Issue Archive
Table of Contents
BLOOD COMMENTARIES
PERSPECTIVE
Gene therapy for HbSC disease and other compound heterozygous sickle hemoglobinopathies: a time for inclusion
Gene therapy is entering routine clinical practice for patients with sickle cell disease due to the most common genetic subtypes, hemoglobin S (HbS) gene homozygotes and HbS-β0 thalassemia. Wilks et al provide a perspective on why gene therapy should also be considered for patients with severe sickle cell disease due to compound heterozygosity for HbS and HbC (HbSC).
IMMUNOBIOLOGY AND IMMUNOTHERAPY
Deciphering neutrophil dynamics in the focal lesion tumor microenvironment to overcome immunosuppression in multiple myeloma
Myeloid cells in the bone marrow are increasingly recognized as modulators of malignant cell behavior. Using patient multiple myeloma samples and murine models, Rivera et al demonstrate that aberrant mature neutrophil populations can promote myeloma by inhibiting T-cell proliferation and that this can be therapeutically reversed by CXC chemokine receptor 2 (CXCR2) inhibition. These data illuminate the complexity of interactions between myeloma cells and different cells within the bone marrow microenvironment.
LYMPHOID NEOPLASIA
The impact of fitness and dose intensity on clinical outcomes with venetoclax-obinutuzumab in CLL
Clinical Trials & Observations
The combination of obinutuzumab for 8 infusions and venetoclax for 1 year is a standard first-line therapy for patients with chronic lymphocytic leukemia (CLL). Through rigorous comparison across 2 sequential German CLL study group randomized trials, Al-Sawaf and colleagues demonstrate that outcomes with this regimen are excellent, regardless of fitness status. Safety and efficacy are similar between patients with cumulative illness rating scale scores of >6 or reduced creatinine clearance (unfit patients) and those fit patients with neither. Unfit patients require more dose reductions, but these do not impact efficacy unless venetoclax dosing is reduced by more than 30%. These data reinforce the applicability of this regimen for most patients with CLL requiring initial therapy.
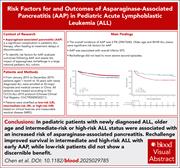
Risk factors and outcomes of asparaginase-associated pancreatitis in pediatric patients with ALL
Clinical Trials & Observations
MYELOID NEOPLASIA
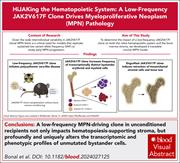
HiJAKing the hematopoietic system: a low-frequency JAK2V617F clone drives myeloproliferative neoplasm pathology
The activating mutation JAK2V617F causes clonal hematopoiesis and myeloproliferative neoplasms (MPNs) but can be present in a minority of cells. Using an immunocompetent murine model of low-level chimerism, Bonal et al addressed how small clones of cells with JAK2V617F cause disease. They show that JAK2V617F cells significantly affect the bone marrow microenvironment and unmutated hematopoiesis, together skewing the whole hematopoietic system toward an MPN-like phenotype. These data help explain MPN development and why some clinical features may persist despite effective reductions in JAK2V617F clone size with therapy.
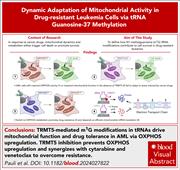
Disrupting tRNA modifications to target mitochondrial vulnerabilities in drug-resistant leukemia cells
PLATELETS AND THROMBOPOIESIS
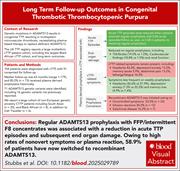
Long-term follow-up outcomes in congenital thrombotic thrombocytopenic purpura
Clinical Trials & Observations
Congenital thrombotic thrombocytopenic purpura (cTTP) is the hereditary form of TTP and is characterized by biallelic mutations in ADAMTS13 resulting in severe ADAMTS13 deficiency. Stubbs et al provide detailed longitudinal follow-up data for nearly 100 patients from a multiethnic registry in the United Kingdom, reporting 16 new ADAMTS13 variants. Postdiagnosis prophylaxis with plasma products or recombinant ADAMTS13 reduces recurrences and end-organ damage, including stroke and renal dysfunction.
THROMBOSIS AND HEMOSTASIS
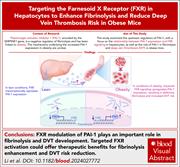
Targeting FXR in hepatocytes: a promising approach to enhance fibrinolysis and reduce deep vein thrombosis risk
Obesity increases the risk of venous thrombosis and is commonly associated with an increase in plasma levels of plasminogen activator inhibitor 1 (PAI-1), a key inhibitor of fibrinolysis. Li et al report that tropifexor, an experimental farnesoid X receptor (FXR) agonist, reduces obesity-associated impairment of fibrinolysis through modulation of hepatic PAI-1 expression in murine models of venous thrombosis. Clinical studies will be necessary to assess the therapeutic potential of targeting the FXR/PAI-1 pathway to improve fibrinolysis and reduce deep vein thrombosis risk.
TRANSFUSION MEDICINE
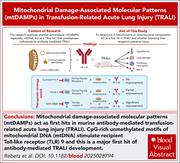
Mitochondrial DNA via recipient TLR9 acts as a potent first hit in murine transfusion-related acute lung injury
Patients in intensive care with an acute illness associated with systemic inflammation are known to be at highest risk for transfusion-related acute lung injury (TRALI). This is speculated to be because TRALI seems to be a “2-hit” phenomenon, with transfusion being the second hit and inflammation the first. Rebetz and colleagues investigated mechanisms underpinning the first hit in elegant murine models, finding that mitochondrial DNA stimulates recipient Toll-like receptor 9 (TLR9) to instigate pulmonary damage, with TLR9 antagonism preventing murine TRALI. These data increase our understanding of how TRALI develops and provide a novel therapeutic target to reduce TRALI in patients.
BLOOD WORK
ERRATA
-
Cover Image
Cover Image
![issue cover]()
Hematoxylin and eosin-stained femur section from a 10-week-old B6N.129S6(SJL)-Jak2tm1.2Ble/AmlyJ mouse crossed with a B6.Cg-Tg(Mx1-cre)1Cgn/J mouse displaying hypercellular bone marrow, consistent with a polycythemia vera-/essential thrombocythemia-like phenotype. See the article by Bonal et al on page 2428.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals


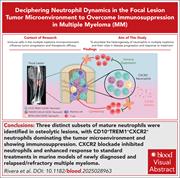


Guardians of the tumor microenvironment: the neutrophil saga