Since the cloning of interleukin (IL)-15 six years ago, there have been numerous studies examining the molecular and cellular biology of this cytokine. IL-15 and IL-2 have similar biologic properties in vitro, consistent with their shared receptor (R) signaling components (IL-2/15Rβγc). However, specificity for IL-15 versus IL-2 is provided by unique private α-chain receptors that complete the IL-15Rαβγ and IL-2Rαβγ heterotrimeric high-affinity receptor complexes and thereby allow differential responsiveness depending on the ligand and high-affinity receptor expressed. Intriguingly, both IL-15 and IL-15Rα transcripts have a much broader tissue distribution than IL-2/IL-2Rα. Further, multiple complex posttranscriptional regulatory mechanisms tightly control IL-15 expression. Thus, based upon complex regulation, as well as differential patterns of IL-15 and IL-15Rα expression, it is likely that the critical in vivo functions of this receptor/ligand pair differ from those of IL-2 and IL-2Rα. Studies to date examining the biology of IL-15 have identified several key nonredundant roles, such as IL-15's importance during natural killer (NK) cell, NK–T cell, and intestinal intraepithelial lymphocyte development and function. A role for IL-15 during autoimmune processes such as rheumatoid arthritis and malignancies such as adult T-cell leukemia suggest that dysregulation of IL-15 may result in deleterious effects for the host. This review attempts to present concisely our current understanding of the cellular and molecular biology of IL-15, IL-15's role in human disease, and its potential clinical utility as a therapeutic agent or target.
Molecular and cellular biology of interleukin 15 (IL-15)
The discovery of IL-15 and its relation to IL-2
IL-15 was identified by 2 independent groups based upon its ability to stimulate proliferation of the IL-2–dependent CTLL-2 T-cell line in the presence of neutralizing anti–IL-2 antibodies. The activity within cell culture supernatants of the simian kidney epithelial cell line CV-1/EBNA was purified, molecularly cloned, and designated IL-15.1 The activity identified in supernatants of the human T-cell leukemia virus-1 (HTLV-1) cell line, HuT-102, was purified and called IL-T.2 3
Scientists at the Immunex Corporation (Seattle, WA) isolated the 14- to 15-kd protein responsible for the CTLL proliferation within CV-1/EBNA supernatants using anion-exchange and high-pressure liquid chromatography and sequenced the NH2-terminal residues. Degenerate oligonucleotide primers were generated from this partial protein sequence and were used to obtain the full-length simian IL-15 cDNA from a CV-1/EBNA cDNA library. With simian IL-15 cDNA as a probe, the full-length human IL-15 cDNA was cloned from the IMTLH bone marrow stromal cell line.1 The IL-T protein identified by researchers at the National Institutes of Health within HuT-102 supernatants was later cloned and shown to be a chimera composed of the HTLV-1 long terminal repeat (LTR) and human IL-15. The HTLV-1 LTR was fused in frame immediately upstream of IL-15, thereby deleting a portion of its 5′ untranslated region (UTR).2-4
Because IL-15 was initially identified through its ability to mimic IL-2–induced T-cell proliferation, the biochemical and functional relation between these cytokines was quickly examined. Comparisons of the primary protein and cDNA sequences of human or simian IL-15 yielded little primary homology to IL-2; however, computer modeling of IL-15's secondary structure suggested that IL-15 belonged to the 4 α-helix bundle cytokine family,1 including human growth hormone, IL-2, IL-3, IL-6, IL-7, granulocyte colony-stimulating factor (G-CSF), and granulocyte-macrophage colony-stimulating factor (GM-CSF).5,6 Functional studies using antibodies that blocked the various IL-2R subunits determined that IL-15 used the IL-2Rβ subunit and the common gamma chain (γc), but not the IL-2Rα. Because signaling via IL-2 and IL-15 appears to occur exclusively via the same βγ chains, IL-15 mediates functions similar to IL-2 in vitro.1,3,7 However, in vivo it is the distribution of the distinct IL-15Rα and IL-2Rα chains that directs when and where each ligand will bind and activate via this βγ signaling pathway. Through the development of mice with targeted disruption of the IL-158 and IL-15Rα9 genes, it is now apparent that IL-15 and IL-2 mediate very different in vivo functions. The similarities and differences between IL-15 and IL-2 are highlighted where appropriate below.
Structure of the genomic locus encoding IL-15
The IL-15 gene spans 34 kb or more, mapping to human chromosome 4q31 and the central region of mouse chromosome 8.10,11 The genomic structure of human IL-15 contains 9 exons (7 coding exons), with a similar intron/exon structure and estimated size between the murine and human IL-15 genes.10,11 More recently, an alternative exon has been described in human12-14 and murine15,16 IL-15, consisting of an additional sequence between exons 4 and 5 that encodes an alternative leader peptide. The structure of the human IL-15 genomic locus is diagramed in Figure 1 and includes the recently described alternative exon (4A).11,12,14 The IL-2 gene is located on human chromosome 4q26-28 and consists of 4 exons and 3 introns.17,18 Of note, the overall intron/exon structure of the portion of the IL-15 gene encoding the mature IL-15 protein (4 exons and 3 introns) is similar to that of the IL-2 gene and other 4 α-helix bundle cytokines.5 However, consistent with other family members, there is little primary homology between IL-2 and IL-15 at the nucleotide or protein level (Figure2).1 Thus, although it is doubtful that the IL-2 and IL-15 genes have a direct, recent ancestral relationship, the gene structure of all members of the 4 α-helix bundle cytokine family appears similar.5
Human IL-15 gene, mRNA, and protein structure.
The human IL-15 locus consists of 9 exons and 8 introns and is located on chromosome 4q31.10 11 Two IL-15 mRNA isoforms have been described, the classical LSP and alternative SSP, with both encoding an identical IL-15 mature protein of 114 AAs (see text for details). Translational start sites (→) and stop codons (●) are indicated; in2 indicates intron 2.
Human IL-15 gene, mRNA, and protein structure.
The human IL-15 locus consists of 9 exons and 8 introns and is located on chromosome 4q31.10 11 Two IL-15 mRNA isoforms have been described, the classical LSP and alternative SSP, with both encoding an identical IL-15 mature protein of 114 AAs (see text for details). Translational start sites (→) and stop codons (●) are indicated; in2 indicates intron 2.
Comparison of IL-15 and IL-2 homology at the DNA, primary protein, and tertiary protein levels.
The model of IL-2's tertiary folding structure was generated from known crystal structures from protein data bank data file3INK.284 The theoretical model of IL-15's tertiary structure was generated using IL-2's 3-dimensional structure as a template and the SwissProt software program, and yielded results similar to those described.23
Comparison of IL-15 and IL-2 homology at the DNA, primary protein, and tertiary protein levels.
The model of IL-2's tertiary folding structure was generated from known crystal structures from protein data bank data file3INK.284 The theoretical model of IL-15's tertiary structure was generated using IL-2's 3-dimensional structure as a template and the SwissProt software program, and yielded results similar to those described.23
IL-15 mRNA isoforms, signal sequences, and intracellular trafficking
The originally identified human IL-15 cDNA contains a 5′ UTR of at least 316 base pairs (bp), a 486-bp open reading frame, and a 3′ UTR of at least 400 bp, encoding a precursor IL-15 with an unusually long 48–amino acid (AA) leader peptide and a 114-AA mature protein.1 Identification of human, simian, and murine IL-15 indicated that IL-15 was conserved between species (97% identity comparing human and simian; 73% identity comparing human with murine).1 An alternative human IL-15 cDNA was identified containing an additional exon.12,13 This variant IL-15 human cDNA contains 119 nucleotides (nt) within intron 4 but lacks exons 1 and 2 of the original cDNA, resulting in a smaller spliced mRNA product (Figure 1).14 However, this exonic sequence encoded 3 premature stop codons and a novel downstream ATG translation start site, resulting ultimately in an IL-15 precursor protein with a 21-AA short signal peptide (SSP), compared with the original 48-AA long signal peptide (LSP). A similar alternative transcript has been described in the mouse.15,16 In human and mouse, both IL-15 isoforms encode an identical mature IL-15 protein, containing differences only within the signal sequence. Regulation of the IL-15 mRNA species expressed may occur through alternative splicing and/or an additional uncharacterized IL-15 promoter driving the expression of the SSP–IL-15.14
The 2 IL-15 mRNA isoforms have significant differences in the N-terminal portions of their leader peptides (Figure 1). Leader peptides determine the intracellular localization and potential secretion of the associated mature protein. Both LSP–IL-15 and SSP–IL-15 appear to have low secretion potential compared with well-secreted cytokines such as IL-2, as replacement of either endogenous IL-15 signal peptide (SP) by CD3313 or IgVκ19 signal peptides resulted in efficient secretion of bioactive IL-15 protein. Both LSP–IL-15 and SSP–IL-15 isoforms had 2 to 3 log-fold less secretion than IL-2 SP,14 and analysis with IL-15–green fluorescent protein (GFP) fusion proteins demonstrated that LSP–IL-15 was targeted to the secretory pathway (endoplasmic reticulum [ER]/Golgi apparatus), whereas SSP–IL-15 appeared to be restricted to the cytoplasm and nucleus.14,20,21 This differential trafficking is discussed later in the context of the regulation of IL-15 gene expression. SSP–IL-15 mRNA is expressed in the heart, thymus, appendix, and testis, whereas LSP–IL-15 is in skeletal muscle, placenta, heart, lung, liver, thymus, and kidney; the biologic significance of these observations will require further investigation.12,14 Recently, Nishimura et al22 generated transgenic mice that express both isoforms of IL-15 under the control of a major histocompatibility complex (MHC) class I promoter, documenting differential in vivo roles for LSP- and SSP–IL-15 (see below).
Structure of the mature IL-15 protein
The 14- to 15-kd, 114-AA mature IL-15 protein is encoded by exons 5 to 8 of the IL-15 gene (Figure 1).1,10,11 IL-15 contains 2 disulfide bonds at positions C42-C88 and C35-C85 (single-letter amino acid codes), the former being homologous to the C-C within IL-2. There are 2 N-linked glycosylation sites at the C-terminus of the IL-15 protein, at N79 and N112. The mature IL-15 protein has been predicted to have strong helical moments at AAs 1 to 15, 18 to 57, 65 to 78, and 97 to 114, supporting a theoretical model of a 4 α-helix bundle structure (Figure 2).1 23
The IL-15 receptor (R) complex and its relation to the IL-2R complex
Three different IL-2R complexes exist: The isolated IL-2Rα binds IL-2 with low affinity (Ka approximately 108M−1) without transducing a signal; the heterodimeric IL-2Rβγ binds IL-2 with intermediate affinity (Kaapproximately 109 M−1) and transduces intracellular signals; and the heterotrimeric IL-2Rαβγ binds IL-2 with high affinity (Ka approximately 1011M−1) and also signals.18,24,25 The IL-2Rγ, also referred to as γc, is shared by receptors for IL-2, IL-4, IL-7, IL-9, and IL-15.26,27 Early experiments using specific blocking monoclonal antibodies (MoAbs) documented the participation of the IL-2Rβ and γc, but not the IL-2Rα, in IL-15 binding and function, suggesting the presence of an additional subunit for high-affinity IL-15 binding to the IL-15R complex.3,7,28,29 The murine and human IL-15Rα subunits were subsequently cloned and characterized and shown to be highly homologous to their IL-2Rα counterparts.29,30 The full-length human IL-15Rα is a type-1 transmembrane protein with a signal peptide of 32 AAs, an extracellular domain of 173 AAs, a transmembrane domain of 21 AAs, a 37-AA cytoplasmic tail, and multiple N- or O-linked glycosylation sites.30,31 Comparison of the IL-2Rα and the IL-15Rα revealed the presence of a conserved protein binding motif (sushi domain or GP-1 motif) and similar intron/exon structure, placing IL-2Rα and IL-15Rα as the founding members of a new receptor family.29 Through transfection experiments, it was established that the full-length IL-15Rα alone was sufficient for high-affinity (Ka greater than or equal to 1011 M−1) binding of IL-15, but, similar to IL-2Rα, it played no role in signal transduction. This high affinity of the isolated IL-15Rα for IL-15 is in stark contrast to the IL-2Rα, which has low affinity for IL-2 (Ka approximately 108 M−1) in the absence of the IL-2Rβγ. Thus, the IL-15Rα binds IL-15 with high affinity, but transduces signals only in the presence of the IL-2/15Rβ and γc(Figure 2). IL-15, like IL-2, may also bind and signal through the heterodimeric IL-2/15Rβγc with intermediate affinity (Ka approximately 109 M−1) in the absence of IL-15Rα.28
Eight splicing variants of the hIL-15Rα have been identified, including all combinations of exon-2 deletion, exon-3 deletion, and alternative use of exon 7 or 7′.10,31 Isoforms that lacked exon 2 (Δ2) were unable to bind IL-15, raising the possibility that Δ2IL-15Rα may associate with IL-2/15Rβγc, removing them from participation in high-affinity IL-15R complexes. Although all isoforms of IL-15Rα were detected within the plasma membrane, ER, and Golgi apparatus, only IL-15Rα forms containing exon 2 localized to the nuclear membrane.31 The localization of both IL-15Rα and SSP–IL-15 to the nuclear membrane/nucleus calls for additional studies to better characterize their biologic significance.
The originally identified full-length IL-15Rα transcript (approximately 1.7 kb) was detected in numerous tissues and cell lines, demonstrating a much wider distribution than the IL-2Rα.30 Expression of all 8 IL-15Rα isoforms was observed in multiple tissues (eg, brain, intestine, liver, peripheral blood mononuclear cells [PBMCs]) and cell lines; however, the relative expression of each isoform varied.31 Because of the high affinity of IL-15Rα for IL-15, it has been hypothesized that the IL-15Rα may act as a molecular sink for excess IL-15 or may associate with other receptor components yet to be identified.30,32 A distinct high-affinity binding receptor (60 to 65 kd, IL-15RX) has been identified on mast cells that does not include the identified IL-2/15Rβ, γc, or IL-15Rα and that transduces different intracellular signals than IL-15Rαβγ.33 Further studies are required to understand the functional importance of IL-15's binding to IL-15RX in mast cell biology because no mast cell developmental defects were found in IL-15−/− mice.8
How does IL-15 relate to other cytokines that use the γc receptor?
Several cytokines share the γc receptor, including IL-2, IL-4, IL-7, IL-9, and IL-15, all of which use additional subunit(s) for specificity or signaling.34,35 In vivo experiments engineering mice with targeted disruption of these cytokines or their specific receptor subunits elegantly demonstrated that although γc is shared, it mediates different biologic functions when paired with individual cytokines. Comprehensive comparative reviews of γc-binding cytokines have been provided elsewhere.36-38
Pathways of IL-15 signal transduction
Because IL-2 and IL-15 share common signaling components (IL-2/15Rβγc), most evidence to date suggests that the interaction of IL-15 with its receptor complex in various cell types leads to a series of signaling events that are similar, if not identical, to those elicited by IL-2.39 These include activation of the Janus kinase (Jak)/signal transducer and activator of transcription (STAT) pathway.40 IL-2/15Rβ is associated with Jak1 and the γc is associated with Jak3, resulting in STAT3 and STAT5 phosphorylation, respectively, after ligation with IL-15 (Figure 2).41,42 Additional signaling pathways through the IL-2/15R complexes include the src-related tyrosine kinases, induction of Bcl-2, and stimulation of the Ras/Raf/MAPK pathway that ultimately results in fos/jun activation.43 In neutrophils, IL-15 has been shown to activate NF-κB but not AP-1, whereas IL-15 stimulation of bulk human peripheral blood lymphocytes activated both transcription factors.44 However, reports of IL-15– but not IL-2–induced signals in an IL-15Rα+IL-2/15Rβ colonic epithelial cell line leave open the possibility of alternative IL-15Rα signaling mechanisms.45 The alternative receptor system in mast cells (IL-15RX) has been shown to induce phosphorylation of Jak2 and STAT5,33,46 as well as Tyk2 and STAT6.47
Physiologic expression of IL-15
IL-15 mRNA is produced by multiple tissues (placenta, skeletal muscle, kidney, lung, heart, monocytes/macrophages)1 and numerous cell types through various stimulatory conditions.48-60 The first cell types to be implicated as a functionally relevant source of IL-15 in the context of the immune response were members of the monocyte/macrophage lineage.48,49 Other antigen-presenting cells (APCs), such as blood-derived dendritic cells, have been shown to produce IL-15 mRNA and protein, suggesting a role in the attraction and stimulation of T cells.50,51 IL-15 is also produced by bone marrow (BM) stromal cell lines,1 primary human BM stromal cells,52 thymic epithelium,53 and fetal intestinal epithelium,54 consistent with IL-15's role during hematopoiesis. Epithelial and fibroblast cells from various tissues have been documented to produce IL-15 mRNA and/or protein, including kidney epithelial cell lines,1 epidermal skin cells and keratinocytes,55 fetal skin,56retinal pigment epithelium,57 and intestinal epithelial cells.58 Other cells producing IL-15 with a less obvious function, and requiring further investigation, include kidney proximal tubule cells59 as well as astrocytes and microglia.60 Although not detected initially,1 T cells were later shown by more sensitive techniques to express IL-15 mRNA.61 Considering the extensive posttranscriptional control of IL-15 now evident (see below), it will be important to document IL-15 protein production, either intracellularly, at the cell surface, or secreted extracellularly, to better understand the true role of IL-15 during normal homeostasis and immune defense.
Regulation of IL-15 gene expression
IL-15 transcription, translation, and secretion have proved to be regulated through multiple complex mechanisms. This topic has been recently reviewed in depth elsewhere,46,62 and only the major points of interest are summarized here. Although transcriptional control of IL-15 is important,63 64 the principle level of IL-15 regulation appears to be posttranscriptional.
Control of transcription.
Both human and murine 5′ regulatory regions upstream of exon 1 have been cloned, sequenced, and analyzed for consensus transcription factor binding motifs.61,65 These studies revealed some common consensus binding sites within the mouse and human promoter regions, including α–INF-2, NF–IL-6, γ-IRE, myb, GCF, and NF-κB. The NF-κB site located at −75 to −65 relative to the transcription start site of the human IL-15 promoter was shown to be important for HTLV-1 Tax protein–induced IL-15 mRNA up-regulation61 and for lipopolysaccharide (LPS)-induced IL-15 gene expression in murine macrophages.65 The region −201 and −141 in the human IL-15 promoter was reported to contain an unidentified site responsible for negative regulation of IL-15 expression, as 5′ deletion of this region resulted in a dramatic increase in IL-15 promoter activity.61
An essential interferon regulatory factor (IRF)-E consensus-binding site was identified at −348 to −336 relative to the cap site of the murine IL-15 promoter, following the observation that IRF-1−/− mice simultaneously lack inducible IL-15 expression and natural killer (NK) cells.63 64 It remains unclear what upstream signals are responsible for IRF-induced IL-15 expression during the normal physiologic process of NK cell development in the BM (discussed below).
Primary regulation of IL-15: translation, intracellular trafficking, and secretion.
Three primary checkpoints have been identified that regulate IL-15 mRNA translation into the IL-15 precursor protein: multiple start codons (AUGs) in the 5′ UTR, the unusual LSP and SSP, and a negative regulator near the C-terminus of the precursor proteins. The LSP–IL-15 5′ UTR is relatively long (more than 316 nt in humans) and contains multiple (12 in humans) AUGs upstream of the actual translation start site that have been shown to dramatically reduce translational efficiency.1,4,66 Bamford et al4 demonstrated that removal of 8 of 10 upstream AUGs in the 5′ UTR of the human LSP–IL-15 by fusion with the HTLV-1R region resulted in enhanced IL-15 protein production in the HuT-102 cell line (approximately 5- to 10-fold). However, when the upstream AUGs were circumvented, IL-15 translation and secretion still appeared lower than those of other cytokines, such as IL-2.
Tagaya et al14 showed that replacement of endogenous IL-15 signal peptides with the human IL-2 signal peptide resulted in dramatically elevated IL-15 levels detectable in supernatants from COS-7 transfectants. LSP–IL-15 was shown to have a lower translational efficiency than SSP–IL-15 or IL-2SP–IL-15. With the use of IL-15–GFP fusion constructs, it was evident that SSP–IL-15 was restricted to the cytoplasm and nucleus, whereas LSP–IL-15 was detected within the ER/Golgi apparatus. Thus, it appears that SSP–IL-15 is translated efficiently but not secreted, whereas LSP–IL-15 is translated less efficiently but has complex trafficking through the ER/Golgi pathway and is secreted from the cell at low levels.14,21Similarly, Gaggero et al20 showed that LSP–IL-15 and exogenous IL-15 were detectable in Chinese hamster ovary (CHO) cell endosomes, indicating that rapid uptake by IL-15R–bearing cells may have a regulatory effect on the action of IL-15. The CTLL bioactivity of the LSP–IL-15–GFP construct was significantly higher than that of the LSP–IL-15 without a 3′ tag, suggesting that a signal in the carboxyl portion of the mature IL-15 protein results in inefficient secretion, possibly through a retention signal.20
Through the systematic elimination of these 3 checkpoints, that is, removing upstream AUGs, replacing the endogenous human IL-15 leader with that of IL-2, and fusing the C-terminus of the IL-15 mature protein with the FLAG epitope tag, the synthesis of bioactive IL-15 increased 250-fold.67 Such complex and tight control of the IL-15 gene product is unusual for most cytokines characterized thus far and may indicate that IL-15, if overproduced, is somehow dangerous to the host. Transgenic mice that overexpress IL-15 as a result of elimination of posttranscriptional checkpoints recently provided in vivo evidence supporting this hypothesis.68 These mice developed a fatal lymphocytic leukemia following early expansions in NK and CD8+ T cells (see below).
Recently, Musso et al69 detected bioactive IL-15 protein constitutively expressed on the surface of human monocyte/macrophage cell lines and primary human monocytes. Cell surface expression was increased upon stimulation with interferon (IFN)-γ, suggesting a mechanism by which IL-15 could exert a biologic effect while being undetectable in culture supernatants. It is unclear whether this membrane expression of IL-15 depends upon signal peptide expression. Another recent report demonstrated constitutive IL-15 protein expression in human PBMCs by Western analysis and flow cytometry, which was up-regulated by Cryptococcus neoformans, LPS, or IFN-γ.70 Further study should reveal the exact cell types, tissue distribution, and functional significance of constitutive cell surface expression of IL-15. IL-15's function in promoting the survival of IL-15–responsive cell types, such as NK cells71 and memory T cells,72 may be one hypothesis explaining the reason for low constitutive protein expression. Then, in response to an infectious insult, cytoplasmic protein may be translocated to the cell surface to further stimulate IL-15R–bearing cells, in combination with additionally induced monokines such as IL-12.
In other physiologic settings such as NK cell development (discussed below), it will be interesting to examine BM stromal cells for constitutive cell-surface expression of IL-15 and to test whether any signals induce the movement of cytoplasmic IL-15 protein to the cell surface. In both of these settings, it seems likely that activation of monocytes/macrophages (and other cells such as dendritic cells and epithelium) or appropriate stimulation of BM stromal cells could result in more efficient IL-15 synthesis, translocation, and secretion through removal of the multiple posttranscriptional control points.
IL-15 and immune cells
An essential role for IL-15 in NK cell development
Two critical features of the mammalian innate immune system are its ability to rapidly limit the spread of infectious pathogens and its ability to prepare the antigen-specific or adaptive immune system to effectively clear the pathogens.73 NK cells74,75 are large granular lymphocytes (LGLs) that demonstrate cytotoxicity against tumor and virally infected cells, produce immunoregulatory cytokines and chemokines, and are an important component of the innate immune defense against viruses, fungi, bacteria, and protozoa.76-80 NK cells also express a number of cell surface receptors that recognize MHC class I ligands and regulate NK cell activation and lysis of target cells,81,82 and are likely to be important for the control of some cancers.83
It has long been appreciated that NK cells require the BM microenvironment for complete maturation, based upon studies examining mice with BM ablation by strontium 89 or β-estradiol.84-86 However, the precise factors and events responsible for orchestrating NK cell development within the BM remained elusive for decades. Long-term BM cultures that included stromal cells but lacked exogenous cytokines were able to differentiate low numbers of the NK cell lineage.87 Moreover, through the addition of recombinant (r) IL-2, NK cells were produced in cultures that lacked stromal cells,88 and when added to cultures containing stroma, rIL-2 produced NK cells with high efficiency.89-91 In addition, provision of rIL-2 to mice92,93 and humans94-98 in vivo results in an expansion of NK cells. However, the physiologic relevance of these IL-2 effects was a mystery during NK cell development because IL-2 is produced primarily by antigen-activated T cells located in the periphery,18 and mice deficient in IL-2 contain functional NK cells.99,100 In addition, mice101 and humans102 that lack the γc subunit of the IL-2R lack NK cells, as do mice103 and humans104 that lack the IL-2/15Rβ. Collectively, these data suggested that a factor other than IL-2 was produced in the BM and used signaling components of the IL-2R to induce NK cell development. Numerous studies from many laboratories have now shown convincingly that this factor critical for NK cell development is IL-15, acting through the IL-15Rαβγ. Two broad lines of evidence support this assertion: (1) experiments using in vitro models of human and murine NK cell differentiation and (2) genetically targeted mice with disruption of IL-2, IL-15, IL-2/15 receptors, their signaling components, or transcription factors that regulate gene expression critical to NK cell development (Table 1).
Summary of major phenotypes affecting immune cell compartments exhibited by mice with targeted disruption of IL-15, IL-15R components, IL-15R downstream signals, and transcription factors affecting IL-15 expression
| Mutation . | Major phenotypes . | References . |
|---|---|---|
| IL-15−/− | NK cells absent | 8 |
| NK-T cell deficiency (thymic and peripheral) | ||
| Memory CD8+ T-cell deficiency | ||
| i-IEL TCRγδ decreased | ||
| i-IEL CD8α α decreased | ||
| Decreased weight, cellularity of peripheral LN | ||
| IRF-1−/− (lacks inducible IL-15) | NK cells deficient, NK cell activity absent | 63, 64 |
| NK-T cell deficiency | ||
| i-IEL CD8α α deficient | ||
| IL-15Rα−/− | NK cells absent | 9 |
| NK-T cell deficiency (30% of wt) | ||
| Single-positive CD8+ T-cell deficiency (thymus) | ||
| CD8+ T-cell deficiency (periphery) | ||
| Memory CD8+ T-cell deficiency | ||
| TCRγδ i-IEL decreased 5- to 10-fold | ||
| IL-2/15Rβ−/− | NK cells absent | 56, 103, 179 |
| i-IELs (TCRα β, CD8α α, TCRγδ) reduced | ||
| NK-T cells deficient | ||
| DETCs absent | ||
| IL-2/15Rβ−/−→tgΔHIL-2/15Rβ | NK cells deficient | 118 |
| i-IEL TCRγδ deficient | ||
| IL-2/15Rβ−/−→tgΔAIL-2/15Rβ | NK cells normal | |
| i-IEL TCRγδ normal | ||
| Decreased induced NK cytotoxicity | ||
| γc−/− | NK cells deficient (greater than 350-fold reduction) | 101,119 |
| T and B cells deficient (10-fold reduction) | ||
| Jak3−/− (γc signal) | NK cells deficient | 120, 121 |
| DETCs absent | ||
| i-IEL TCRγδ deficient | ||
| STAT5a/b−/− (γcsignal) | NK cells deficient | 122 |
| STAT5b−/− (γc signal) | NK cell proliferation defect | 123 |
| NK cell cytotoxicity defect |
| Mutation . | Major phenotypes . | References . |
|---|---|---|
| IL-15−/− | NK cells absent | 8 |
| NK-T cell deficiency (thymic and peripheral) | ||
| Memory CD8+ T-cell deficiency | ||
| i-IEL TCRγδ decreased | ||
| i-IEL CD8α α decreased | ||
| Decreased weight, cellularity of peripheral LN | ||
| IRF-1−/− (lacks inducible IL-15) | NK cells deficient, NK cell activity absent | 63, 64 |
| NK-T cell deficiency | ||
| i-IEL CD8α α deficient | ||
| IL-15Rα−/− | NK cells absent | 9 |
| NK-T cell deficiency (30% of wt) | ||
| Single-positive CD8+ T-cell deficiency (thymus) | ||
| CD8+ T-cell deficiency (periphery) | ||
| Memory CD8+ T-cell deficiency | ||
| TCRγδ i-IEL decreased 5- to 10-fold | ||
| IL-2/15Rβ−/− | NK cells absent | 56, 103, 179 |
| i-IELs (TCRα β, CD8α α, TCRγδ) reduced | ||
| NK-T cells deficient | ||
| DETCs absent | ||
| IL-2/15Rβ−/−→tgΔHIL-2/15Rβ | NK cells deficient | 118 |
| i-IEL TCRγδ deficient | ||
| IL-2/15Rβ−/−→tgΔAIL-2/15Rβ | NK cells normal | |
| i-IEL TCRγδ normal | ||
| Decreased induced NK cytotoxicity | ||
| γc−/− | NK cells deficient (greater than 350-fold reduction) | 101,119 |
| T and B cells deficient (10-fold reduction) | ||
| Jak3−/− (γc signal) | NK cells deficient | 120, 121 |
| DETCs absent | ||
| i-IEL TCRγδ deficient | ||
| STAT5a/b−/− (γcsignal) | NK cells deficient | 122 |
| STAT5b−/− (γc signal) | NK cell proliferation defect | 123 |
| NK cell cytotoxicity defect |
tgΔH indicates transgenic for IL-2/15Rβ with deletion of the cytoplasmic H region; tgΔA, transgenic for IL-2/15Rβ with deletion of the cytoplasmic A region; and LN, lymph node.
IL-15 differentiates human NK cells in vitro.
First, for IL-15 to be the major physiologic growth factor responsible for NK cell ontogeny, it must be expressed at the anatomic site of NK cell differentiation, the BM. In support of this, the human IL-15 cDNA was first cloned from the IMTLH BM stromal cell line.1Mrozek et al52 directly demonstrated that primary human BM stromal cells produced IL-15 at the transcript and protein levels, while lacking any expression of IL-2. Further, a 3-week culture of CD34+ hematopoietic progenitor cells (HPCs) supplemented with rIL-15 induced the differentiation of functional CD56+NK cells in the absence of stroma or other cytokines. The CD56+ NK cells generated in these cultures lysed MHC class I tumor targets, produced cytokine and chemokines upon stimulation, and expressed cytoplasmic CD3-ζ chain protein similar to mature peripheral blood NK cells.52
Two additional BM stromal cell factors, ligands for the class III receptor tyrosine kinases (RTKs) c-kit (c-kit ligand, KL) and flt3 (flt3 ligand, FL), have been shown to potentiate the expansion of other hematopoietic cell lineages, usually in combination with a lineage-specific growth factor.105 KL or FL alone induces no NK cell differentiation, but when combined with IL-15, each of these factors potentiated IL-15–induced expansion of NK cells from CD34+ HPCs.52,106 Subsequent studies demonstrated that culture of CD34+ HPCs in FL or KL increased the NK cell precursor frequency, as determined by limiting dilution analysis. What was the mechanism whereby the RTK ligands FL and KL increased NK cell precursor frequency? Culture of CD34+ BM HPCs in FL or KL alone induced a population of CD34brightIL-2/15Rβ+ cells after 10 days, and cell sorting experiments showed that these CD34brightIL-2/15Rβ+ cells have a 65- to 200-fold higher NK cell precursor frequency compared with freshly isolated CD34+ HPCs. FL and KL also increased expression of IL-15Rα mRNA within CD34+ HPCs measured by reverse transcriptase polymerase chain reaction (RT-PCR). Thus, human NK cell development can be divided into an early phase in which an NK progenitor cell responds to early-acting stromal cell growth factors (eg, FL or KL) and develops into an NK cell precursor intermediate with the basic phenotype CD34brightIL-2/15Rβ+CD56−. This NK precursor is then responsive to IL-15 for maturation into a functional CD56+ NK cell (Figure3).106
Schematic diagram of human NK cell development.
NK cell progenitors that respond to early-acting RTK ligands (FL and KL) differentiate into IL-15–responsive NK cell precursors by up-regulating the IL-15R complex on their surface. The NK precursors then respond to IL-15 to differentiate into mature NK cells. Characterization of the resultant CD56bright NK cells produced strongly suggests that other (eg, stromal) signals are likely required for complete NK cell differentiation. FL−/− mice are deficient in NK cells, suggesting that this RTK ligand serves a critical, nonredundant function in NK cell development or expansion in mice in vivo, most likely at the level of the NK cell progenitor.285 In addition, RAG2/γc−/− mice (lacking T, B, and NK cells) reconstituted with c-kit−/− progenitors have defects in NK cell expansion and survival, suggesting that KL serves a critical role in these functions in vivo.286 Further, IL-15Rα−/− and IL-15−/− mice lack NK cells, suggesting that IL-15 is critical for the differentiation of mature NK cells from NK cell precursors (Table 1).
Schematic diagram of human NK cell development.
NK cell progenitors that respond to early-acting RTK ligands (FL and KL) differentiate into IL-15–responsive NK cell precursors by up-regulating the IL-15R complex on their surface. The NK precursors then respond to IL-15 to differentiate into mature NK cells. Characterization of the resultant CD56bright NK cells produced strongly suggests that other (eg, stromal) signals are likely required for complete NK cell differentiation. FL−/− mice are deficient in NK cells, suggesting that this RTK ligand serves a critical, nonredundant function in NK cell development or expansion in mice in vivo, most likely at the level of the NK cell progenitor.285 In addition, RAG2/γc−/− mice (lacking T, B, and NK cells) reconstituted with c-kit−/− progenitors have defects in NK cell expansion and survival, suggesting that KL serves a critical role in these functions in vivo.286 Further, IL-15Rα−/− and IL-15−/− mice lack NK cells, suggesting that IL-15 is critical for the differentiation of mature NK cells from NK cell precursors (Table 1).
It is important to note that the NK cells resulting from adult CD34+ HPCs in stroma-free cultures with IL-15 are CD56+, lyse tumor target cells, and produce immunoregulatory cytokines and chemokines upon stimulation. However, these NK cells have high-density expression of CD56, closely resembling the minor CD56bright NK cell population in peripheral blood, as they have little surface expression of CD16, with most cells expressing C-type lectin CD94/NKG2 NK receptors (NKR) and only small (1% to 8%) percentages of cells expressing killer-cell immunoglobulin-like receptor (KIR).106 This suggests that other soluble or cell-contact signals, perhaps from BM stroma, are required for normal KIR acquisition and other CD56dim NK characteristics, or alternatively the CD56dim NK cell may have a different precursor. To address these issues, further experiments are needed comparing IL-15–based culture systems using various starting HPC populations, with and without autologous BM stroma (or other MHC class I interaction systems).
Additional human culture systems have also supported a central role for IL-15 in human NK cell development from various starting progenitor populations, including cord blood CD34+,107,108 adult BM CD34+,108 fetal liver CD34+CD38±,109 and thymocyte T/NK progenitors.110 Beginning with CD56−CD16+ cord blood cells, Gaddy and Broxmeyer111 have demonstrated that IL-15 induced the maturation of these cells into highly lytic, phenotypically mature NK cells. Collectively, these in vitro human culture systems demonstrate a central role for IL-15 in the later stages of NK cell development from various adult and fetal progenitors. Further studies are needed to clarify how IL-15 acts in concert with signals from early-acting growth factors and stromal cells to facilitate physiologic human NK cell development and normal NK cell repertoire acquisition. The basic understanding of how human NK cells develop can also be directly translated to optimizing the ex vivo112 and in vivo expansion of this lymphocyte subset for therapeutic intervention.
IL-15 differentiates murine NK cells.
In vitro murine culture systems have also demonstrated a critical role for IL-15 during NK cell ontogeny. Leclercq et al showed that bipotential T/NK progenitors113 isolated from the thymus selectively differentiated into NK cells in the presence of IL-15.53 Addition of high concentrations of IL-15 to progenitors in fetal thymic organ cultures (FTOCs) blocked TCRαβ T-cell development and shifted differentiation toward the NK cell lineage.53 A series of studies by Kumar and colleagues examined the role of IL-15 during murine NK cell ontogeny from adult BM progenitors.114 First, Puzanov et al115 demonstrated that IL-15 corrected the lytic defect of immature NK1.1+ cells within mice rendered osteopetrotic by β-estradiol treatment. This suggested that IL-15 may replace the BM microenvironment deficits resulting in such immature NK cells.115 Williams et al116 established a murine stroma-free culture system in which an NK progenitor population (c-kit+Sca2+Lin−IL-2/15Rβ−) cultured in IL-6/IL-7/KL/FL differentiated into an NK cell precursor population (NK1.1−IL-2/15Rβ+), which in turn responded to IL-15 for differentiation into mature, lytic NK1.1+ NK cells.
Overall, there are strong parallels between human106 and murine116 117 models of NK cell differentiation because both involve NK progenitors that respond to early-acting cytokines (eg, FL and KL) and NK precursors that express the IL-2/15Rβ and respond to IL-15 for mature NK cell development. In both systems, there is abnormal NK receptor repertoire development in the presence of IL-15 alone, suggesting that other signals, as discussed earlier, are required for proper NKR acquisition.
Mice with targeted genetic alterations demonstrate that IL-15 is a critical NK cell differentiation factor in vivo.
As introduced earlier, the phenotypes of mice with targeted disruption of IL-2, IL-2Rα, and γc first suggested that cytokines other than IL-2, acting through IL-2R components, may be important for NK cell development. After the identification and cloning of IL-15, the aforementioned in vitro studies provided the first evidence that IL-15 could indeed serve as the central physiologic NK cell hematopoietic factor. Consequently, additional gene-targeting experiments in mice have confirmed this postulate at the level of the whole animal (Table1). Mice with targeted disruption of the IL-2/15Rβ, shared only by IL-2 and IL-15, have a dramatic reduction in peripheral NK1.1+CD3− cells and an absence of NK cytotoxicity in vitro.103 In addition, Fujii et al118 recently demonstrated that the IL-2/15Rβ H-region, which activates STAT5/STAT3, selectively affects the development of NK and γδ T cells through reconstitution of IL-2/15Rβ−/− mice with IL-2/15Rβ transgenes containing specific mutations in the cytoplasmic domain. Mice that have genetic disruption of the γc have multiple lymphoid defects, including a dramatic decrease in NK cells.101,119Consistent with these models, mice that have disrupted signaling components that operate downstream of IL-15R, such as Jak3−/−, STAT5a/b−/−, or STAT5b−/−, also have NK cell defects.120-123
Mice with disruption of the IRF-1 gene fail to induce IL-15 in the BM and have NK cell deficiency.63,64 Progenitor cells from IRF-1−/− mice develop into functional NK cells upon culture in IL-15 or transfer into lethally irradiated wild-type mice, suggesting that IRF-1 is required for the expression of IL-15 in the BM microenvironment. Indeed, IRF-1–binding sites have been identified in the 5′ regulatory region of the IL-15 gene, supporting this hypothesis.63 At present, it is unclear what provides the endogenous signal to activate IRF-1 within BM stromal cells, which in turn induces the IL-15 expression important for NK cell development.
Mice with targeted disruption of the Ets-1 transcription factor were shown to have a selective deficit of NK cells.124Ets-1−/− mice do not appear to have defects in IL-15Rαβγ, IL-15, or IL-2 expression, leaving the precise mechanism responsible for this NK cell deficiency unknown. Because Ets-1 is expressed in mature NK cells, it is possible that upstream IL-15–derived signals may induce Ets-1 that may then orchestrate the expression of an NK cell genetic program. Further investigation into the genetic changes at the molecular level during NK cell differentiation will help to clarify the gene programs activated during NK cell ontogeny and the transcription factors involved in this process.
Lodolce et al9 recently generated mice with targeted disruption of the IL-15Rα, providing direct evidence that the IL-15/IL-15Rαβγ system is critical for murine NK cell development. These mice contain multiple defects in innate immune effectors, including an absence of splenic NK cells and NK cytotoxic activity. Moreover, IL-15−/− mice also lack any phenotypic or functional NK cells in the spleen and liver, a defect that is reversible upon administration of exogenous IL-15 for 1 week.8 Exogenous IL-15 treatment of normal mice increases NK cell activity and both the percentage and absolute number of splenic NK cells.8,125,126 Transgenic mice that overexpress murine IL-15 have been generated and demonstrate a striking early expansion in NK cells.68 Thus, in vivo evidence demonstrates that IL-15 is requisite for murine NK cell development, and exogenous IL-15 supports the differentiation of human NK cells in BM culture systems. These basic observations provide invaluable insight into the critical, nonredundant role of IL-15 during NK cell development and suggest the potential utility of IL-15 therapy to expand NK cells in patients.
IL-15 activates NK cell proliferation, cytotoxicity, and cytokine production and regulates NK cell/macrophage interaction
NK cells constitutively express cytokine receptors and produce abundant cytokines and chemokines during the early, innate immune response to infection. Such NK cell–derived immunoregulatory factors may be vital in the orchestration of the innate immune response, as well as influence the developing adaptive response.73,78,127 NK cells constitutively express IL-2/15Rβγc, but the lack of abundant IL-2 during the early innate immune response prompted us to investigate the role of IL-15 as the more important physiologic ligand for NK cell proliferation, cytotoxicity, and cytokine production in this setting. The majority (approximately 90%) of human NK cells have low-density surface expression of CD56 (CD56dim), express high surface density of CD16 (FcγRIII), and have a low proliferative capacity. CD56bright NK cells represent a minor subset (approximately 10%) of human NK cells that are low or negative for CD16 and are capable of high proliferation.75
NK cell proliferation and cytotoxicity.
IL-15 induced the proliferation of CD56bright NK cells in a dose-dependent fashion to a similar extent as IL-2, yet required a nanomolar concentration to activate the IL-2/15Rβ for proliferative activity.7 However, picomolar amounts of IL-15 were effective at maintaining NK cell survival in serum-free media.71 IL-15 was found to activate cytotoxicity and antibody-dependent cellular cytotoxicity (ADCC) by sorted CD56bright and CD56dim human NK cell subsets.7 Incubation of purified, resting CD56dim NK cells with IL-15 resulted in significant, dose-dependent increases in lymphokine-activated killing activity against the NK-resistant COLO 205 cell line and ADCC against the P815 murine mastocytoma cell line. IL-15 and IL-2 induce nearly identical levels of cytotoxicity, and both depend upon signals through the IL-2/15Rβ, as enhanced NK activity was abrogated in the presence of an anti–IL-2/15Rβ MoAb.7 Infection of human PBMCs with herpesviruses resulted in endogenous IL-15–dependent increases in NK cell cytotoxicity, suggesting that IL-15 participates in the normal innate host defense against viral infections.128 129
IL-15 costimulates NK cell cytokine and chemokine production and regulates interactions between macrophages and NK cells.
IL-15 acts in concert with IL-12 to induce the macrophage-activating factors IFN-γ and tumor necrosis factor (TNF)-α,7,130,131 whereas IL-15 alone appears to be a potent stimulus for GM-CSF production7,132 by resting CD56+ human and murine133 NK cells. Interestingly, human CD56bright NK cells stimulated with IL-15 plus IL-12 produce approximately 10-fold greater amounts of IFN-γ, TNF-α, and GM-CSF protein compared with an equal number of CD56dim NK cells132 (and our unpublished observations). Thus, the CD56bright NK cell may have a unique biologic role in the production of immunoregulatory cytokines within the innate immune system.
Macrophages activated with LPS, IFN-γ, mycobacteria, Toxoplasma gondii, C neoformans, and Salmonella have been shown to express IL-15.1,48,49,134,135 In human cocultures of LPS-stimulated macrophages and NK cells, endogenous IL-15 produced by the activated macrophages, working in concert with IL-12, was shown to be critical for optimal IFN-γ production by human NK cells.48 Similarly, in vitro culture of LPS-activated severe combined immunodeficiency (SCID) mouse splenocytes (NK cells and macrophages) produced abundant IFN-γ protein, which was abrogated by blocking the IL-2/15Rβ or neutralizing IL-15.133 In vivo, preadministration of either an antibody that blocks the IL-2/15Rβ or a neutralizing anti–IL-15 antiserum to SCID mice resulted in a significant reduction in serum IFN-γ measured in vivo 6 hours after an LPS challenge.133 Therefore, in both mice and humans, activated macrophages and NK cells interact through a paracrine feedback loop, with macrophages producing monokines (eg, IL-15 and IL-12) that bind to surface receptors constitutively present on NK cells, resulting in the production of macrophage-activating factors (eg, IFN-γ). NK cell–derived macrophage-activating factors in turn feed back upon the macrophages to further augment their activation (Figure 4). Thus, macrophage-derived IL-15 contributes with other monokines (especially IL-12) to the proinflammatory cascade leading to innate immune IFN-γ production. Additionally, Ross and Caligiuri130demonstrated that continuous stimulation of CD56+ NK cells with IL-15 + IL-12 in vitro results in NK cell apoptosis mediated through an autocrine TNF-α–dependent mechanism, initiated after 24 hours of monokine stimulation. This may represent one means whereby the innate immune system limits itself after prolonged activation.130
IL-15 participates in innate immune cross-talk between activated monocytes/macrophages and NK cells.
After an infectious insult (1), macrophages produce monocyte-derived cytokines (monokines) (2), including IL-15, that bind to constitutively expressed monokine receptors on NK cells. Monokine-stimulated NK cells in turn produce cytokines that activate the macrophage (3), including IFN-γ, allowing the macrophage to clear the offending pathogen and stimulating further monokine production.
IL-15 participates in innate immune cross-talk between activated monocytes/macrophages and NK cells.
After an infectious insult (1), macrophages produce monocyte-derived cytokines (monokines) (2), including IL-15, that bind to constitutively expressed monokine receptors on NK cells. Monokine-stimulated NK cells in turn produce cytokines that activate the macrophage (3), including IFN-γ, allowing the macrophage to clear the offending pathogen and stimulating further monokine production.
NK cells also produce the C-C chemokines macrophage inflammatory protein (MIP)-1α and MIP-1β after stimulation with IL-15, which is augmented with the addition of IL-12.131,136,137Because C-C chemokines also serve as chemoattractants for NK cells,138 IL-15 + IL-12–induced MIP-1α and MIP-1β production may be one mechanism for proper trafficking of additional NK cells to the site of infectious insult. In addition, chemokine production may have implications in the interactions between macrophages and NK cells, as MIP-1α has been shown to potentiate IFN-γ–inducible secretion of inflammatory cytokines by macrophages such as IL-1β.139 Further, NK cells costimulated with IL-15 + IL-12 produce soluble factors (including C-C chemokines) that inhibit human immunodeficiency virus (HIV)-1 replication in vitro.137 The cytokine and chemokine profiles produced by human NK cells in response to monokines IL-15 + IL-12 were recently compared with those induced by monokines IL-18 + IL-12.132 Alone, IL-18, IL-15, or IL-12 induced little or none of the cytokines examined, with the exception of IL-15–induced GM-CSF, MIP-1α, and MIP-1β. IL-18 + IL-12 induced extremely high amounts of IFN-γ by CD56+ NK cells, with the majority produced by the CD56bright NK cell subset. IL-15 + IL-12 induced moderate amounts of IFN-γ but was also the optimal stimulus for IL-10, TNF-α, GM-CSF, MIP-1α, and MIP-1β. This suggests that NK cell cytokine production may be governed in part by the monokine milieu (including IL-15) induced during the early pathogen-dependent response to infection, as well as the NK cell subset present at the site of inflammation.132
As described earlier, there is now in vitro and in vivo evidence for IL-15's participation in early innate immune cytokine responses, especially those resulting in IFN-γ production by NK cells. Thus, IL-15 acts as a costimulator of IFN-γ production by NK cells and may therefore be important in the control of infections that require IFN-γ for clearance.77 Additional in vivo studies of IL-15's role during such infections may yield information to direct therapies aimed at boosting the immune response to infection or decreasing improper immune activation or inflammation. Because mice genetically targeted to delete functional IL-15 or IL-15Rα gene products concurrently lack NK cells,8 9 it will be difficult to assess the role of IL-15 during the innate immune response in these models. Use of experimental systems that neutralize IL-15 will be important to complement such IL-15/IL-15R knockout mice.
IL-15 and uterine NK cells.
In mice, the metrial gland is a uterine tissue that develops adjacent to the placenta and contains granulated metrial gland cells that are phenotypically and functionally uterine NK cells.140Similar NK-like cells have also been identified in the human uterus and have the phenotype CD56brightCD16−.141,142 These NK cells are located at the maternal/fetal junction and are thought to play a role in regulating implantation and trophoblast invasion, but the factors governing their localization or differentiation are unclear.143 Uterine NK cells express IL-15R components, and IL-15 increases the expression of NK cytolytic mediators (perforin and granzymes) in pregnant uterine tissue explanted in vitro,144 as well as in primary mouse uterine NK cells.145 Moreover, IL-15 (but not IL-2) was detected in uterine macrophages, amnion, chorion, and decidual cells, suggesting a possible source of IL-15 during pregnancy.144,146,147IL-15 expression was shown to peak in the midsecretory phase of normal human menstruation and was up-regulated during progesterone-induced decidualization.148 Because IL-15 costimulates blood NK cell cytokine production, IL-15 may also be involved in cytokine production by uterine NK cells, which have been proposed to regulate placental changes during pregnancy.143 Thus, IL-15 and IL-15R components are expressed in murine and human uterine tissues and may play a role in the differentiation or homeostasis of specialized uterine NK cells. Further studies may illuminate potential roles for abnormal IL-15/IL-15R expression during pathologic pregnancies.
IL-15 regulation of monocytes/macrophages and granulocytes
Human macrophages express high-affinity binding sites for IL-15 that are up-regulated upon activation with LPS.28Monocytes have been shown to express the IL-2/15Rβ,149γc,150 and the IL-15Rα,30suggesting the possibility for IL-15 to act in an autocrine fashion. Human monocytes treated with IL-15 (10-1000 ng/mL) produced IL-8 and macrophage chemotactic protein (MCP)-1 that was chemotactic for neutrophils and monocytes, respectively.69 Alleva et al151 demonstrated autocrine IL-15 regulation of macrophage proinflammatory cytokine production that was highly dependent upon the concentrations of IL-15 available to the macrophage. Extremely low (picomolar to attomolar) concentrations of IL-15 suppressed macrophage proinflammatory (TNF-α, IL-1, IL-6) cytokine production, but at high concentrations it enhanced the production of these mediators.
Human neutrophils express the IL-2Rβ and γc subunits of the IL-2/15R complexes,152-154 as well as IL-15Rα.155,156 IL-15 activates human neutrophils, with effects including morphologic changes, increased phagocytosis, increased de novo RNA and protein synthesis,157 delayed apoptosis, and stimulation of the growth-inhibitory effects of neutrophils against Candida albicans.155Overall, these studies further suggest that IL-15 may have a role in establishing innate immune responses and maintaining neutrophil-mediated inflammatory processes. However, defects in these cell types were not reported in IL-15Rα−/− or IL-15−/− mice, suggesting that IL-15/IL-15R interactions are not critical to their development or expansion.8 9
IL-15 plays a role in the development, homeostasis, and activation of TCRγδ dendritic epidermal T cells, intestinal intraepithelial lymphocytes, and NK-T cells
Because IL-15 binds to and signals through the shared IL-2/15Rβγc, cell types that respond to ligation of these receptors with IL-2 were logical potential targets for IL-15. In addition to NK cells, several innate immune T-cell populations have been shown to express the IL-2/15Rβ or the γc. These include dendritic epidermal TCRγδ T cells (DETCs), intestinal intraepithelial lymphocytes (i-IELs), and NK1+ T cells (NK-T cells).
DETCs are a skin-specific member of the TCRγδ T-cell population that migrate to the skin during fetal life in mice.158 The DETC population in skin was absent after treatment with anti–IL-2/15Rβ in utero,159 yet were present in normal numbers in IL-2−/− mice.160 Further, Vγ3 DETCs are absent in IL-2/15Rβ−/− mice56 and γc−/− mice.119 IL-15 (but not IL-2) expression was detected in fetal skin during the time frame that DETCs traffic to the skin microenvironment.56Thy-1+ murine DETCs proliferated in response to IL-15 after activation with mitogens that induced IL-15R components.161 When low concentrations of exogenous IL-15 were added to NK/T progenitors in alymphoid FTOCs, the greatest expansion occurred in the Vγ3 DETC compartment.53 The status of Vγ3 DETCs was not reported in IL-15Rα−/− or IL-15−/− mice.8 9 Collectively, these studies suggest that IL-15 is critical to DETC growth and survival after activation and may be important in selective localization of these cells in the skin.
I-IELs consist of both TCRαβ and TCRγδ T cells located at the basolateral surfaces of intestinal epithelial cells and are thought to play a key role in mucosal immunity.162,163 TCRγδ i-IELs express the CD8αα homodimer, whereas TCRαβ express CD8αβ, CD8αα, or CD4.164Thy-1CD8αα+ i-IELs are thought to develop extrathymically and express the IL-2/15Rβγc receptor components, yet are able to proliferate in an IL-2–independent fashion. Thy-1+CD8αβ+ or CD4+i-IELs are thought to depend on the thymus for development.165 166
TCRγδ i-IELs were shown to express IL-15Rα mRNA and to proliferate in response to IL-15, and IL-15 protected these cells against growth factor deprivation–induced apoptosis through the up-regulation of Bcl2.167Listeria monocytogenes infection of rats resulted in increased IL-15 mRNA within intestinal epithelial cells that correlated with i-IEL accumulation and IFN-γ production.168 Further, mice with targeted disruption of the IL-2/15Rβ103 or γc119 have a dramatic reduction of TCRγδ and TCRαβ/CD8αα i-IELs. Mice deficient in IRF-1 (IRF-1−/−) fail to induce IL-15 expression and exhibit a similar deficit in CD8αα i-IELs.64 A definitive demonstration of the requisite IL-15/IL-15R complex participation in the development of CD8αα i-IELs was provided by mice with targeted disruption of the IL-15Rα and IL-15. IL-15Rα−/− mice had a 2-fold reduction in total i-IELs and a 5- to 10-fold reduction in TCRγδ CD8αα i-IELs.9 IL-15−/− mice had a 2-fold decrease in total i-IEL numbers, a 2-fold increase in the ratio of TCRαβ to TCRγδ i-IELs, and a dramatic reduction in TCRαβCD8αα i-IELs.8 Recent work by Lai et al169 suggests that IL-15 plays a role in TCRαβ i-IEL survival in the absence of antigen stimulation, as well as in their expansion and survival in the presence of antigen. IL-15 also stimulates the proliferation, cytotoxicity, and IFN-γ production by human TCRγδ IELs.170 Thus, IL-15 plays a critical role in the expansion and function of i-IEL and DETC cells, thereby contributing to mucosal immune defense. Whereas IL-15Rα−/− and IL-15−/− mice demonstrate changes in DETC and i-IEL TCRγδ T cells, there are no apparent numeric or phenotypic defects in other TCRγδ compartments.8,9 However, these results do not preclude a role for IL-15 in TCRγδ proliferation and cytokine production in response to infectious pathogens.134 171-173
Murine T cells that exhibit a restricted TCR repertoire (invariant Vα14 with Vβ8, 2, or 7) that coexpress NK1.1 and TCRαβ have been defined as NK1+ T cells (or NK-T cells).174,175 Analogous NK-T cells have also been described in humans.176-178 Similar to NK cells, NK-T cells lyse MHC class I and YAC-1 target cells; express NK1.1, NKRs, and the IL-2/15Rβ; and are readily detectable in athymic mice. Murine NK-T cells proliferate in response to IL-15, and their numbers are severely reduced in IL-2/15Rβ−/−, IRF-1−/−, IL-15Rα−/−, and IL-15−/− mice,8,9,64,179 yet are normal in IL-2−/− mice.179,180 The few NK-T cells present in IL-15−/− mice underwent normal thymic selection, suggesting that IL-15 is important for the expansion, survival, or functional maturation of committed NK-T cells.8 Therefore, NK-T cells depend upon IL-15/IL-15R complex-mediated signals for expansion and homeostasis, in contrast to NK cells, which appear to have an absolute requirement for IL-15/IL-15R for development.
Function of IL-15 on TCRαβ T cells
IL-15 was first identified as a T-cell growth factor through its ability to promote the proliferation of CTLL cells and mitogen-stimulated T cells in a fashion similar to that of exogenous IL-2.1,2 Of note, resting T cells do not appear to respond to IL-15, and it is likely that TCR ligation induces the expression of IL-15Rα, conferring responsiveness to IL-15. Such action on T cells suggests that IL-15 expressed by APCs may be important for the early activation of T cells at sites of inflammation immediately after TCR ligation. Stimulation of TCR-engaged T cells with IL-15 has been shown to induce various activation antigens, such as IL-2Rα (CD25), IL-2/15Rβ (CD122), FasL (CD95), CD30, TNFRII, CD40L, CD69, and CD94/NKG2A,181-185 while down-regulating the IL-15Rα.186 The in vitro proliferation of resting T lymphocytes in response to anti-CD3 plus IL-15 was greatly reduced in IL-15Rα−/− lymphocytes compared with wild type, supporting the idea that IL-15 requires induction of the IL-15Rα to optimally stimulate resting T cells. Further, IL-15Rα−/− T cells showed a lower response to CD3 ligation plus IL-2, suggesting that IL-15Rα may be important for the induction of IL-2Rα and hence responsiveness to IL-2.9IL-15 also protected concanavalin A–activated human T lymphoblasts from undergoing apoptosis after Fas or CD3 cross-linking or treatment with dexamethasone in vitro and in vivo.187
IL-15 acts as a potent chemoattractant for T cells isolated from human blood.188 This observation has led to a number of studies examining the role of IL-15 during chronic inflammatory and autoimmune diseases, such as rheumatoid arthritis (see below). IL-15Rα−/− mice have defects in T-cell homing to peripheral lymph nodes, providing additional evidence that IL-15 has a physiologic role in T-cell trafficking in vivo.9 IL-15 may also operate through indirect mechanisms, such as chemokine production189 and activation of human endothelial cell expression of hyaluronan,190 to regulate T-cell trafficking.
Jonuleit et al51 demonstrated that unstimulated human dendritic cell (DC) cultures produced low levels of IL-15 protein that were detectable by enzyme-linked immunosorbent assay and CTLL bioassay, and stimulated DC supernatants were shown to be chemoattractant for T cells. The production of IL-15 protein after phagocytosis51 or CD40 ligation191 provides an intriguing mechanism for initial attraction and stimulation of T cells in the absence of IL-2, as may be the case for other APCs such as macrophages.1,48,49 192
IL-15 stimulated the proliferation of human memory (CD45RO+) CD4 and CD8 and naive (CD45RO) CD8+human T cells in vitro, while having no effect on naive CD4 T lymphocytes, consistent with IL-2/15Rβ expression.181Zhang et al72 documented selective high IL-2/15Rβ expression on CD44hiCD8+ memory T cells in mice, and IL-15 selectively stimulated this cell type both in vitro and in vivo. Further, in mice transgenic for the LSP–IL-15 cDNA22 or IL-2SP–IL-1568 under the control of an MHC class I promoter, CD44hiLy-6C+CD8+ memory-phenotype T cells were increased in peripheral lymphoid tissues. IL-15Rα−/− mice have a selective deficit in CD8+ T-cell numbers in both the thymus and periphery.9 Specifically, thymic CD8+single-positive and peripheral CD8+CD44hi and CD44int lymphocytes were reduced. IL-15−/−mice have reduced numbers of memory-phenotype CD8+ T cells in the spleen and lymph nodes that were reversible upon provision of exogenous IL-15.8 Because IL-15−/− mice had normal numbers of single-positive CD8 thymocytes, IL-15 may not be requisite for the development of CD8+ T cells but may be critical for their expansion or survival.8 The subtle differences in the thymic CD8 single-positive cells between IL-15Rα and IL-15 knockout mice warrant additional investigation. IL-15−/− mice maintained good health when housed under specific pathogen-free conditions; however, they demonstrated a dramatic lethal sensitivity to vaccinia virus infection compared with control mice.8 Because both NK cells and CD8+T cells are important for protection against vaccinia, failure to mount a protective host response is likely due to the deficiencies in these lymphocyte populations. Examining IL-15−/− mice in various models of infectious disease may provide novel information about the requirement for these cell types in host defense.
Most reports support the classification of IL-15 as a proinflammatory type-1 cytokine,193-198 whereas a few have observed IL-15 as a costimulator of type-2 cytokines.47,199,200 When IL-15 has been used as an adjuvant to vaccination, a type-1 cytokine profile and increased IFN-γ production have been documented.193,195-197 The addition of exogenous IL-15 favored human Th1 T-cell differentiation in vitro,198 as well as in murine Th1 clones costimulated with IL-15 and IL-12.194 Furthermore, IL-15 has been shown to costimulate innate immune IFN-γ production, potentially shifting subsequent adaptive T-cell responses toward Th1.7,48,132 133 It will be interesting to definitively study the role of IL-15 in Th-cell differentiation at the level of the whole organism by using IL-15−/− and IL-15Rα−/− mice, as well as reagents that neutralize IL-15 in wild-type mice.
Function of IL-15 on nonimmune cells
IL-15 expression has been detected in numerous tissues, many of which are not sites of immune responses, indicating the potential for additional nonimmune functions.1 Indeed, IL-15 also affects cells outside of the immune system. IL-15 serves as an anabolic agent for skeletal muscle201 and may support muscle cell differentiation.202 Intestinal epithelial cells signal and proliferate in response to IL-15 in vitro.58 Vascular endothelial cells express IL-15Rαβγ mRNA and respond to IL-15 with intracellular signals, and IL-15 induced angiogenesis in vivo.203 However, IL-15Rα and IL-15−/−mice do not appear to have defects in muscle, bone, or vasculature, suggesting that IL-15 is not critical to the development or function of these nonimmune tissues.8 9 IL-15's broad pleiotropic effects on multiple tissues and cell types outside of the immune system are unusual for a cytokine, and further understanding of how IL-15 may affect nonimmune cells could provide information relevant to the design of potential therapeutic applications.
Relevance of IL-15 to human disease
Role of IL-15 in autoimmune and inflammatory disease
Rheumatoid arthritis.
Rheumatoid arthritis (RA) is a chronic degenerative condition of synovial membranes that is thought to be mediated in part by aberrant cytokine regulation that ultimately results in abnormally high levels of proinflammatory cytokines, such as TNF-α, within the joints. Current hypotheses suggest that abnormal T-cell trafficking to the joints may be a key early step in this process.204 On the basis of work describing IL-15 as a potent T-cell attractant,188 McInnes et al205 suggested that IL-15 may play a primary role in the development of RA. IL-15 protein was demonstrated in the synovial fluids and synovial membranes of patients with active RA. Synovial fluids were found to promote the chemoattraction and activation of T cells, which were partially abrogated by the addition of anti–IL-15 antibodies. In addition, injection of a single dose of IL-15 resulted in a lymphocytic inflammatory infiltrate in vivo.206
The presence of multiple chemoattractants in synovial fluid, including IL-15, IL-8, MCP-1, and MIP-1α, suggests some redundancy in the factors responsible for T-cell extravasation into RA synovial membranes.205,207 Indeed, recent work has also documented a role for IL-17208,209 and IL-18210 in the pathophysiology of this disease, highlighting the complexity of the cytokine cascades at work in RA. Subsequent studies also demonstrated that IL-15–activated T cells from RA patients stimulated macrophage cell lines and primary monocytes/macrophages to produce TNF-α in vitro.206 This effect was cell-contact dependent, and antibodies to CD69, lymphocyte function-associated antigen (LFA)-1, and intercellular adhesion molecule (ICAM)-1 inhibited the T-cell–induced production of TNF-α by macrophages. An increased expression of IL-15 protein in the synovium of RA in comparison with osteoarthritis patients has also been documented.211 In the mouse, administration of soluble IL-15Rα prevents collagen-induced arthritis, suggesting that development of effective IL-15–blocking agents such as soluble receptors or MoAbs may be useful in the treatment of RA.212
Sarcoidosis.
Sarcoidosis is a chronic granulomatous condition of unclear etiology that progressively affects multiple organs, especially the lungs.213 Agostini et al214 suggested a potential role for IL-15 during the pathogenesis of pulmonary sarcoidosis because alveolar macrophages isolated from patients with active sarcoidosis expressed IL-15 mRNA and cytoplasmic or membrane IL-15 protein, whereas patients with inactive disease or normal donors did not. In addition, CD4+ T cells isolated from bronchoalveolar lavage of patients with active sarcoidosis expressed components of the IL-2/15R complexes and proliferated in response to IL-15, suggesting that macrophages may provide a proliferative signal to T cells in the lungs during this disease process.214
Inflammatory bowel disease.
Two major types of inflammatory bowel disease (IBD) commonly occur, ulcerative colitis (UC) and Crohn disease (CD), and are thought to represent inappropriate chronic inflammatory processes.215Kirman and Nielsen216 demonstrated that patients with UC or severe CD had an increased percentage of PBMCs that expressed IL-15 protein, which was decreased after successful symptomatic treatment. Serum IL-15 was detectable in several patients with UC with moderate to severe disease (5 of 8 cases; range, 0-490 pg/mL), but was not detectable in CD patients or normal donors. In vitro, LPS activation of UC or CD patients' PBMCs resulted in further increases in intracellular IL-15 protein levels.216 IL-15 protein was detected from supernatants of rectal mucosal biopsy specimens, and IL-15 mRNA was detected in macrophages and epithelial cells by in situ hybridization from patients with active CD or UC, but not from healthy controls. Further, lamina propria mononuclear cells from IBD patients proliferate in response to rIL-15.217 Recent studies have confirmed IL-15 protein production by macrophages in the mucosa of patients with IBD and provided evidence for T-cell modulation by IL-15 in this setting.218 These studies suggest that IL-15 released during chronic bowel inflammation may contribute to the pathogenesis of UC, and possibly CD.
Other autoimmune or inflammatory diseases.
Increased production of IL-15 during several other chronic inflammatory conditions has also been observed, including hepatitis C–induced liver diseases and multiple sclerosis.219-221 Elevated levels of serum IL-15 protein have been measured in hepatitis C virus–infected patients with chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma as compared with asymptomatic carriers and healthy controls.219 The highest levels of IL-15 were found in patients with hepatocellular carcinoma, who had significantly higher IL-15 levels compared with all other groups studied (n = 11; mean ± SD, 77.4 ± 78 pg/mL; P < .05). Treatment with IFN-α resulted in resolution of liver inflammation measured by transaminase levels, concurrent with suppression of serum IL-15 levels.
Multiple sclerosis (MS), an inflammatory disease of the central nervous system, is thought to have an etiology involving autoimmunity and cytokine dysregulation.222 Patients with MS were found to have higher numbers of IL-15 mRNA–expressing blood mononuclear cells compared with patients with aseptic meningoencephalitis (P < .02) or healthy controls (P < .01).220 Increased numbers of IL-15 mRNA–expressing cells were found in the central nervous system compared with the blood in MS patients. In addition, patients with chronic-progressive MS had higher IL-15 expression than those with relapsing-remitting MS. Another study confirmed this finding and correlated it with the duration and durability of MS.221The role of IL-15 in these diseases must be evaluated further in appropriate animal models.
Recently, a case of severe eosinophilia with an aberrant T-cell population presenting as cough and dyspnea was reported.223 This patient had elevated serum levels of IL-15 (13.8-36 pg/mL) and IL-2 (1160 pg/mL), and a major T-cell population expressing activation (CD25) and NK cell (CD16, CD56) markers was identified. Although treatment of the patient with steroids failed, the hypereosinophilia and symptoms resolved after hydroxyurea therapy, along with disappearance of the T-cell population and serum IL-15 and IL-2. The authors propose that after challenge with an unknown antigen, a population of T cells was primed by IL-15–secreting APCs. These T cells then produced eosinophilopoietic cytokines, resulting in the pathologic eosinophilia. IL-15 and IL-2 may therefore have a role in the genesis of idiopathic eosinophilia and T-cell expansion, and the shared IL-2/15Rβ may be a useful target in such cases.223
IL-15 and transplant rejection
The immunologic rejection of allografted solid organs by the recipient is a complicated process that includes acute, subacute, and chronic subtypes and is a major obstacle in transplant medicine.224 Cytokines are thought to contribute to allograft rejection by promoting the infiltration and activation of recipient immune cells within the transplanted organ. IL-15 mRNA expression was detected in all 45 biopsies from transplanted kidneys (IL-2 in only 3 of 45) and was significantly increased in rejecting compared with nonrejecting grafts.225 Although IL-15 mRNA expression was detected in the majority of posttransplant livers and was up-regulated compared with nontransplanted liver tissue, no significant correlation was found between IL-15 expression and rejection.226 The failure of an antibody (BT563) that selectively blocks the high-affinity IL-2Rα pathway to prevent acute rejection of heart allografts suggests that other cytokines, such as IL-15, may be responsible for the T-cell proliferation during this process.227 Further studies demonstrated IL-15 mRNA and protein expression within CD68+ macrophages infiltrating transplanted myocardium, with or without anti–IL-2Rα treatment.228 Although the percentage of IL-15+ cells invading the grafts did not directly correlate with rejection grade, these studies suggest that IL-15 may be involved in T-cell activation during heart allograft rejection in the absence of IL-2. Li et al229 observed that mice with targeted disruption of IL-2 and IL-4 (IL-2−/−/IL-4−/− double knockouts) rejected islet allografts, with robust intragraft expression of both IL-15 and IL-7. In this animal model, blockage of the γc receptor significantly prolonged survival, suggesting that signals mediated by IL-15 or IL-7, in the absence of IL-2 and IL-4, participate in acute graft rejection. Collectively, these studies demonstrate a potential role for IL-15 as a therapeutic target during the rejection of transplanted solid organs that requires further investigation.
IL-15 and cancer
HTLV-1–mediated adult T-cell leukemia.
Infection with HTLV-1 can result in adult T-cell leukemia (ATL), a malignancy in which the early phases are associated with autocrine production of IL-2 and expression of IL-2R components. However, later phases lack IL-2 production while IL-2R components remain on the surface of these leukemic cells.230,231 As described earlier, IL-15 was codiscovered as the IL-T fusion protein involving the R region of HTLV-1 fused with the 5′ UTR of the IL-15 gene, and the ATL cell line HuT-102 produced abundant IL-T/IL-15 protein within cell culture supernatants.4 Later it was discovered that HTLV-1 Tax protein transactivates IL-15 gene transcription through a NF-κB site, and cell lines infected with HTLV-1 or transfected with HTLV-1 Tax had significantly higher IL-15 mRNA levels. In addition, IL-15 mRNA expression is elevated in ex vivo leukemic cells from ATL patients compared with normal peripheral blood T cells.61Yamada et al232 demonstrated that ATL cell lines expressed IL-15Rα, bound [125I]IL-15 with high affinity (170 pM), and proliferated for months in response to rhIL-15. However, these cell lines did not produce measurable IL-15 protein in cell culture supernatants, and plasma from patients with ATL (n = 31) did not contain detectable IL-15 protein, with a few exceptions (4.9, 1.7, and 1.7 pg/mL). Thus, the unique property of abundant IL-15 protein secretion by HuT-102 cells does not appear to be a general phenomenon of all ATL cell lines or primary leukemic cells isolated from ATL patients.
On the basis of these studies, we suggest a possible role for IL-15 in the pathogenesis or maintenance of ATL, especially during the relatively common infiltration into IL-15–expressing tissues such as the skin, lungs, liver, and gastrointestinal tract. This hypothesis is consistent with findings that in later IL-2–independent stages of ATL, there is constitutive activation of IL-2/15R signals Jak1/Jak3 and STAT3/STAT5.233 234 Further study of IL-15 in patients with ATL is warranted and will be required to determine definitively whether IL-15 may participate in the initiation, maintenance, or progression of this disease.
Other lymphoid malignancies.
Cutaneous T-cell lymphoma (CTCL) broadly delineates a group of related lymphoproliferative disorders of the skin, including mycosis fungoides (MF) and Sezary syndrome (SS).235 Both IL-2 and IL-7 have been implicated as important growth factors for CTCL cells; however, the etiology of these disorders is actively being investigated.236,237 Indeed, treatment of these patients with an IL-2 fusion toxin, thereby targeting IL-2/15Rβ+cells, appears promising.238 Dobbeling et al239 demonstrated that IL-15 may act as a growth and viability promoting factor for CTCL. IL-15 promoted growth and prolonged survival of the SeAx Sezary cell line as well as malignant T cells isolated from SS patients, and IL-15 mRNA was present within these cells. IL-15 protein was detected by immunohistochemistry in the basal cell layer keratinocytes and in the infiltrating lymphocytes of SS and MF patients' skin biopsy specimens.239 IL-15 was also shown to stimulate AP-1 and JunD DNA binding within CTCL cell lines and may use such pathways to promote CTCL growth.240 Of note, HTLV-1 infection has also been implicated in such CTCLs,241 consistent with the above involvement of HTLV-1/ATL and IL-15 expression. In agreement with IL-7's ability to promote CTCL growth in vitro, transgenic mice engineered to overexpress IL-7 develop cutaneous lymphoproliferation and lymphoma.242 Intriguingly, mice with a global overexpression of a human IL-2 transgene, via an MHC class I promoter, develop a mild cutaneous lymphocytic infiltration. However, this phenotype is not lethal or transforming.243 IL-15 transgenic mice that globally overexpress murine IL-15, including in the skin, develop a lymphocytic infiltrate in the dermis that ultimately leads to total alopecia.68 Considering the well-documented expression of IL-15 message and protein in the skin and the phenotype of IL-15 transgenic mice, it may be appropriate to assess an anti–IL-2/15Rβ treatment in patients with CTCL.
Lymphoproliferative disorder of granular lymphocytes (LDGL) is characterized by an expansion of LGLs consisting of either CD3+ (T cell) or CD3− (NK cell) populations.244 Zambello et al245 showed that both CD3+ and CD3− cells isolated from LDGL patients expressed all 3 of the IL-15R components (IL-2/15Rβ, γc, and IL-15Rα) and proliferated in response to IL-15 in vitro. Although no IL-15 protein was detected in the serum or CD14+ cell culture supernatants of these cells, membrane-bound IL-15 was demonstrated on the surface of CD3+ and CD3− cells from LDGL patients, but not normal controls, by flow cytometry. This is in contrast to the lack of IL-15 mRNA expression by RT-PCR in sorted LGLs from patients, leaving the significance of surface IL-15 detected by flow cytometry unclear. However, the chronic nature of this leukemia and the clear role of IL-15 in the development of CD3+ NK-T and CD3− NK cells suggest that the possible deregulation of IL-15 expression in these patients should be pursued. Indeed, mice engineered with an IL-15 transgene that lacks the normal posttranscriptional checkpoints regulating IL-15 protein translation and secretion have recently been described.68 These mice exhibit an early lymphocytosis composed of NK and CD8+CD44hi T cells. Later, a significant fraction of IL-15 transgenic mice develop a fatal lymphocytic leukemia with a CD3+TCRαβ+CD44+DX5±CD8±phenotype. The clinical course and disease manifestations appear similar to those in patients with LGL leukemia.244,246 247Thus, continued overexpression of IL-15 may predispose to chronic lymphocytosis and eventually to malignant transformation of lymphocytes.
IL-15 has also been shown to induce the proliferation of normal B cells,248 malignant B cells obtained from B-cell chronic lymphocytic leukemia and hairy cell leukemia,249 and the M-07e acute myelogenous leukemia (AML) cell line.250 IL-15R components are expressed on multiple myeloma cells, and IL-15 may play a role in the autocrine propagation of this malignancy.251
Solid tumors.
IL-15 is normally expressed at the mRNA level in several organs, including skeletal muscle, skin, lung, and kidney. Their malignant counterparts, including osteosarcoma, Ewing sarcoma, rhabdomyosarcoma,252 melanoma,253 small cell lung cancer,12 renal cell carcinoma, glioblastoma, neuroblastoma, and mesothelioma, also express the IL-15 transcript.254 Intracellular protein was observed in melanoma cell lines253 and renal cancer cells,254 and low secretion of IL-15 was observed in a subset of osteosarcoma and rhabdomyosarcoma lines (4-8 pg/mL).252 However, a definitive role for IL-15 in the pathogenesis of solid tumors has not been demonstrated.
IL-15 and infectious disease
Human immunodeficiency virus.
IL-15, through its ability to mimic the actions of IL-2, has 2 opposing effects in the HIV-infected patient: a potentially beneficial augmentation of immune function137,255-261 and a potentially detrimental activation of HIV replication.189,258,262,263 Because both of these effects have been observed in several experimental systems, any proposed use of IL-15 in vivo to boost immunity in this immunocompromised population must include careful analysis of HIV replication. Initial studies by Seder et al255 demonstrated that IL-15 enhanced the proliferative response of PBMCs from HIV-infected patients when stimulated with polyclonal mitogens, tetanus toxoid, or HIV-specific antigens. Patki et al256 showed that whereas IL-2 enhanced both spontaneous and antigen-induced lymphocyte proliferation in HIV-infected patients, IL-15 enhanced antigen-induced lymphocyte function only with significantly less HIV-1 replication. IL-15, alone and in combination with IL-12, enhanced deficient in vitro NK cell activity in HIV-1–infected patients,264 and IL-15 + IL-12–stimulated NK cells isolated from HIV-infected patients produced C-C chemokines and inhibited HIV-1 infection in vitro.137Thus, a large body of evidence now suggests that IL-15 significantly improves innate and antigen-specific immune cell function in HIV-1–infected patients in vitro, in some cases better than IL-2. While evidence documents that IL-15 may increase HIV-1 replication in PBMCs and cell lines in vitro, it remains unclear whether the benefits of IL-15 may be achieved at concentrations that do not affect viral loads in vivo. It is encouraging that IL-2 has been used successfully in vivo at low doses to boost immune function in HIV-infected patients, without increases in HIV viral load.95,96 98 Thus, IL-15 is poised as a potential candidate for cytokine therapy in HIV-1 patients that may provide the benefits of IL-2 plus additional immune modulation because of distinct IL-2/15Rαβγ expression patterns.
Other viral and bacterial pathogens.
IL-15 mRNA levels are elevated in PBMCs from patients with another HTLV-1–mediated disease, HTLV-1 myelopathy/tropical spastic paraparesis (HAM/TSP), compared with normal donors.265Antibodies against IL-15 or its receptor blocked spontaneous proliferation of HAM/TSP PBMCs and, when combined with anti–IL-2 antibodies, completely abrogated proliferation. This suggests that dual autocrine loops, including both IL-15/IL-15R and IL-2/IL-2R, may promote lymphocyte proliferation in this disorder.265 In vitro infection of human PBMCs with human herpesvirus (HHV)-6, HHV-7, herpes simplex virus type-1, or Epstein-Barr virus resulted in IL-15–dependent increases in NK cell cytotoxicity and IFN-γ production.128,129 266 Such studies suggest that IL-15 may be involved in early, innate immune defense against viral infections in humans.
Serum levels of IL-15 were significantly elevated in patients with bacteremic (mean, 49.4 pg/mL; range, 12.4-338.8 pg/mL) and nonbacteremic (mean, 31.3 pg/mL; range, 11.6-2743 pg/mL)Burkholderia pseudomallei infection (melioidosis) compared with controls (mean, 12.8 pg/mL; range, less than 8.2 to 122.2 pg/mL), with significantly higher levels in patients with positive blood cultures.267 Several reports have indicated that exogenous administration of rIL-15 before infection, such asSalmonella,134Plasmodium falciparum,268 or C neoformans,135 improves host defense against and clearance of the invading organism. Nishimura et al22generated 2 lines of transgenic mice that express both isoforms of IL-15 under the control of an MHC class I promoter. LSP–IL-15 transgenic mice expressed serum IL-15 protein and had increased memory-phenotype CD8+ T cells in lymph nodes. These mice were resistant to Salmonella infection via a mechanism dependent upon CD8+ T-cell IFN-γ production. In contrast, mice transgenic for the SSP–IL-15 expressed intracellular IL-15 protein, had defective T-cell IFN-γ production, and were susceptible to Salmonella infection. Thus, it appears that in vivo, overexpression of the LSP–IL-15 leads to IL-15 secretion, enhanced CD8+ memory-type cell development, and enhanced host defense against Salmonella, whereas overexpression of SSP–IL-15 remains intracellular and limits T-cell IFN-γ responses.22 rIL-15 has been successful as a vaccine adjuvant in animals through boosting the production of Toxoplasma gondii–specific CD8+ T cells.193Continued explorations of additional animal models of infection, as well as delineation of the mechanism(s) of the action of IL-15 during host defense, are needed to fully understand its role during both innate and specific immune responses.
IL-15 and toxicity
For IL-15 to be considered for use as an immunomodulator in humans, it must be determined whether such exogenous provision will result in toxicity for the patient. Whereas IL-15 administration (3 × 105 U/mouse/d) did not result in mortality when provided alone to mice over the course of at least 10 to 14 days, direct coadministration of IL-15 + IL-12 (1 μg/d) to mice resulted in a lethal cytokine-induced shock cascade, indistinguishable from the lethal effects of IL-2 + IL-12.269 Depletion of NK cells or macrophages before administration of IL-15 and IL-12 provided protection from lethality, suggesting that these innate immune effector cells were the primary effectors during this cytokine-induced shock. Selective elimination of various inflammatory mediators (TNF-α, IFN-γ, MIP-1α, IL-1, IL-1–converting enzyme, Fas, perforin, inducible nitrous oxide synthase (iNOS), or STAT1) using mice with targeted disruptions or neutralizing antibodies revealed that none of these, even in combination, were responsible for the lethal shock-like reaction. Therefore, it is possible that novel proinflammatory mediators are produced in this cascade. Of note, in this model, modest doses of IL-15 become toxic only when combined with IL-12.
The generalized Shwartzman reaction is a lethal cytokine-induced shock response elicited by sequential priming and challenge with bacteria or bacterial components (eg, LPS).270,271 IL-12–induced IFN-γ is critical for sensitization of macrophages during LPS priming.272,273 After initial IFN-γ–dependent priming, a subsequent intravenous LPS challenge 18 to 24 hours later results in cytokine-induced shock and death, largely due to the release of TNF-α and IL-1.272-274 We recently demonstrated that in vivo neutralization of IL-15 before initial LPS priming significantly reduced lethality in this reaction.133 We hypothesized that LPS priming induced IL-12 and IL-15, which costimulated NK cell–derived IFN-γ, consistent with the observation that pretreatment with either anti–IL-2/15Rβ or anti–IL-15 antibodies reduced serum IFN-γ protein after in vivo LPS administration to SCID mice. IL-15 may therefore be a key cofactor in IL-12–induced toxicity in vivo by potentiating IL-12–induced cytokine release.133 These findings should be taken into consideration when designing combination therapies involving IL-15 with other proinflammatory cytokines such as IL-12.
Several chemotherapeutic agents (eg, 5-fluorouracil [5-FU], irinotecan [CT-711]) have documented clinical efficacy against colon cancer, but severe mucosal toxicity remains a significant clinical problem.275 In rat models of colon carcinoma, exogenous administration of IL-15 protected against diarrhea, stomatitis, weight loss, and death induced by 5-FU and irinotecan and increased maximal tolerated doses and overall complete response.276 277 In contrast, exogenous IL-2 potentiated toxicities with no beneficial antitumor effect when used in combination with either chemotherapeutic agent. Although the clinical benefit observed in these 2 animal model systems requires additional study for confirmation of the apparent toxicity-limiting activity, these preclinical models suggest that IL-15 may be useful as a chemoprotective agent in certain therapies.
IL-15 and immunodeficiency
The γc, shared by receptors for IL-2, IL-4, IL-7, IL-9, and IL-15, has been implicated in the etiology of X-linked SCID.26,27 Similarly, the lack of Jak3, a downstream signaling component of γc, results in mice101and humans102 with SCID. The severe immunodeficiency associated with a nonfunctional γc or Jak3 is likely associated with its common usage by multiple cytokines (IL-7, IL-15, IL-2, IL-4) important for lymphocyte development and homeostasis. Although such mutations provide a molecular basis for SCID, a significant portion of SCID patients have normal γc/Jak3 activity. Recently, Gilmour et al104 described a patient with an NK cell–deficient (T↓, NK−, B+) form of SCID, which retained γc/Jak3 yet lacked expression of IL-2/15Rβ. Flow cytometric analysis of the lymphocyte population showed a severe deficit in NK cells, a decrease in T cells, and normal numbers of B cells. However, this patient had defective cellular and humoral immune responses that manifested as recurrent viral and fungal infections during his first year of life. This report demonstrates that lack of IL-2/IL-15 signaling through IL-2/15Rβ can lead to SCID, with the most prominent deficit in the NK cell lineage, thereby highlighting the importance of the human IL-15/IL-15R pathway in vivo.
Potential therapeutic uses of IL-15
Out of the multitude of basic studies on the biology of IL-15 and preclinical models of human disease, it is important to identify those lines of investigation that point toward potential clinical benefit. Two major directions of immediate interest are immune augmentation through exogenous provision of IL-15 and immune down-regulation through elimination of improperly expressed IL-15. Additional clinical applications of IL-15 are emerging from basic and preclinical studies on this cytokine (eg, vaccine adjuvant) but require further development.
Cytokine therapy with IL-15.
Numerous cytokines produced through recombinant DNA technology have now been used successfully to expand or activate immune cells or their progenitors in patients, including erythropoietin, G-CSF, macrophage-CSF, GM-CSF, thrombopoietin, IL-11, IFN-α, and IL-2.278 One direction with strong rationale from basic scientific investigations is the use of exogenous IL-15 to expand lymphocyte subsets in patients with cancer or immunodeficiency. Can IL-15 be used in vivo to increase those cell types that require it for development, expansion, or survival (eg, NK cells, NK-T cells, CD8+ memory T cells) without significant toxicity to patients? Obvious parallels can be made between immunotherapy with IL-2 and IL-15 because of their similar in vitro biologic effects and shared receptor components. Given that IL-2 has been approved by the Food and Drug Administration since 1992 and is effective for increasing lymphocyte subsets at low doses without significant toxicities,94-96 why pursue therapeutic pathways with IL-15? IL-2 and IL-15 use unique high-affinity receptor complexes that have dramatically different expression profiles in humans. Because of this, low concentrations of exogenous IL-15 may have the ability to modulate other immune cell compartments without significant toxicity. This is supported by the fact that IL-15 and IL-2 have very different, nonredundant roles in vivo in mice.9,63,64,99,100,103 In addition, IL-15 and IL-2 appear to have different biodistribution after administration in vivo, with IL-15 more localized in the BM.279 In murine models comparing treatment with IL-15 and IL-2 for efficacy against experimental lung metastases (MCA-205), doses of IL-15 six times higher than IL-2 were required to induce pulmonary vascular leak, ultimately resulting in a higher therapeutic index for IL-15.125 The first step toward evaluating IL-15 for cytokine therapy would be preclinical animal trials examining biologic parameters and toxicity, and, if warranted, phase I and II studies to determine maximal tolerated doses and biologic modulation when IL-15 is administered to humans.
Blockade of improperly expressed IL-15.
Agents that selectively block the action of improperly regulated cytokines have also been successfully used in the clinic, one prime example being soluble TNF receptor for inflammatory conditions.280,281 Several studies in murine models have identified agents that can block the action of murine IL-15 in vivo, including a soluble IL-15Rα,212 an antagonist IL-15mutant/Fcγ2a fusion protein,282 and a polyclonal neutralizing antiserum.133 Strong evidence (described earlier) now exists for the role of IL-15 in RA, and the blockade of IL-15 is of potential clinical benefit.283 Thus, with recent evidence in animal models demonstrating that the blockade of IL-15/IL-15R in vivo ameliorates collagen-induced arthritis212 and antigen-specific delayed-type hypersensitivity responses,282 the performance of additional preclinical studies and early clinical trials appears warranted. Similarly, certain lymphoid malignancies may be associated with aberrant IL-15 or IL-15R expression (discussed earlier), and therapeutic strategies to block the IL-15/IL-15R axis may also be useful in these diseases. Therefore, the development of effective human IL-15–blocking agents (eg, high-affinity soluble IL-15Rα, humanized anti–IL-15 MoAb) with in vivo blocking activity could facilitate rapid translation of such approaches to the clinic.
Conclusions
A remarkable amount of progress has been made in our understanding of IL-15 biology, its role in the normal host immune response, and its potential for participation in the pathogenesis of disease since its discovery in 1994. Because IL-15 has pleiotropic activity that ultimately results in immunoregulatory cross-talk between natural and specific immune cells, it may now be considered a cytokine that bridges the innate and adaptive immune systems (Figure5). Unraveling the biology of IL-15 has revealed some interesting surprises, such as the complex multifaceted regulation of its gene expression and a potential nuclear function. The large body of in vitro and in vivo evidence documenting the importance of IL-15 during NK cell ontogeny may point toward some of the first therapeutic applications for this cytokine to augment immune function in patients with cancer or immunodeficiency. In contrast, the discovery of IL-15's role in the pathogenesis of RA and shock may yield equally fruitful therapies aimed at blocking improper immune activation. For IL-15–based therapies to be rapidly translated into the clinical arena, additional preclinical animal studies and phase I/II clinical trials must be performed to solidify the rationale for broader application in human disease.
IL-15 is a pleiotropic cytokine that functions in NK cell development, lymphocyte homeostasis, and peripheral immune functions.
Multiple cell types elaborate IL-15, including activated (eg, virus- or bacteria-infected) monocytes/macrophages, dendritic cells, and epithelium, as well as constitutive production by BM stromal cells. IL-15 has a critical role in the development of the NK lineage, as well as in its survival, expansion, and function. Other innate lymphocytes (NK-T, CD8αα i-IEL, TCRγδ DETCs) and memory-phenotype CD8+ T cells depend upon IL-15 for survival or expansion. IL-15 also plays multiple roles in peripheral innate and adaptive immune cell function.
IL-15 is a pleiotropic cytokine that functions in NK cell development, lymphocyte homeostasis, and peripheral immune functions.
Multiple cell types elaborate IL-15, including activated (eg, virus- or bacteria-infected) monocytes/macrophages, dendritic cells, and epithelium, as well as constitutive production by BM stromal cells. IL-15 has a critical role in the development of the NK lineage, as well as in its survival, expansion, and function. Other innate lymphocytes (NK-T, CD8αα i-IEL, TCRγδ DETCs) and memory-phenotype CD8+ T cells depend upon IL-15 for survival or expansion. IL-15 also plays multiple roles in peripheral innate and adaptive immune cell function.
Acknowledgments
We thank Anand Ponnappan (The Ohio State University) for assistance in the preparation of the manuscript and Christopher VanDeusen (Stanford University) for his assistance in generating the theoretical model of IL-15 structure. We also thank Drs Christine Biron and Jacques Peschon, as well as Megan Cooper and Jeffrey VanDeusen, for their critical review of the manuscript. We apologize to those investigators not cited in this review as a result of space limitations.
Supported by National Institutes of Health grants CA68458, CA65670, and P30CA16058. T.A.F. is the recipient of Medical Scientist Program (MSP) and Bennett fellowships from The Ohio State University College of Medicine and Public Health.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Michael A. Caligiuri, The Ohio State University, 458A Starling Loving Hall, 320 W 10th Ave, Columbus, OH 43210; e-mail:caligiuri-1@medctr.osu.edu.

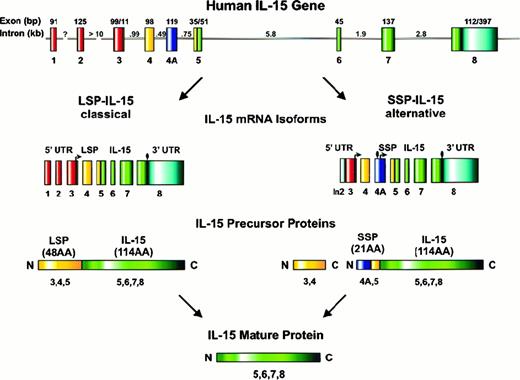
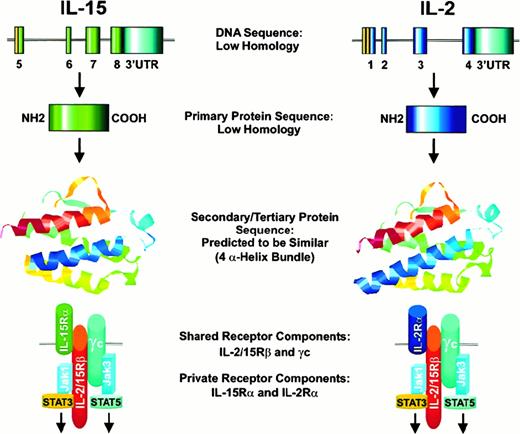
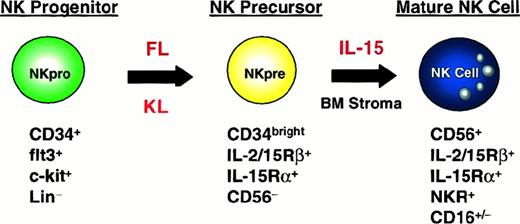
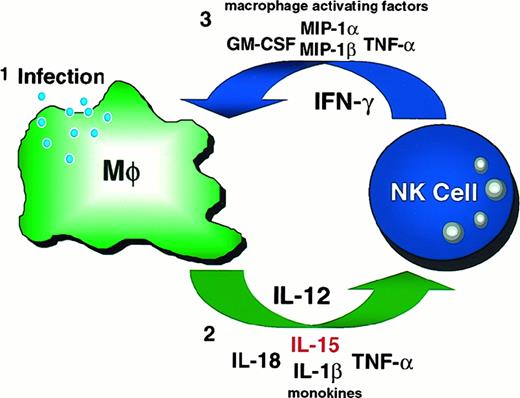
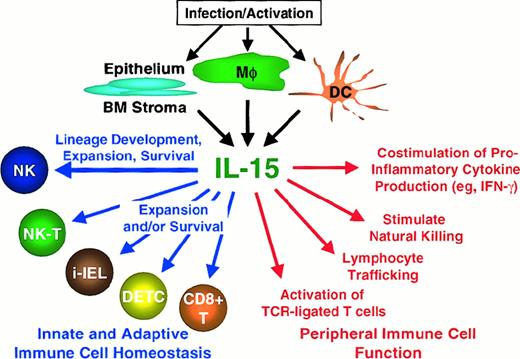
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal