The influence of platelets on the cellular metabolism of atherogenic lipoproteins has not been characterized in detail. Therefore, we investigated the effect of platelet factor 4 (PF4), a cationic protein released in high concentration by activated platelets, on the uptake and degradation of low-density lipoprotein (LDL) via the LDL receptor (LDL-R). LDL-R–dependent binding, internalization, and degradation of LDL by cultured cells were inhibited 50%, 80%, and 80%, respectively, on addition of PF4. PF4 bound specifically to the ligand-binding domain of recombinant soluble LDL-R (half-maximal binding 0.5 μg/mL PF4) and partially (approximately 50%) inhibited the binding of LDL. Inhibition of internalization and degradation by PF4 required the presence of cell-associated proteoglycans, primarily those rich in chondroitin sulfate. PF4 variants with impaired heparin binding lacked the capacity to inhibit LDL. PF4, soluble LDL-R, and LDL formed ternary complexes with cell-surface proteoglycans. PF4 induced the retention of LDL/LDL-R complexes on the surface of human fibroblasts in multimolecular clusters unassociated with coated pits, as assessed by immuno-electron microscopy. These studies demonstrate that PF4 inhibits the catabolism of LDL in vitro in part by competing for binding to LDL-R, by promoting interactions with cell-associated chondroitin sulfate proteoglycans, and by disrupting the normal endocytic trafficking of LDL/LDL-R complexes. Retention of LDL on cell surfaces may facilitate proatherogenic modifications and support an expanded role for platelets in the pathogenesis of atherosclerosis.
Introduction
Platelet adhesion and aggregation contribute to thrombotic occlusion of atherosclerotic vessels.1,2Whether persistent platelet activation occurring over decades also contributes to the progression of atherosclerosis itself is less clear. The paucity of platelets seen in morphologic analyses of human atherosclerotic lesions has de-emphasized their role in lesion development. However, platelet antigens have been detected in human atherosclerotic lesions,3 and platelets have been found adherent to activated endothelium in affected human vessels.4-6 Moreover, recent studies indicate that platelet activation begins during early stages of atherosclerotic development in mice with targeted deletions in apolipoprotein E or the low-density lipoprotein receptor (LDL-R)7 and that pharmacologic inhibition of platelet cyclooxygenase-1 inhibits lesion progression.8 Activated platelets release potent vasoconstrictors such as thromboxane A2, smooth muscle cell mitogens,9,10 and other moieties that augment the recruitment of monocytes to the vessel wall by inducing endothelial cells to synthesize monocyte chemotactic protein-1 and to express intracellular adhesion molecule 111 in vitro. However, the mechanism by which platelets might promote the development of atherosclerosis in vivo has received little study.
One candidate linking platelet activation with atherosclerosis is platelet factor 4 (PF4), the most abundant protein secreted by activated platelets. PF4 is stored in platelet α-granules as a tetramer bound to serglycin-4, a proteoglycan rich in chondroitin sulfate (CS).12 The concentration of PF4 in the α-granules is estimated to be 1500 μg/mL,12 and serum concentrations exceed 8 μg/mL when platelets are activated.13 Even higher concentrations of PF4 are likely to occur at the interface between the exocytosed membranes of the α-granules and the anionic proteoglycans of the vasculature, which avidly bind the protein.14 15
The crystal structure of PF4 demonstrates that the core of the tetramer is composed of 3 antiparallel β-sheets. The carboxy-terminal amphipathic-helix of each constituent monomer also contains 4 lysine residues that face the outer surface of the molecule that contribute to a ring of cationic residues that encircle the tetramer,16comprising the binding site for heparin and related vascular proteoglycans. This juxtaposition of hydrophobic and cationic domains may allow PF4 to serve as a bridge between lipoproteins and the vasculature.
Increasing evidence suggests that factors that promote the retention of lipoprotein in the vessel wall contribute to the pathogenesis of atherosclerosis (reviewed in Williams and Tabas17). In the case of LDL, binding of apolipoprotein B (ApoB) to the LDL-R18-20 and proteoglycans17,21 initiates plasma clearance and lipoprotein degradation. Analysis of naturally occurring mutations in patients with hypercholesterolemia, confirmed by mutagenesis studies, indicates that ApoB100, like apolipoprotein E and lipoprotein lipase, has a hydrophobic surface that interacts within the lipoprotein and a cationic face that binds to negatively charged domains on LDL-R and proteoglycans.21,22 Likewise, we have observed that α-defensins, a family of closely related neutrophil proteins that share this property of alternating hydrophobic and cationic domains, inhibit the interaction of LDL with LDL-R and promote its binding to proteoglycans and other components of the vascular matrix.23,24 Redirection of LDL from the efficient LDL-R–mediated pathway of internalization/degradation promotes lipoprotein retention in the vasculature and may predispose to proatherogenic modifications.23
On the basis of these considerations, we examined the effect of PF4 on the formation and trafficking of the LDL/LDL-R complex. PF4 has been reported to inhibit binding of LDL to cells that express LDL-R, although involvement of this receptor per se and mechanism by which PF4 exerts this effect have not been elucidated.20 Our findings indicate that PF4 partially inhibits LDL binding to LDL-R and almost totally inhibits receptor-dependent internalization and degradation of the lipoprotein by forming multimolecular complexes with cell-surface proteoglycans. The result is redirection of LDL from efficient endocytosis and intracellular catabolism toward retention on the cell surface in aggregates containing LDL-R and proteoglycans.
Materials and methods
Materials
Heparinase I (EC 4.2.2.7) and chondroitin ABC lyase (EC 4.2.2.4) were from Sigma (St Louis, MO); their enzymatic activity, specificity, and absence of protease activity were verified as described.25-27 Recombinant PF4 and neutrophil-activating peptide 2 (NAP-2) were prepared and purified as described.28-30 Recombinant PF4 QE2 mutant complementary DNA (cDNA) was constructed in pGEX-6P-1 as a fusion protein with glutathione-S-transferase (GST) N-terminal sequence followed by the PreScission protease (Amersham-Pharmacia-Biotech, Piscataway, NJ), the PF4 protein using overlap polymerase chain reaction mutagenesis and was transfected into BL21 bacteria, and expression was induced as described.30 Purification and removal of the GST N-terminal sequence was performed by using the GST Gene Fusion System (Amersham-Pharmacia-Biotech) following the manufacturer's instructions. The final products migrated as single bands on sodium dodecyl sulfate–polyacrylamide gel electrophoresis Coomassie-blue–stained gels. Monoclonal C7 α–LDL-R antibody was purified from conditioned medium of the hybridoma CRL-1691 (American Type Culture Collection, Manassas, VA) by using protein A–Sepharose (Pharmacia Biotech, Uppsala, Sweden). Rabbit α-human ApoB100 antibody was obtained from Calbiochem (La Jolla, CA). LDL was prepared from fresh human plasma by ultracentrifugation (1.019 < d < 1.63 g/mL)24 and radiolabeled by using125I-monochloride.31 The specific activity of125LDL was 200 to 400 cpm/ng protein (45-90 Ci/mmol [1.7-3.3 × 1012 Bq/mmol]). Oxidation of LDL32 was below the limits of detection (< 0.5 TBARS/mg protein).
Cell culture
All cultures were maintained at 37°C in a humidified atmosphere containing 5% CO2. Chinese hamster ovary (CHO) cells lacking xylosyl-transferase (XT−), incapable of initiating the synthesis of heparan sulfate (HS) or CS chains, and CHO cells lacking glucuronic acid/N-acetylgalactosamine transferase (HS−), selectively deficient in HS but overexpressing CS, were the kind gifts of J. Esko (University of California, San Diego).33 CHO cells lacking LDL-R (A7) were the kind gift of M. Krieger (MIT, Cambridge, MA).34 CHO cells were grown in Hams F12 media supplemented with fetal calf serum (FCS; 10%), glutamine (2 mM), penicillin (100 U/mL), and streptomycin (100 μg/mL). Normal skin fibroblasts (CRL-1474) obtained from American Type Culture Collection and LDL-R–deficient (FH) fibroblasts, kindly provided by E. Leitersdorf (Hadassah Medical Center, Jerusalem, Israel), were grown in Dulbecco modified Eagle medium (DMEM) supplemented with FCS (10%), nonessential amino acids (0.1 mM), glutamine (2 mM), penicillin (100 U/mL), and streptomycin (100 μg/mL). A431 cells were grown in DMEM supplemented with FCS (10%), glutamine (2 mM), penicillin (100 U/mL), and streptomycin (100 μg/mL).
RNA synthesis and transfection
Synthetic messenger RNA (mRNA) transcripts were obtained by in vitro synthesis.35,36 The plasmid pT7TD–LDL-R was constructed by subcloning human LDL-R cDNA into pT7TS plasmid (kindly provided by P. Krieg, University of Texas, Austin) at the EcoRV site between the globin gene 5′- and 3′-untranslated sites. The plasmid was linearized with XbaI and Eco1CRI. Linearized pT7TD–LDL-R (1 μg) was used as the template for mRNA synthesis by using the MessageMachine system (Ambion, Austin, TX) with T7-polymerase. Extension of the poly-A tail was performed by using Yeast Poly(A) Polymerase (USB, Cleveland, OH) according to the manufacturer's instructions. LDL-R–deficient CHO cells were transfected with RNA (LDL-R or control) in 48-well plates by using Lipofectin (Life Technologies, Rockville, MD).35 36
Binding, internalization, and degradation of 125I-LDL
The method of Goldstein et al31 was followed. Briefly, LDL-R–deficient CHO cells transfected with LDL-R or control mRNA were incubated in binding buffer (minimal essential medium supplemented with Earle salts, 20 mM HEPES, 1% bovine serum albumin [BSA], pH = 7.4) containing the relevant ligand(s) for 4 hours at 37°C in 5% CO2. Cells were then incubated at 4°C for 30 minutes prior to measuring radioactivity in each compartment. Internalized counts were defined as the sum of the NaOH soluble counts and degraded LDL.37 Binding refers to LDL that remains on the cell surface at the end of the incubation period. In some experiments, cells were preincubated with low doses of PF4 (2 μg/mL) for 24 hours prior to addition of 125I-LDL. In other experiments, the capacity of heparin (10 μg/mL), LDL (200 nM), and EDTA (10 mM) to displace cell-associated 125I-LDL was measured by incubation with these agents for 1 hour at 37°C prior to chilling the cells. The migration of 125I-LDL and125I-LDL eluted from the cell surface by EDTA was compared by native gel electrophoresis by using the Titan Gel Lipoprotein Kit (Helena Laboratories, Beaumont, TX) and viewed by autoradiography.
Binding, internalization, and degradation of125I–epidermal growth factor
Experiments were performed as described.38125I–epidermal growth factor (EGF; 7 nM) was incubated with A431 cells for 4 hours at 37°C alone or in the presence of PF4 (20 μg/mL) or unlabeled EGF (800 nM). Binding buffer was DMEM, BSA (0.1%), and HEPES (20 mM, pH 7.4). Bound, internalized, and degraded counts were determined as for LDL except that surface-bound EGF was eluted with acetate buffer (200 mM NaAc,500 mM NaCl, pH 5).
Cloning, expression, and purification of LDL-R 1-354
The plasmid pMT–LDL-R was constructed by subcloning the human LDL-R cDNA fragment encoding the first 354 residues of the mature receptor into pMT/BIP/V5-HIS (Invitrogen, Carlsbad, CA). The plasmid was transfected into Drosophila Schneider-2 cells, selected with hygromycin, and induced with CuSO4 according to manufacturer's instructions (Drosophila Expression System; Invitrogen). LDL-R 1-354 (sLDL-R) was purified from media by using the Xpress System ProBond-Ni resin (Invitrogen) followed by reverse-phase high-performance liquid chromatography over a C8-column (Vydac, Hesperia, CA); high-performance liquid chromatography mobile phase was 0.1% TFA and CH3CN (from 20% to 70% over 35 minutes) at 4 mL/minute.
Binding of PF4 to sLDL-R
sLDL-R (10 μg/mL) was coated on 96-well plates (Immulon 2; Dynatech Labs, Chantilly, VA) overnight at 4°C and blocked with 1% BSA for 1 hour at room temperature. After incubation with125I-PF4 in TBSC (50 mM Tris pH = 8, 90 mM NaCl, 2 mM CaCl2) containing 1% BSA (50 μL/well) for 1 hour at room temperature, wells were washed 3 times with ice-cold TBSC. Bound125I-PF4 was removed by adding 2 N NaOH for 30 minutes at room temperature. Nonspecific binding was measured in the presence of 100 μg/mL unlabeled PF4. Specific binding was determined by subtracting nonspecific binding from total binding. In addition, an enzyme-linked immunosorbent assay (ELISA) format was used to measure PF4 binding to sLDL-R. PF4 (0.25-8 μg/mL) was added to immobilized sLDL-R for 1 hour at room temperature. Bound PF4 was detected by using a murine monoclonal antihuman PF4 antibody (RTO)39 as the primary antibody and a peroxidase-conjugated donkey antimouse secondary antibody (Jackson ImmunoResearch Laboratories, West Grove, PA). Absorbance at 450 nm was monitored after addition of o-phenylenediamine. Nonspecific binding, determined by measuring PF4 binding to BSA-coated wells, was less than 20% of total. Binding of preimmune isotype control (MOPC141; Sigma) was comparable to nonspecific binding.
Binding of 125I-sLDL-R to cells
Cells were incubated in LDL binding buffer for 1 hour at 37°C in 5% CO2 to remove residual LDL. Cells were then incubated in binding buffer containing ligands for 1 hour at 37°C in 5% CO2 and then at 4°C for 15 minutes. Media were removed, and cells were washed 3 times with ice-cold binding buffer. Cells were incubated for 30 minutes at room temperature with 2 N NaOH to solubilize bound ligand.
Gold-labeled ligand electron microscopy
Colloidal gold40 and LDL-gold (Au-LDL) complex were prepared as described.41 Fibroblasts (SK25) grown on membrane inserts (Costar, Corning, NY) were incubated with 5 nM Au-LDL ± 40 μg/mL PF4 at 37°C for 5 to 240 minutes, as indicated. Cells were fixed immediately in 0.1 M sodium cacodylate (NaCaC) buffer containing 2% glutaraldehyde, postfixed in 1% Osmium tertraoxide, stained enbloc in 2% aqueous uranyl acetate, and dehydrated in graded alcohol followed by propylene oxide. After infiltrating with PO/Epon 1:1, they were embedded in Epon and cured at 70°C for 48 hours. Sections (70-nM thick) were placed on Formvar-coated slotted or thin bar 200-mesh copper grids. Sections were saturated with alcoholic uranyl acetate, counterstained in bismuth subnitrite, and observed by using a JEOL JEM 1010 microscope (Tokyo, Japan). Images were captured by using AMT HR-12 system with a Hamamatsu CCD camera (Danvers, MA). Particles in 13 to 28 representative fields (×30 000) were counted in each condition to estimate the percentage of internalization.
Immuno-electron microscopy
Immuno-electron microscopy studies were performed as described42 by using fibroblasts grown in 35-mm tissue culture dishes (Costar). Cells were incubated either with Au-labeled or unlabeled LDL in the absence or presence of 40 μg/mL PF4 for up to 120 minutes. After fixation, cells were gently scraped off the plate, pelleted, partially dehydrated in graded alcohol, and embedded in LRWhite. Sections, 90-nm thick, were picked up on nickel grids. Nonspecific staining was blocked, and LDL-R was stained with monoclonal C7 α–LDL-R followed by 5 or 10 nm Au–α-mouse immunoglobulin G (IgG). Unlabeled LDL was detected by using polyclonal α–ApoB100 and 18 nm Au–α-rabbit IgG. Identical results were obtained when the size of the Au labels was reversed to ensure that Au particle size did not create artifacts. To avoid steric hindrance by the first antibody, the secondary antibody was added to the opposite grid face. Sections were stained with aqueous uranyl acetate for contrast and imaged.42
Results
We studied the effect of PF4 on the binding, internalization, and degradation of LDL through the LDL-R pathway. Initial studies were performed in CHO cells transiently transfected with LDL-R mRNA to enhance receptor copy number in a controlled manner and to permit the role of proteoglycans in the process to be examined. All experiments were performed with 5 nM 125I-LDL, which approximates the Kd for LDL-R, to selectively examine LDL-R–dependent interactions.
PF4 inhibits LDL-R–mediated degradation of LDL
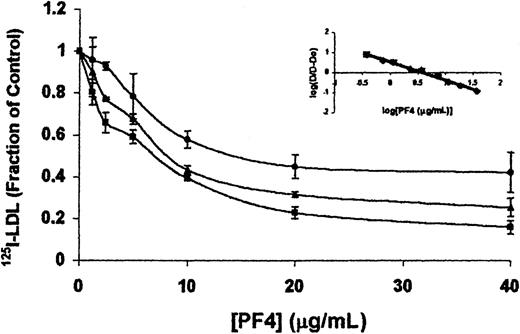
PF4 inhibited the internalization and degradation of125I-LDL (5 nM) by CHO cells expressing LDR-R in a dose-dependent manner (Figure 1). Half-maximal inhibition of degradation was observed at a PF4 concentration of 3.7 μg/mL (from indirect Hill analysis; Figure 1inset), and inhibition was almost total at PF4 concentrations above 20 μg/mL. Similar results were obtained by using LDL-R up-regulated fibroblasts (not shown). Inhibition of LDL degradation in the presence of 40 μg/mL PF4 was comparable to that seen with 500 nM LDL (100-fold excess), 10 mM EDTA, by mock-transfected LDL-R–deficient CHO cells, or by human FH fibroblasts lacking LDL-R (not shown). Inhibition of LDL-R–mediated degradation (approximately 20%) was also evident in cells repetitively exposed to lower doses of PF4 (2 μg/mL) over 24 hours. Taken together, these results demonstrate that PF4 inhibits the degradation of LDL through the LDL-R, consistent with previous observations using human fibroblasts.20 However, LDL internalization and degradation were unaffected by NAP-2, a cationic platelet α-granule–specific chemokine with 60% amino acid homology to PF4 that also binds to heparin and related molecules.30Thus, inhibition of LDL binding and degradation by PF4 cannot be ascribed solely to its cationic charge.
PF4 inhibits the binding, endocytosis, and degradation of LDL.
125I-LDL (5 nM) was incubated with LDL-R–transfected CHO cells in the presence of increasing concentrations of PF4 for 4 hours at 37°C. Cells were chilled to 4°C for 30 minutes, after which surface bound (●), internalized (▴), and degraded (■) LDL were measured as described in “Materials and methods.” Data are the mean ± SEM of 4 independent experiments, each performed in triplicate. (Inset) Indirect Hill plot of degradation data. D0 represents LDL degradation in the absence of PF4. D represents LDL degradation in the presence of PF4 at a given concentration.
PF4 inhibits the binding, endocytosis, and degradation of LDL.
125I-LDL (5 nM) was incubated with LDL-R–transfected CHO cells in the presence of increasing concentrations of PF4 for 4 hours at 37°C. Cells were chilled to 4°C for 30 minutes, after which surface bound (●), internalized (▴), and degraded (■) LDL were measured as described in “Materials and methods.” Data are the mean ± SEM of 4 independent experiments, each performed in triplicate. (Inset) Indirect Hill plot of degradation data. D0 represents LDL degradation in the absence of PF4. D represents LDL degradation in the presence of PF4 at a given concentration.
PF4 partially inhibits the binding of LDL to LDL-R
We then asked whether PF4 blocked LDL degradation solely by inhibiting its binding to LDL-R. PF4 inhibited binding of125I-LDL to CHO cells expressing LDL-R, but to a substantially lesser extent than it blocked degradation at each concentration studied (Figure 1). At the highest concentration tested (40 μg/mL) binding of LDL was reduced by approximately 50%, whereas degradation was inhibited nearly completely. These results indicate that PF4 inhibits LDL degradation through mechanisms in addition to its effect on receptor binding.
We also measured the binding and degradation of 125I-PF4 by untransfected and LDL-R–transfected LDL-R–deficient CHO cells. As expected, no difference in binding to the 2 cell types was seen at PF4 concentrations that almost completely inhibited LDL degradation (20 μg/mL). The absence of a discernible difference in binding undoubtedly reflects the large reservoir of proteoglycans relative to LDL-R. Of greater interest, we found no measurable internalization or degradation of 125I-PF4 within the first 4 hours of incubation at 37°C, a time by which internalization and degradation of LDL was essentially complete in the absence of PF4. These data suggest that the effect of PF4 on LDL degradation is likely to occur on the cell surface.
Inhibition of LDL degradation by PF4 requires proteoglycans
With the knowledge that PF415,43 and LDL17,21,44 45 each bind to proteoglycans, we studied the involvement of HS and/or CS in the inhibition of degradation. We used 3 complementary approaches: (1) enzymatic cleavage of proteoglycans from wild-type (WT) cells, (2) CHO cell variants with genetically altered proteoglycan expression, and (3) analysis of PF4 variants with selective deficiency in binding to heparin and related molecules.
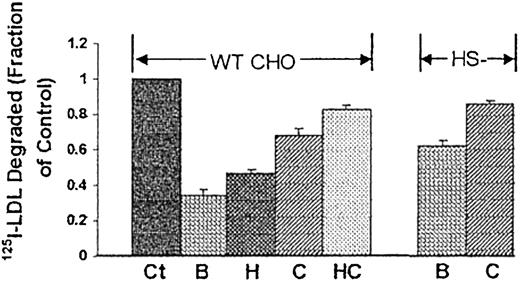
Digestion of either HS or CS from WT LDL-R–expressing CHO cells blunted the inhibitory effect of PF4 (Figure2). Simultaneous digestion of cell-associated HS and CS almost completely abrogated inhibition. Similarly, degradation of LDL by LDL-R–expressing CHO cells that lack HS (but which do express CS) was less affected by PF4, comparable to WT cells from which HS had been removed. Treatment of these cells with chondroitinase almost entirely abolished the effect of PF4, similar to the effect seen after digestion of both classes of glycosaminoglycans from WT cells. These data demonstrate that both CS and HS are required for maximal inhibition of LDL degradation by PF4, but that CSs play the dominant role. Furthermore, because CSs are internalized poorly, if at all,26 their involvement is consistent with our finding that PF4 acts on the cell surface.
Participation of proteoglycans in PF4-mediated inhibition of LDL degradation.
Degradation of 125I-LDL (5 nM) in the presence or absence of PF4 (20 μg/mL) by WT CHO cells and CHO cells that do not express heparan sulfate (HS−). LDL-R–transfected cells were pretreated with buffer (B), heparanase (H), chondroitinase ABC (C), or both heparanase and chondroitinase (HC) for 2 hours at 37°C prior to addition of 125I-LDL. Data are expressed relative to “control” (Ct), which represents degradation of LDL in the absence of PF4. Data are the mean ± SEM of 3 independent experiments, each performed in triplicate.
Participation of proteoglycans in PF4-mediated inhibition of LDL degradation.
Degradation of 125I-LDL (5 nM) in the presence or absence of PF4 (20 μg/mL) by WT CHO cells and CHO cells that do not express heparan sulfate (HS−). LDL-R–transfected cells were pretreated with buffer (B), heparanase (H), chondroitinase ABC (C), or both heparanase and chondroitinase (HC) for 2 hours at 37°C prior to addition of 125I-LDL. Data are expressed relative to “control” (Ct), which represents degradation of LDL in the absence of PF4. Data are the mean ± SEM of 3 independent experiments, each performed in triplicate.
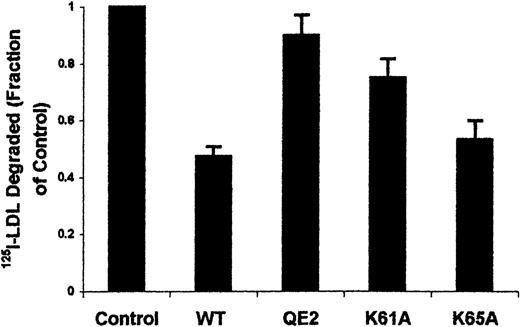
The effect of mutations in the carboxy-terminal α-helical region of PF4 was then examined. This region contains 2 lysine clusters (61,62 and 65,66) important for PF4-glycosaminoglycan interactions.16,46,47 As shown in Figure3, replacement of both of these lysine pairs with the QE combination (QE2)48 almost totally blocks the inhibitory effect of PF4. To dissect the contribution of each cluster, the first lysine of each pair was individually replaced with alanine (K61A and K65A). Whereas loss of K61 significantly reduced the inhibitory capacity of PF4, loss of K65 has little or no effect, although each has similar heparin affinity for heparin as WT PF4.30 The data support the concept that PF4-glycosaminoglycan interactions are necessary but not sufficient to inhibit LDL degradation.
C-terminal lysine residues are important for PF4 inhibition of LDL degradation.
Degradation of 125I-LDL (5 nM) in the absence (control) or presence of WT or mutant PF4 (10 μg/mL) by LDL-R–transfected CHO cells. Data are shown relative to control and are the mean ± SEM of 3 independent experiments, each performed in triplicate. QE2, K61, and K65 are mutant PF4 proteins described in the text.
C-terminal lysine residues are important for PF4 inhibition of LDL degradation.
Degradation of 125I-LDL (5 nM) in the absence (control) or presence of WT or mutant PF4 (10 μg/mL) by LDL-R–transfected CHO cells. Data are shown relative to control and are the mean ± SEM of 3 independent experiments, each performed in triplicate. QE2, K61, and K65 are mutant PF4 proteins described in the text.
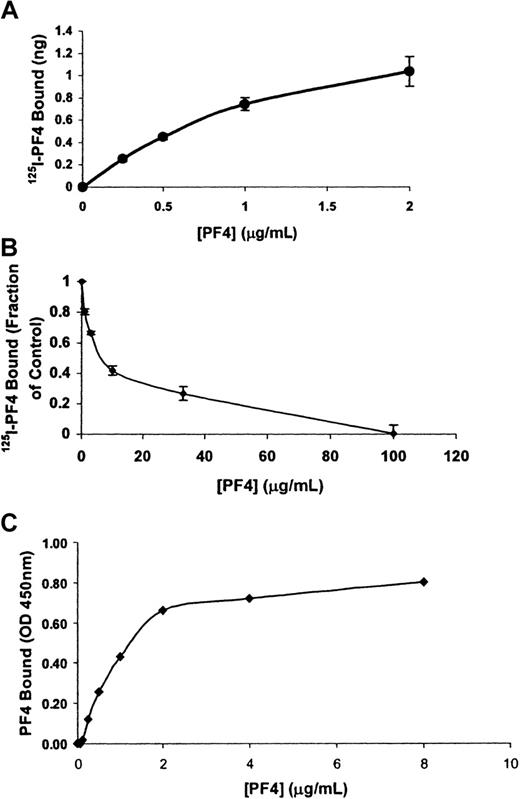
PF4 binds to soluble LDL-R
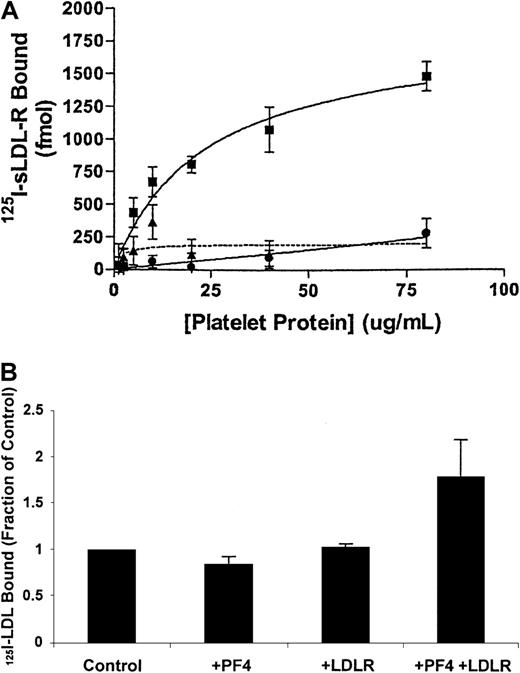
We next examined the involvement of LDL-R in greater detail. Data presented thus far suggest that the effect of PF4 on LDL degradation likely occurs on the cell surface. Therefore, we asked whether PF4 binds to external domains of LDL-R and thereby inhibits LDL binding. A soluble fragment of human LDL-R composed of the 7-ligand binding domains (residues 1-354; sLDL-R) was immobilized, and binding of125I-LDL and 125I-PF4 was measured at room temperature. Binding of 125I-LDL to sLDL-R was specific, concentration-dependent, Ca++-dependent, and saturable (Kd approximately 20 nM), consistent with previous characterization of this receptor fragment.49 PF4 (up to 40 μg/mL) partially (approximately 50%) inhibited the binding of 125I-LDL, similar to its effects on the cell surface (not shown).125I-PF4 also bound to sLDL-R in a specific, dose-dependent manner. Binding was half-maximal at a concentration of approximately 0.5 μg/mL and approached saturation at 2 μg/mL (Figure4A); PF4 approached but did not attain saturation because of increased nonspecific binding at concentrations above 2 μg/mL. Saturation was evident when binding of PF4 to sLDL-R was measured by ELISA. We, therefore, measured PF4 binding by ELISA by using a monoclonal anti-PF4 antibody (Figure 4C). These data demonstrate saturable binding with half-maximal binding at approximately 1 μg/mL and are consistent with the radioligand binding data (Figure 4A).
PF4 binds to the LDL receptor.
125I-PF4 was incubated for 1 hour at room temperature with soluble human LDL-R (amino acids 1-354). (A) Isotherm of specific binding of 125I-PF4 to sLDL-R. (B) Inhibition of125I-PF4 (0.5 μg/mL) binding to sLDL-R by unlabeled PF4. Data are the mean ± SEM of 3 independent experiments, each performed in triplicate. (C) Isotherm of specific binding of PF4 to sLDL-R detected by the monoclonal antihuman PF4 antibody (RTO). Data are representative of 3 independent experiments, each performed in triplicate.
PF4 binds to the LDL receptor.
125I-PF4 was incubated for 1 hour at room temperature with soluble human LDL-R (amino acids 1-354). (A) Isotherm of specific binding of 125I-PF4 to sLDL-R. (B) Inhibition of125I-PF4 (0.5 μg/mL) binding to sLDL-R by unlabeled PF4. Data are the mean ± SEM of 3 independent experiments, each performed in triplicate. (C) Isotherm of specific binding of PF4 to sLDL-R detected by the monoclonal antihuman PF4 antibody (RTO). Data are representative of 3 independent experiments, each performed in triplicate.
Binding of 125I-PF4 (0.5 μg/mL) to sLDL-R was inhibited by unlabeled PF4 (IC50 = 6.9 ± 0.8 μg/mL; Figure 4B) and by 10 mM EDTA. However, binding of 125I-PF4 to sLDL-R was not inhibited by 500 nM LDL, although PF4 partially inhibited125I-LDL binding (vide supra). These data suggest that PF4 binds directly to the ligand-binding domains of LDL-R but that LDL and PF4 do not compete for the same site. Moreover, the maximal effect of PF4 on LDL degradation occurred at ligand concentrations that exceed those that maximally inhibit binding to LDL-R.
LDL and LDL-R are clustered on the cell surface in the presence of PF4
These data show that PF4 inhibits LDL-R–mediated degradation in part by inhibiting binding of the lipoprotein. However, inhibition of LDL binding is incomplete, whereas PF4 inhibits LDL degradation almost completely. We, therefore, turned our attention to understanding the mechanism by which PF4 inhibited the degradation of the residual LDL that bound to the cell.
On the basis of the requirement for proteoglycans and the discordance between the effect of PF4 on LDL binding and degradation, we hypothesized that the PF4-protetoglycan complexes may alter the membrane trafficking of LDL and/or LDL-R. To address this possibility, we examined the effect of PF4 on the subcellular distribution of LDL in normal human fibroblasts, which express coated pits that are readily visualized through which LDL/LDL-R complexes are internalized. After internalization, LDL and LDL-R are segregated; LDL-R is recycled back to the cell surface, whereas LDL is targeted to lysosomes for degradation.50 51
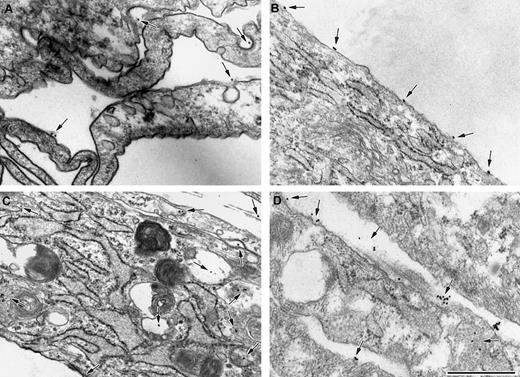
Fibroblasts were incubated with Au-LDL in the presence or absence of 40 μg/mL PF4 and then examined by transmission electron microscopy (Figure 5). In the absence of PF4, LDL was localized primarily (mean, 71%) on the cell surface after a 30-minute incubation at 37°C, with many particles found in clatharin-coated pits (Figure 5A). By 120 minutes, the LDL was almost entirely internalized (mean, 91%) in normal-appearing endosomal/lysosomal structures (Figure 5C). Au-LDL did not bind to FH fibroblasts, which lack LDL-R (not shown). In the presence of PF4, LDL was also found on the surface at 30 minutes (mean, 93%; Figure 5B) but never in coated pits. Small clusters of LDL on the cell surface were noted at this time. However, more dramatic differences in the subcellular localization were evident at 120 minutes. In the presence of PF4, 92% of the remaining LDL was retained on the cell surface in clusters containing 10 or more particles (Figure 5D). Such clusters of LDL were never seen in the absence of PF4.
PF4 promotes aggregation of LDL on the cell surface, outside coated pits.
Electron micrographs of fibroblasts incubated with 5 nM Au-LDL alone (A,C) or 5 nM Au-LDL in the presence of 20 μg/mL PF4 (B,D) for 30 (A,B) or 120 (C,D) minutes at 37°C. The size of the Au particles used was 18 nm. At 30 minutes (A,B) most Au-LDL (arrow) is on the cell surface. In the absence of PF4, LDL is seen in coated pits, whereas, when PF4 is present, LDL was exclusively located outside coated pits. At 120 minutes LDL is primarily located intracellularly in the absence of PF4 (C). LDL is present in clusters on the cell surface in the presence of PF4 (D, arrowhead). The micron bar corresponds to 500 nm. Shown are representative images from 2 or more independent experiments.
PF4 promotes aggregation of LDL on the cell surface, outside coated pits.
Electron micrographs of fibroblasts incubated with 5 nM Au-LDL alone (A,C) or 5 nM Au-LDL in the presence of 20 μg/mL PF4 (B,D) for 30 (A,B) or 120 (C,D) minutes at 37°C. The size of the Au particles used was 18 nm. At 30 minutes (A,B) most Au-LDL (arrow) is on the cell surface. In the absence of PF4, LDL is seen in coated pits, whereas, when PF4 is present, LDL was exclusively located outside coated pits. At 120 minutes LDL is primarily located intracellularly in the absence of PF4 (C). LDL is present in clusters on the cell surface in the presence of PF4 (D, arrowhead). The micron bar corresponds to 500 nm. Shown are representative images from 2 or more independent experiments.
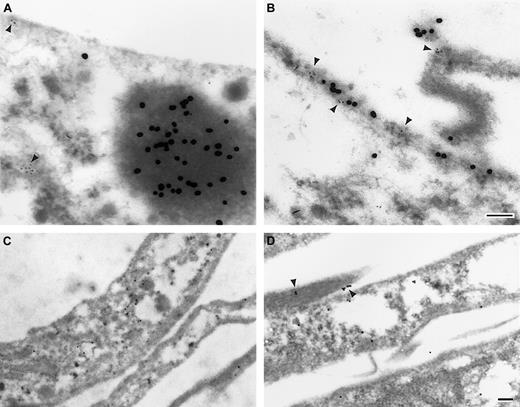
We next examined the localization of LDL-R by using immuno-electron microscopy. Fibroblasts were incubated with LDL in the absence or presence of PF4, and the cells were stained with antibody against LDL-R and/or LDL. These studies confirmed that LDL is retained on the cell surface in clusters only in the presence of PF4 (Figure6B). In the absence of PF4 (Figure 6A), individual LDL-R molecules were identified on the cell surface and small clusters were found within the cell. Although some endocytic compartments appeared to contain both LDL and LDL-R, many contained only one or the other (Figure 6A). This pattern of localization is consistent with the segregation of LDL and LDL-R that normally occurs in endosomal compartments. Small clusters of LDL-R were also found intracellularly in the presence or absence of PF4, presumably molecules recently synthesized and moving toward the cell surface.
PF4 promotes the clustering of LDL and LDL-R detected by immuno-electron microscopy.
Electron micrographs of fibroblasts incubated with 5 nM LDL (A), 5 nM LDL plus 20 μg/mL PF4 (B), buffer (C), or 20 μg/mL PF4 alone (D) for 120 minutes at 37°C. After fixation, LDL was labeled with a polyclonal rabbit anti-apoB100 IgG and 18 nm Au-antirabbit IgG (A,B) from opposite sides of the grid as described in “Materials and methods.” LDL-Rs were labeled with a monoclonal antireceptor immunoglobulin and either 5 nm Au (A,B) or 10 nm (C,D) Au-labeled antimouse immunoglobulin. Clusters of LDL and/or LDL-R (arrowheads) are seen at the cell surface (B,D) in the presence of PF4. LDL-R is seen throughout the cell in the absence of both LDL and PF4. Micron bars correspond to 100 nm. Shown are representative images from 2 or more independent experiments.
PF4 promotes the clustering of LDL and LDL-R detected by immuno-electron microscopy.
Electron micrographs of fibroblasts incubated with 5 nM LDL (A), 5 nM LDL plus 20 μg/mL PF4 (B), buffer (C), or 20 μg/mL PF4 alone (D) for 120 minutes at 37°C. After fixation, LDL was labeled with a polyclonal rabbit anti-apoB100 IgG and 18 nm Au-antirabbit IgG (A,B) from opposite sides of the grid as described in “Materials and methods.” LDL-Rs were labeled with a monoclonal antireceptor immunoglobulin and either 5 nm Au (A,B) or 10 nm (C,D) Au-labeled antimouse immunoglobulin. Clusters of LDL and/or LDL-R (arrowheads) are seen at the cell surface (B,D) in the presence of PF4. LDL-R is seen throughout the cell in the absence of both LDL and PF4. Micron bars correspond to 100 nm. Shown are representative images from 2 or more independent experiments.
What was remarkable, however, was the extensive clustering of LDL-R on the cell surface that was readily apparent when PF4 was present but not in its absence (Figure 6B). Both the coclustering of LDL and LDL-R and the clusters containing predominantly one or the other protein were observed on the cell surface. Because larger gold particles may obscure smaller ones, it is possible that the clusters of LDL seen also contain LDL-R. Of importance, clusters of LDL-R were also observed in the presence of PF4 without LDL present (Figure 6D) but not in the absence of PF4 and LDL (Figure 6C). Staining these sections with anti-ApoB100 confirmed the absence of endogenous LDL (not shown). These data demonstrate that PF4 interacts with LDL-R on the cell surface and modifies its distribution and that of the LDL/LDL-R complex. PF4 causes partitioning of both reactants away from coated pits and promotes their appearance in cell surface aggregates containing either or both proteins.
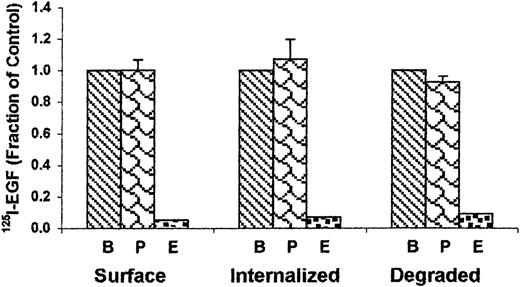
To determine if PF4 was a general inhibitor of clatharin-mediated endocytosis, we examined the behavior of another protein-receptor complex internalized by clatharin-coated pit, EGF. Concentrations of PF4 (20 μg/mL) that almost totally inhibited degradation of LDL had no effect on the binding, internalization, or degradation of125I-EGF (Figure7).52 This outcome indicates that PF4 is not a general inhibitor of clatharin-mediated endocytosis.
PF4 does not inhibit EGF binding or degradation.
125I-EGF (7 nM) was incubated with A431 cells for 4 hours at 37°C either alone (B) or in the presence of 20 μg/mL PF4 (P) or unlabeled 800 nM EGF (E). Data are the mean ± SD of 2 independent experiments performed in triplicate.
PF4 does not inhibit EGF binding or degradation.
125I-EGF (7 nM) was incubated with A431 cells for 4 hours at 37°C either alone (B) or in the presence of 20 μg/mL PF4 (P) or unlabeled 800 nM EGF (E). Data are the mean ± SD of 2 independent experiments performed in triplicate.
PF4 promotes binding of LDL/LDL-R to cellular proteoglycans that are retained on the cell surface
Experiments were then performed to understand the mechanism by which PF4 promotes clustering of LDL and LDL-R on the cell surface. The studies cited above demonstrate that PF4 and LDL can occupy LDL-R simultaneously. Therefore, we asked whether PF4 might act as a bridge between LDL-R and cellular proteoglycans. To explore this possibility, we examined the binding of 125I–sLDL-R to CHO cells lacking endogenous LDL-R, in the absence and presence of PF4. As shown in Figure 8A, PF4, but not NAP-2, promoted the binding of sLDL-R to the cells in a dose-dependent manner (half-maximal binding at approximately 10 μg/mL PF4). Of interest, binding of sLDL-R to the cells in the presence of PF4 was relatively resistant to acid elution, as only 10% of the surface counts were removed by glycine buffer, pH 2.7, suggesting that these complexes are remarkably stable. PF4 did not promote the binding of sLDL-R to XT− cells (Figure 8A), indicating a requirement for proteoglycans.
PF4 promotes the binding of soluble LDL-R to the cell surface.
(A) 125I–sLDL-R (250 nM) was incubated with LDL-R–deficient CHO cells (▪, ▴) or with XT− CHO cells, which lack HS and CS chains (●), in the presence of increasing concentrations of PF4 (▪, ●) or NAP2 (▴; dashed line). (B)125I-LDL (50 nM) was incubated with LDL-R–deficient CHO cells as in (A) in the presence of PF4 (80 μg/mL), sLDL-R (2.5 μM), or both PF4 and sLDL-R. Data are the mean ± SEM of 3 to 6 independent experiments, each performed in triplicate.
PF4 promotes the binding of soluble LDL-R to the cell surface.
(A) 125I–sLDL-R (250 nM) was incubated with LDL-R–deficient CHO cells (▪, ▴) or with XT− CHO cells, which lack HS and CS chains (●), in the presence of increasing concentrations of PF4 (▪, ●) or NAP2 (▴; dashed line). (B)125I-LDL (50 nM) was incubated with LDL-R–deficient CHO cells as in (A) in the presence of PF4 (80 μg/mL), sLDL-R (2.5 μM), or both PF4 and sLDL-R. Data are the mean ± SEM of 3 to 6 independent experiments, each performed in triplicate.
We next asked whether sLDL-R bound to cells complexed with PF4 and proteoglycans retained its capacity to bind LDL, albeit perhaps with a lowered affinity. To test this hypothesis, LDL-R–deficient CHO cells were incubated with 125I-LDL (50 nM) alone or in the presence of sLDL-R ± PF4 (80 μg/mL) (Figure 8B).125I-LDL bound directly to CHO cells, likely to cellular proteoglycans as would be expected at this ligand concentration. Binding of LDL was not enhanced by sLDL-R alone. However, PF4 caused a 2-fold increase in LDL binding to the cells in the presence of sLDL-R, whereas PF4 had no significant effect on LDL binding in the absence of sLDL-R. This increase was not seen in the presence of NAP-2 or on XT− cells lacking proteoglycans (not shown). This experiment demonstrates that complexes can form between LDL and LDL-R that are capable of binding to cell surface proteoglycans in the presence of PF4.
Finally, we examined the elution profile of LDL bound as cell-associated complexes with PF4, LDL-R, and proteoglycans. To do so, LDLR-expressing CHO cells were incubated with 125I-LDL in the presence of PF4 (20 μg/mL) at 37°C, and the elution of LDL was examined. Although LDL and heparin almost completely inhibited the binding of 125I-LDL to the cells initially, less than 10% of the LDL bound to the cells in the presence of PF4 was eluted at 3 hours, in contrast to more than 80% elution by 10 mM EDTA. Consistent with this change in elution profile, the LDL eluted by EDTA comigrated with partially oxidized LDL on native agarose gel electrophoresis (not shown).
Discussion
This study demonstrates that PF4 inhibits the degradation of LDL by LDL-R–expressing cells through 2 interrelated mechanisms. First, PF4 acts by binding to the LDL-R, partially inhibiting the binding of LDL. Second, PF4 frustrates endocytosis of the LDL-Rs themselves. The net effect is a clear inhibition of LDL degradation at concentrations of PF4 likely to be achieved at sites of vascular disease, where platelet activation occurs and PF4 is concentrated along vascular proteoglycans.14 15
Our studies both confirm, in part, and extend the finding that PF4 inhibits LDL binding to the LDL-R.20 Our data show for the first time that PF4 binds with high affinity to the ligand-binding region (domains 1-7) of LDL-R in a Ca++-dependent process, similar to the requirements for LDL binding. Binding of PF4 to LDL-R is likely to be complex and requires further study for several reasons. First, sLDL-R contains several LDL-binding motifs. Which of these accommodate the smaller PF4 molecule is unknown. Second, monomeric PF4 exists in a dynamic equilibrium with itself, reversibly forming dimers and tetramers.43,53 This equilibrium is affected by PF4 concentration, pH, and ionic strength43,53and possibly by binding to the LDL-R. Third, PF4 forms higher ordered complexes in the presence of anionic proteoglycans54 that may affect this equilibrium and its interaction with LDL-R.
Interestingly, PF4 does not completely inhibit binding of LDL to LDL-R on cells or in a purified system, even at concentrations as high as 80 μg/mL, as would be predicted if the cationic residues in the ligands competed for the same epitopes in the receptor. Said another way, at concentrations that inhibit degradation maximally, LDL-R retains the capacity to bind approximately half as much LDL as in the absence of PF4. In addition, the cationic platelet α-granule protein NAP-2, which bears 60% homology to PF4 at the amino acid level, did not inhibit LDL binding to LDL-R nor did a PF4 variant bearing 4 critical amino acid mutations. Moreover, LDL does not inhibit the binding of PF4 to LDL-R. Taken together, these studies demonstrate that PF4 does not behave as a competitive inhibitor of LDL binding to LDL-R. PF4 may bind to an independent binding site in LDL-R, inducing a conformational change that makes it less accommodating to LDL. This conclusion is further supported by the inability of LDL to inhibit the binding of PF4 to the receptor. These observations are in line with previous findings that protamine is a noncompetitive inhibitor of LDL binding to LDL-R–expressing cells.20
The observation that HS- and CS-containing proteoglycans must be present for PF4 to inhibit LDL binding to LDL-R–expressing cells provides additional support for the hypothesis that inhibition is more complex than a simple competition between reactants. The requirement for proteoglycans was demonstrated by enzymatic removal of HS and/or CS from WT LDL-R transfectants, through analysis of genetic variants unable to synthesize one or both glycosaminoglycans and through study of PF4 variants with diminished or absent binding to heparin.
Our data show that removal of CSs from the cell surface is somewhat more detrimental to the inhibitory effects of PF4 than is removal of HSs. That PF4 is neither internalized nor degraded in our experiments is also consistent with binding to CSs, which in contrast to HS-containing proteoglycans, such as syndecan-1, are internalized slowly if at all.26 Additionally, it has been shown that PF4 binds specifically to CSs on neutrophils55,56 and within platelet α-granules.12
The major effect of proteoglycans on the behavior of PF4 is likely to involve changes in the behavior of the LDL-R itself. This interpretation is consistent with effects of PF4 on fibroblast growth factor and vascular endothelial growth factor receptors.57 58 PF4 profoundly alters the subcellular distribution of LDL-R as well as LDL/LDL-R complexes as visualized by electron microscopy. Residual LDL bound in the presence of PF4 is located almost exclusively (> 90%) in macromolecular clusters or in aggregates on the cell surface. Some of these clusters appear to contain LDL bound to LDL-R, whereas others appear to contain only one or the other reactant. The biochemical composition of LDL in these aggregates and the extent of its affiliation with LDL-R or other lipoprotein receptors will require additional study as well.
It is clear that both LDL- and LDL-R–containing aggregates are excluded from clatharin-coated pits. However, PF4 does not cause a general disruption of their morphology or function. Coated pits were readily visualized on cells incubated with PF4, and PF4 had no effect on the degradation of EGF through this pathway. Rather, PF4 appears to prevent LDL-R from entering the coated pits. It is anticipated that such a marked effect on LDL-R entry into coated pits by PF4 would inhibit the rapid internalization and degradation of LDL through this, its primary catabolic pathway. These morphologic studies thereby help us to understand how PF4 inhibits LDL degradation to a greater extent than it inhibits LDL binding at each concentration tested.
The mechanism by which PF4 inhibits LDL-R entry into coated pits will also require additional investigation to unravel. Because sLDL-R used in this study does not contain the cytoplasmic domain previously reported to be involved in receptor self-association,59the mechanism by which PF4 induces clustering must differ. We postulate that PF4 forms high molecular weight oligomeric complexes with specific cellular proteoglycans, consistent with their purported interaction with CS and HS eluted from the surface of neutrophils.55Such PF4-proteoglycan complexes appear capable of binding several molecules of LDL-R and/or LDL simultaneously, thereby generating a scaffold on which LDL and/or LDL receptors cluster. Support for this concept comes from our finding that PF4 promotes the binding of soluble LDL-R to WT CHO cells but not to cells genetically incapable of synthesizing HS and CS side chains. Furthermore, complexes between PF4, sLDL-R, and cellular proteoglycans retain the capacity to bind, but not to internalize and degrade, LDL. LDL bound in these complexes loses its capacity to be eluted by LDL and comigrates with partially oxidized LDL on native gels.
Taken together, these studies demonstrate that PF4 inhibits the degradation of LDL at least in part by modulating the behavior of the LDL-R. We propose a model in which PF4 binds directly to LDL-R and decreases LDL binding to the receptor through a noncompetitive mechanism that involves association with proteoglycans. Binding to proteoglycans not only increases the local concentration of PF4 and its propensity to interact with LDL-R but leads to the formation of high molecular complexes that can cross-link LDL-R and possibly LDL or “modified” LDL. In the presence of PF4, macromolecular clusters of LDL-R and LDL form on the cell surface that are incapable of migrating into clatharin-coated pits. A substantial fraction of the residual-bound LDL becomes trapped within PF4/proteoglycan complexes that are endocytosed slowly, if at all. The increased residence time of LDL on the cell surface afforded by PF4 is likely to facilitate lipoprotein aggregation, oxidation, and other modifications that promote foam cell formation.10 60-62
PF4 has been reported to act as a chemoattractant for monocytes promoting differentiation into tissue macrophages.63Activated macrophages release soluble mediators that stimulate platelet aggregation and secretion,64 generating a positive feed-forward system of mutual cell activation that would be predicted to enhance the atherogenic process. Our finding that atherosclerotic lesions contain abundant PF465 provides additional support for involvement of this chemokine in lesion development. Studies are in progress in mice that lack PF4 and that overexpress PF4 to test this hypothesis in vivo. The recent development of potent inhibitors of platelet activation that may be amenable to chronic use underscores the importance of delineating the contribution of platelets to the development of atherosclerosis. Understanding the biochemical basis of PF4–LDL-R interaction may provide a new locus for pharmacologic intervention.
Supported in part by grants K08HL04245, HL58107, P50H54500, HL58884, and HL38956.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Bruce S. Sachais, Department of Pathology and Laboratory Medicine, 207A John Morgan Bldg, 3620 Hamilton Walk, Philadelphia, PA 19104; e-mail: Sachais@mail.med.upenn.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal