (B) Neutrophils (106/300 μL) were cultured for 9 hours at 37°C in the presence or absence of increasing concentrations of either IL-15 (closed squares) or IL-2 (open squares). The IL-8 content of the resulting culture supernatants was then determined by ELISA. Values are the mean ± s.e.m. of duplicate determinations for each experimental condition. This experiment is representative of at least three. (C) Neutrophils (106/300 μL) were cultured for 20 minutes at 37°C in the presence of 10 μg/mL cycloheximide (CX) or its diluent (DMSO), before stimulation with 250 ng/mL IL-15 (ie, 20 nmol/L), 103 U/mL IL-2 (∼5 nmol/L), or diluent control (ctrl), for 8 hours at 37°C. Cell-free culture supernatants and the corresponding cell pellets were collected, and their respective IL-8 concentrations were determined by ELISA. Values are the mean ± s.e.m. of averaged duplicate determinations from three independent experiments. Open bars, IL-8 release; shaded bars, total IL-8 production (ie, released + cell-associated). *, P < .04 relative to control cells, using Student’s t-test for paired data; CX treatment also yielded significantly lower (P < .05) values relative to the matched controls for all conditions tested.
IL-15, but not IL-2, induces NF-κB activation in neutrophils.
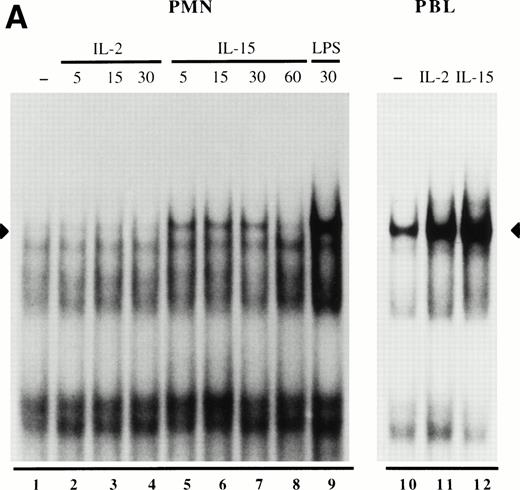
We recently reported that in neutrophils, many of the stimuli that are known to induce IL-8 production also have the ability to activate NF-κB.20 We therefore examined whether this transcription factor can be detected in nuclear extracts from neutrophils stimulated with either IL-15 or IL-2. As a positive control, neutrophils were also stimulated with LPS, which is a powerful NF-κB activator in these cells.20 As shown in Fig 2A, exposure of neutrophils to 20 nmol/L IL-15 (250 ng/mL) resulted in the enhanced detection of a nuclear NF-κB DNA-binding activity, which comigrated with the LPS-inducible NF-κB complex previously characterized as containing primarily p50 and RelA.20 This effect of IL-15 was rapid and transient, because binding of the IL-15–inducible complex to the NF-κB probe was already detectable within 5 minutes, was still elevated at 30 minutes, and had returned to basal levels by 60 minutes. Dose-response experiments additionally showed that a threshold concentration of 8 nmol/L IL-15 (100 ng/mL) is required to detect an effect towards NF-κB activation (data not shown). By contrast, three different commercial IL-2 preparations consistently failed to induce any NF-κB DNA-binding activity in human neutrophils, using up to 103 U/mL (ie, ∼5 nmol/L) IL-2 (Fig 2A and data not shown). The general lack of effect of IL-2 towards neutrophils could not be attributed to a poor biological activity of our IL-2 preparations, because in the same experiments, IL-2 strongly activated NF-κB in autologous PBL (Fig 2A), as expected. Importantly, IL-15 was also found to induce NF-κB activation in human PBL (Fig2A), thereby showing that this IL-15–elicited response is not restricted to neutrophils. It must be noted that the relative ability of IL-15 and IL-2 to activate NF-κB in PBL showed some variation between donors, with IL-15 being somewhat more potent in three out of five experiments (Fig 2A), whereas IL-2 was the more potent stimulus in the remainder. Finally, supershift experiments performed using either neutrophil or PBL nuclear extracts showed that in both cell types, the IL-15–inducible NF-κB complex probably consists of p50-RelA (Fig2B).
Effect of IL-15 and IL-2 towards the activation of nuclear NF-κB DNA-binding activities in human polymorphonuclear neutrophils (PMN) and PBL. (A) Neutrophils were cultured for the indicated times (in minutes), and autologous PBL were cultured for 15 minutes in the presence or absence of 250 ng/mL IL-15 (ie, 20 nmol/L), 103 U/mL IL-2 (∼5 nmol/L), or 100 ng/mL LPS. Nuclear extracts were prepared and analyzed in EMSA using a consensus NF-κB oligonucleotide probe. The amount of extract used in the binding reactions corresponded to 3.5 μg protein (about 3.1 × 106 cell equivalents) for neutrophils, and to 1.5 μg protein (about 1.2 × 10 6 cell equivalents) for PBL. This experiment is representative of six (neutrophils) and five (PBL). (B) Nuclear extracts from IL-15–activated neutrophils or autologous PBL were prepared as described in (A), and incubated without antibodies (–), or with specific antisera to p50, RelA, c-Rel, p52 and RelB, before the addition of labeled NF-κB probe and subsequent EMSA analysis. The amount of extract used corresponded to 3.5 μg of protein (neutrophils), and 1.0 μg of protein (PBL). This experiment is representative of three. Closed arrowheads indicate the inducible NF-κB complex; open arrowheads indicate supershifted bands.
Effect of IL-15 and IL-2 towards the activation of nuclear NF-κB DNA-binding activities in human polymorphonuclear neutrophils (PMN) and PBL. (A) Neutrophils were cultured for the indicated times (in minutes), and autologous PBL were cultured for 15 minutes in the presence or absence of 250 ng/mL IL-15 (ie, 20 nmol/L), 103 U/mL IL-2 (∼5 nmol/L), or 100 ng/mL LPS. Nuclear extracts were prepared and analyzed in EMSA using a consensus NF-κB oligonucleotide probe. The amount of extract used in the binding reactions corresponded to 3.5 μg protein (about 3.1 × 106 cell equivalents) for neutrophils, and to 1.5 μg protein (about 1.2 × 10 6 cell equivalents) for PBL. This experiment is representative of six (neutrophils) and five (PBL). (B) Nuclear extracts from IL-15–activated neutrophils or autologous PBL were prepared as described in (A), and incubated without antibodies (–), or with specific antisera to p50, RelA, c-Rel, p52 and RelB, before the addition of labeled NF-κB probe and subsequent EMSA analysis. The amount of extract used corresponded to 3.5 μg of protein (neutrophils), and 1.0 μg of protein (PBL). This experiment is representative of three. Closed arrowheads indicate the inducible NF-κB complex; open arrowheads indicate supershifted bands.
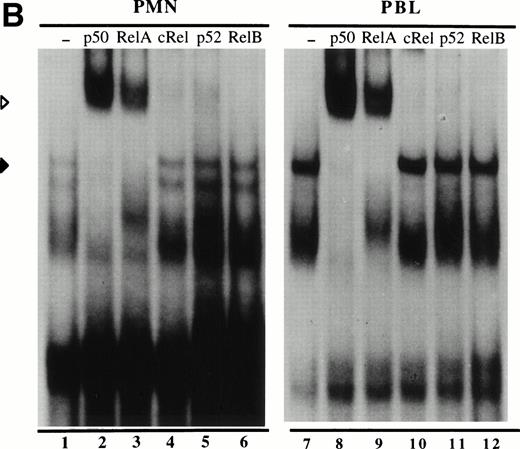
IL-15 and IL-2 induce AP-1 in lymphocytes, but not in neutrophils.
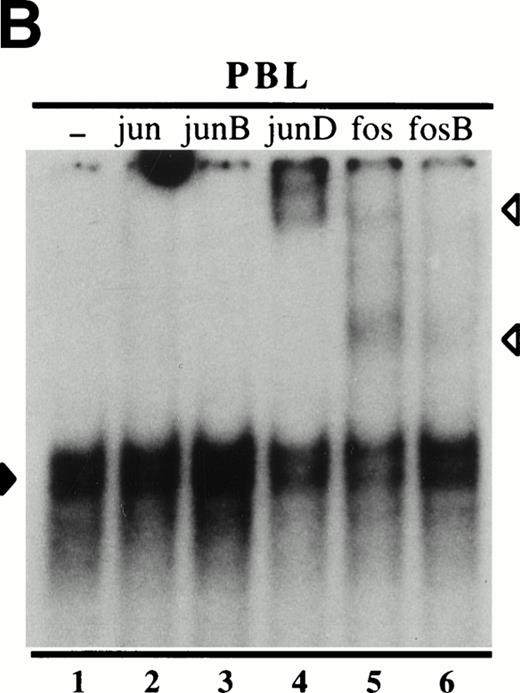
We also investigated whether IL-15 stimulation of neutrophils might result in the activation of AP-1, a transcription factor whose activation often occurs in parallel to that of NF-κB in various cell types. As shown in Fig 3A, neither IL-15 nor IL-2 have the ability to induce AP-1 DNA-binding activity in neutrophils. This lack of effect was observed regardless of the time point examined (ranging from 5 minutes to 1 hour; data not shown). By contrast, both cytokines were found to induce an AP-1 doublet in autologous PBL (Fig 3A, arrowhead); in two out of four experiments, a faster-migrating doublet was also somewhat enhanced in extracts from stimulated cells (Fig 3A). The IL-15–inducible complex appeared to contain c-Fos and JunD, because it was partially supershifted using antibodies that specifically recognize these proteins, but not by antibodies to c-Jun, or JunB (Fig 3B); a weak effect of antiFosB antibodies was also sometimes noted. Identical results were obtained using nuclear extracts from IL-2–activated PBL (data not shown). Whereas the above data indicate that complexes containing c-Fos and/or JunD can be activated by IL-2 and IL-15 in lymphocytes, it cannot be excluded that these complexes contain other proteins as well. In support of this view, is that the combined use of JunD, c-Fos and FosB antibodies failed to supershift the inducible AP-1 complexes to a greater extent than when the same antibodies were used individually (data not shown).
Effect of IL-15 and IL-2 towards the activation of nuclear AP-1 DNA-binding activities in human peripheral blood neutrophils and lymphocytes. (A) Neutrophils or autologous PBL were cultured for 15 minutes in the presence or absence of 250 ng/mL IL-15 (ie, 20 nmol/L) or 103 U/mL IL-2 (∼5 nmol/L); nuclear extracts were then prepared and analyzed in EMSA using a consensus AP-1 oligonucleotide probe. The amount of extract used in the binding reactions corresponded to 5 μg protein for neutrophils, and to 2 μg protein for PBL. This experiment is representative of three (neutrophils) and four (PBL). (B) Nuclear extracts from IL-15–activated PBL (1.5 μg of protein) were prepared as described in (A), and incubated without antibodies (–), or with specific antibodies to c-jun, junB, junD, c-fos, and fosB, before the addition of labeled AP-1 probe and subsequent EMSA analysis. This experiment is representative of three. Closed arrowheads indicate the major inducible AP-1 complex; open arrowheads indicated supershifted bands.
Effect of IL-15 and IL-2 towards the activation of nuclear AP-1 DNA-binding activities in human peripheral blood neutrophils and lymphocytes. (A) Neutrophils or autologous PBL were cultured for 15 minutes in the presence or absence of 250 ng/mL IL-15 (ie, 20 nmol/L) or 103 U/mL IL-2 (∼5 nmol/L); nuclear extracts were then prepared and analyzed in EMSA using a consensus AP-1 oligonucleotide probe. The amount of extract used in the binding reactions corresponded to 5 μg protein for neutrophils, and to 2 μg protein for PBL. This experiment is representative of three (neutrophils) and four (PBL). (B) Nuclear extracts from IL-15–activated PBL (1.5 μg of protein) were prepared as described in (A), and incubated without antibodies (–), or with specific antibodies to c-jun, junB, junD, c-fos, and fosB, before the addition of labeled AP-1 probe and subsequent EMSA analysis. This experiment is representative of three. Closed arrowheads indicate the major inducible AP-1 complex; open arrowheads indicated supershifted bands.
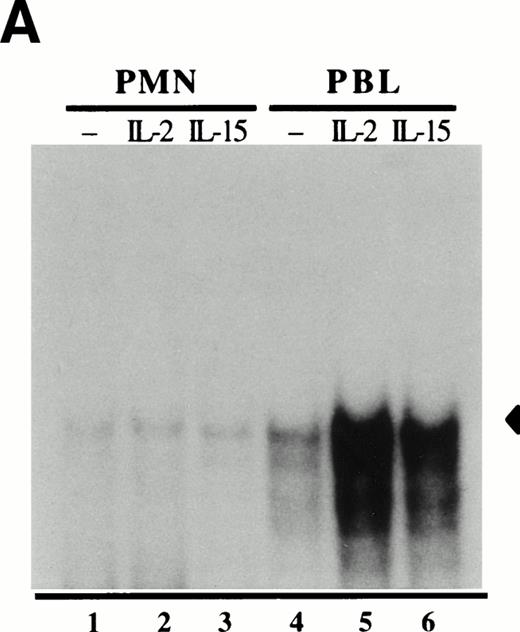
Human neutrophils constitutively express the gene encoding IL-15Rα.
The various stimulatory effects of IL-15 towards neutrophils suggest that these cells must express the IL-15Rα. To clarify this issue, total RNA was extracted and amplified by RT-PCR, using primers specific for IL-15Rα. For comparative purposes, we performed similar analyses using total RNA extracted from autologous PBMC. As shown in Fig 4 (lane 1), two amplification products (at about 530 and 430 base pairs [bp]) were readily detectable in resting neutrophils and (to a lesser extent) in resting PBMC (lane 2). These two complementary DNA (cDNA) species presumably reflect alternatively spliced IL-15Rα mRNA isoforms, based on their respective sizes, and on observations made in other experimental systems.21,24 Using the same approach, we were also able to show that neutrophils constitutively express IL-2Rβ and IL-2Rγ mRNA transcripts (Fig 4, lanes 3 and 5), in agreement with earlier studies.10-14 We finally performed control experiments to ensure that the detection of mRNA transcripts encoding the various IL-15R subunits in our neutrophil preparations did not reflect the presence of contaminating monocyte or lymphocyte RNA. For this purpose, we used cDNA primers specific for the IL-6 gene, which is known to be expressed in peripheral blood monocytes and lymphocytes but not in neutrophils.18,26 27 As shown in Fig 4 (lane 9), no amplified RT-PCR product was detectable using these primers in neutrophils, as opposed to PBMC (lane 10). Similarly, we observed that although TNFα mRNA is induced to similar levels by concanavalin A (ConA) in both PBMC and autologous neutrophils (as determined in ribonuclease protection assays), lymphotaxin-α mRNA is only detected in PBMC (our unpublished data). Taken together, the latter observations make it unlikely that the IL-15R/IL-2R amplification products that we detected in neutrophils might originate from contaminating lymphocytes or monocytes. Thus, human neutrophils constitutively express all three components of the high-affinity IL-15 receptor.
Expression of individual components of the IL-15 receptor complex in human neutrophils. Total RNA was extracted from resting neutrophils and autologous PBMC, and processed by RT-PCR using cDNA primers specific for IL-15R (15R), IL-2Rβ (2Rβ), IL-2Rγ (2Rγ), β-actin, and IL-6. This experiment is representative of three. Odd-numbered lanes, neutrophils; even-numbered lanes, PBMC; mm, migration markers (in base pairs [bp]).
Expression of individual components of the IL-15 receptor complex in human neutrophils. Total RNA was extracted from resting neutrophils and autologous PBMC, and processed by RT-PCR using cDNA primers specific for IL-15R (15R), IL-2Rβ (2Rβ), IL-2Rγ (2Rγ), β-actin, and IL-6. This experiment is representative of three. Odd-numbered lanes, neutrophils; even-numbered lanes, PBMC; mm, migration markers (in base pairs [bp]).
DISCUSSION
Human neutrophils were recently shown to represent a cellular target for IL-15.9 In the present study, we extend the current knowledge on IL-15/neutrophil interactions by showing that in these cells, IL-15 induces the synthesis and release of IL-8, a chemokine that is thought to play a pivotal role in inflammatory reactions. Consistent with this finding, Girard et al9 previously showed that in IL-15–treated cells, at least 11 proteins were synthesized de novo. A closer examination of their data further shows that one of these proteins migrated well below the 14-kD marker, and had a markedly basic isoelectric point.9 Interestingly, these electrophoretic properties are strikingly similar to those of IL-8, a protein that has an Mr of about 8 kD in sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE),27 and a pI of 9.4.28 Finally, while this manuscript was in preparation, Badolato et al29reported that IL-15 has the ability to induce the production of IL-8 in human monocytes, in keeping with the current data. Together, these observations suggest that in an inflammatory setting, the combined presence of IL-15 and neutrophils (or monocytes) could potentially result in a significant synthesis of IL-8. That this is indeed the case in certain pathophysiological conditions grants credibility to this scenario. For instance, elevated amounts of IL-15 have been detected in the synovial fluid of arthritic joints,30 which typically contain large numbers of neutrophils, as well as high concentrations of IL-8.31 Therefore, through its ability to induce the synthesis of IL-8, IL-15 could promote the recruitment of additional neutrophils to inflamed tissues, thereby amplifying ongoing inflammatory reactions. In addition, IL-15 has the potential to exacerbate the proinflammatory activities of infiltrating neutrophils at inflammatory sites, by virtue of its ability to delay neutrophil apoptosis and to enhance their phagocytic activity (Girard et al9 and our unpublished data). Collectively, these considerations suggest a potentially important role for IL-15 in neutrophil-mediated inflammatory processes.
In contrast to the numerous actions exerted by IL-15, neutrophil function appears to be only poorly (if at all) affected by IL-2,9,12 and our current observations strongly support this view. Whereas it has been reported that 103 U/mL IL-2 induces the release of IL-8 in human neutrophils,32 we were unable to reproduce these observations, even though we used three commercially available IL-2 preparations, which were all biologically active, as evidenced by their ability to induce transcription factor activation in PBL (Fig 3,4). Although we have no explanation for this discrepancy, it is noteworthy that other investigators have observed that a broad range of IL-2 concentrations not only failed to elicit IL-8 release in neutrophils (D. Girard, personal communication), but also failed to increase the de novo synthesis of any protein in these cells.9 Similarly, we observed in preliminary studies that although 25 ng/mL IL-15 (ie, 2 nmol/L) enhanced the phagocytosis of IgG-opsonized sheep erythrocytes, up to 103 U/mL IL-2 (ie, ∼5 nmol/L) was ineffective towards this response (our unpublished data). This is in good agreement with a recent study, in which similar concentrations of IL-15 and IL-2 were also found to affect neutrophil phagocytic activity differentially9; the inability of IL-2 to enhance ongoing phagocytosis had also been reported by other groups.33-35 Collectively, the different actions of IL-15 and IL-2 correlate well with the fact that individual subunits of the IL-2/IL-15 receptor complexes are selectively expressed in neutrophils. Indeed, we show herein that neutrophils constitutively express mRNA encoding the IL-15R α chain; we also confirm earlier reports that had established that both IL-2Rβ and IL-2Rγ are expressed in resting neutrophils.10-14 Thus, all three components of the high-affinity IL-15 receptor are expressed in neutrophils. Conversely, several groups have reported that IL-2Rα surface expression is undetectable in these cells.11-14 The latter observation might therefore provide a basis for the general lack of effect of IL-2 towards many neutrophil responses, and further indicates that IL-2Rα must be a critical component of a fully functional IL-2R complex. Consistent with this interpretation is that despite the fact that up to 70% of neutrophils express both IL-2Rβ and IL-2Rγ on their surface, fewer than 20% of the cells actually bind fluorescent-labeled IL-2.12 Thus, the differential ability of IL-2 and IL-15 to stimulate human neutrophils might reflect the pattern of expression of the various IL-2R and IL-15R subunits in this cell type.
In the current study, we also explored one of the potential mechanisms involved in the stimulatory effect of IL-15 towards IL-8 production in neutrophils. In this respect, studies performed in other cell types have established that IL-8 gene expression and release are largely dependent on NF-κB activation.36-38 In keeping with these observations, we found that IL-15 transiently activates NF-κB in neutrophils. To our knowledge, this represents the first demonstration that IL-15 is an NF-κB inducer in any cell type studied to date. Conversely, even though the binding of AP-1 complexes to their cognate sequence within the IL-8 promoter has also been proposed to participate in transcriptional induction,39,40 this is unlikely to be the case in IL-15–treated neutrophils because IL-15 did not promote detectable AP-1 activation in these cells. By comparison, IL-2 failed to activate either NF-κB or AP-1 in neutrophils, consistent with the observed inability of IL-2 to stimulate IL-8 production in these cells. In PBL, however, IL-2 proved to be a strong stimulus of NF-κB activation, as expected. More importantly, IL-15 induced NF-κB activation to a comparable extent as did IL-2 in PBL, thereby showing that this IL-15–elicited response is not restricted to neutrophils. In addition, both IL-15 and IL-2 were found to induce AP-1 DNA-binding activities that contain c-Fos and JunD (and perhaps other proteins) in human PBL. With respect to IL-15, this constitutes the first demonstration of its ability to induce AP-1 activation, whereas IL-2 had already been reported to activate AP-1 in a gibbon leukemia cell line41 as well as in the murine CTLL-2 cell line,42 but surprisingly, not in human cells. Collectively, these observations suggest that in cells expressing the IL-15R, the expression of κB-dependent genes is likely to be upregulated in response to IL-15 (as shown herein for the IL-8 gene product in neutrophils), and that in lymphocytes at least, both IL-15 and IL-2 might likewise induce the expression of genes whose promoters are under the control of AP-1. In keeping with this view, the IL-2Rα and TNFα gene promoters contain NF-κB sites that are required for transcriptional inducibility (reviewed in Baeuerle and Henkel43), and in lymphocytic cells, IL-15 was indeed reported to induce the accumulation of IL-2Rα mRNA44 and to increase TNFα production.45 Similarly, the induction of the TNFα gene has been reported to involve an AP-1 site in its promoter,46 which raises the possibility that the induction of TNFα production by both IL-15 and IL-2 in human peripheral T lymphocytes45 might partially reflect the ability of these cytokines to induce AP-1, as observed herein in PBL. Further studies are clearly required to fully document the mechanisms underlying the actions of IL-15 in various cells of the immune system.
In conclusion, despite the fact that IL-15 and IL-2 exert similar biological actions in several cell types, neutrophils could represent an interesting cellular model to discriminate between the effects of these two cytokines. Conversely, some neutrophil responses were unaffected by IL-15. In this regard, the inability of IL-15 to induce AP-1 activation in these cells might provide important insights into how IL-15 signalling is coupled (or uncoupled) to various aspects of transcriptional regulation. In a broader context, the envisaged use of IL-15 in cancer therapy47,48 will have to take into consideration the potential of IL-15 to induce the expression of proinflammatory genes through its ability to activate NF-κB and AP-1 (as shown herein), as well as distinct members of the signal transducers and activators of transcription (STAT) family of transcriptional activators.4
ACKNOWLEDGMENT
We are indebted to Dr Nancy Rice for having generously provided many antisera. We also wish to thank Dr Peter Henson for his critical reading of this manuscript. P.P. McDonald is a Centennial Postdoctoral Fellow of the Medical Research Council of Canada.
Supported by grants from the MURST (fondi 40% e 60%, e cofinanziamento MURST-Università), the AIRC, and the Fondazione Cassa di Risparmio VR-VI-BL-AN (progetto Sanità96/97), as well as from the National Institutes of Health (NIH Grant No. GM48211).
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Patrick P. McDonald, PhD, National Jewish Research Center, Neustadt Bldg, Room D501,1400 Jackson St, Denver, CO 80206; e-mail: mcdonaldp@njc.org.



![Fig. 4. Expression of individual components of the IL-15 receptor complex in human neutrophils. Total RNA was extracted from resting neutrophils and autologous PBMC, and processed by RT-PCR using cDNA primers specific for IL-15R (15R), IL-2Rβ (2Rβ), IL-2Rγ (2Rγ), β-actin, and IL-6. This experiment is representative of three. Odd-numbered lanes, neutrophils; even-numbered lanes, PBMC; mm, migration markers (in base pairs [bp]).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/12/10.1182_blood.v92.12.4828/5/m_blod42409004w.jpeg?Expires=1765981142&Signature=FcGJOhCOmEGvV9lz3F3QDBqCUhj~HoGPhfMiPfo29FBRilgTCs6JcVhfXgYLcn5kOz2gZ4D-dgtVTn8HwdLhwm-bJBH2Spok6kiLtw6Wz9a3XCcWOmVH2gV3V5d0LSuS1r0FkdcgS7J6dqSqqge51jr-BHBQqfTMGU8tFzFq5VTwhhQpjhsHr15cqYQNSF~Vev3wslPYAEBD~NyrA71m8w~r1t7iZw-GP-G4oDVeiwJNNiMzRo2D0Ta7cUQeBpkW3R3X8bjSW0cKLsHXh2NJPmyuI3mNLhtoLLGwaCOAm7WnrVQz3UWe-b2vpaeEL5h1-N5mMX-D4CHPEZQgf6hSwQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal