Abstract
The long form of B-cell lymphoma-x (Bcl-xL), an outer mitochondrial membrane protein, has been proposed to mediate the antiapoptotic action of erythropoietin on erythroid progenitor cells and to be necessary for heme synthesis in erythroblasts. Mice with conditional knockout of Bcl-xL (conditional bcl-x-/- mice) develop severe anemia that has been attributed to hemolysis and is accompanied by splenomegaly. We characterized further the anemia of conditional bcl-x-/- mice and investigated the role of Bcl-xL in the action of erythropoietin and in heme synthesis. We analyzed peripheral blood cells and cultured splenic erythroblasts of conditional bcl-x-/- mice and littermates that were rendered anemic by bleeding. Although they had massive splenic erythroblastosis, conditional bcl-x-/- mice had decreased circulating reticulocytes compared to littermates even prior to bleeding the littermates. Compared to erythroblasts of bled littermates, bcl-x-/- erythroblasts cultured with erythropoietin underwent apoptosis during the later, hemoglobin-synthesizing stages of differentiation. The bcl-x-/- erythroblasts synthesized heme, but at reduced rates compared to bled littermate erythroblasts. When cultured without erythropoietin, bcl-x-/- erythroblasts underwent apoptosis at early stages of differentiation, prior to hemoglobin synthesis. Bcl-xL is not required for heme synthesis and does not mediate the antiapoptotic effects of erythropoietin, but it prevents ineffective erythropoiesis due to apoptosis in late-stage, hemoglobin-synthesizing erythroblasts. (Blood. 2005;106:1857-1863)
Introduction
Normal erythrocyte production is a function of the proliferation, death, and differentiation of erythroid progenitor cells. Erythropoietin (EPO) is the principal trophic hormone that controls red cell production by regulating apoptosis of erythroid progenitor cells.1 Erythroid colony-forming units (CFU-Es) and their immediate progeny, proerythroblasts, are EPO-dependent stages of erythroid development.1-3 When EPO levels are insufficient, CFU-Es and proerythroblasts undergo apoptosis.
Bcl-xL, an antiapoptotic member of the B-cell lymphoma (Bcl-2) family of proteins, is associated with the outer mitochondrial membrane. Bcl-xL forms heterodimers with proapoptotic members of the Bcl-2 family and inhibits their apoptotic action.4,5 Others have suggested that Bcl-xL has a direct action on the ion channels of the mitochondrial membrane.6,7 In the presence of EPO, Bcl-xL is up-regulated in erythroblasts8 and in EPO-sensitive cell lines.9 This induction of Bcl-xL has been proposed to be the primary mediator of the antiapoptotic effect of EPO during erythroid differentiation.10,11
In mice, Bcl-xL deficiency is lethal at embryonic day 13.5 due to failure of definitive hematopoiesis in the liver and neuronal apoptosis in the brain.12 Murine embryonic stem (ES) cells in which both bcl-x alleles are disrupted give rise to erythroid colonies in which the cells die at a late stage of maturation.13 The bcl-x-/- ES cells do not contribute to definitive erythropoiesis when injected into the blastocysts that form chimeric mice.13 Bcl-xL deficiency in hematopoietic progenitor cells of mice that acquire it postnatally by a conditional knockout strategy (conditional bcl-x-/- mice) has been associated with severe anemia, splenomegaly, and thrombocytopenia.14 The bone marrow and spleens of these mice accumulate Bcl-xL-deficient erythroblasts, suggesting that the anemia results from a defect14 at the stage of mature erythroblasts or later. Wagner et al14 have proposed that much of this failure occurs after enucleation, that is, it is a hemolytic anemia, because they found that blood reticulocyte numbers were increased. In murine erythroleukemia (MEL) cells induced to differentiate by dimethyl sulfoxide, cell loss appeared to be at an earlier stage than reticulocytes, specifically the mature erythroblast, because inhibition of Bcl-xL resulted in loss of both benzidine-positive cells and heme biosynthesis.15 Loss at this mature erythroblast stage is consistent with the death of mature cells in erythroid colonies derived from ES cells,13 the evidence of cell debris in the spleens of conditional bcl-x-/- mice,14 and our previous studies, showing that Bcl-xL is up-regulated at the terminal stages of erythroblast differentiation,8 when hemoglobin synthesis is maximal.16
We have previously used a system of explanted erythroid cells from spleens of mice infected with the anemia-inducing strain of Friend leukemia virus (FVA cells) to study the EPO-dependent and subsequent stages of erythropoiesis in vitro.16 Anemias in mice with normal EPO production capacities lead to increased erythropoiesis that expands erythroid progenitor and precursor cells in the spleen.17,18 In the present study, we used a similar purification and culture system to that used previously with FVA cells to analyze the differentiation of splenic erythroblasts from severely anemic conditional bcl-x-/- mice and from their normal littermates that had a moderately severe anemia induced by bleeding. Our results show that (1) Bcl-xL plays a key role in the survival of the late-stage erythroblasts in all phases of cell cycle, that is, Bcl-xL deficiency results mainly in ineffective erythropoiesis rather than hemolytic anemia; (2) Bcl-xL does not mediate the antiapoptotic effect of EPO early stage erythroblasts; and (3) despite having its greatest antiapoptotic effect during the stage of hemoglobin synthesis, Bcl-xL is not required for heme synthesis because heme synthesis occurs at a reduced level in Bcl-xL-deficient erythroblasts.
Materials and methods
Mice
All experiments were approved by the Vanderbilt University Animal Care Committee. The conditional bcl-x-/- mice examined in this study were genetically identical to those analyzed by Wagner et al.14 Transgenic mice harboring a gene for the Cre recombinase enzyme of bacteriophage P1 were mated with mice that were homozygous for a bcl-x allele that was flanked by loxP sequences (bcl-x fl, a target for Cre-mediated recombination). The breeder mice containing the cre gene and the breeder mice containing the bcl-x fl gene were obtained from Dr. Ed Rucker of the University of Missouri (Columbia, MO). The cre gene was transcribed under the control of a mouse mammary tumor virus promoter that was up-regulated by reproductive steroid hormones (CreD mice). After the onset of production of reproductive steroid hormones, mice homozygous for bcl-x fl had the bcl-x gene deleted in creD-expressing cells, which included erythroid progenitor cells.14 Analyses of bcl-x fl and creD genes were performed with DNA from tail tissue and amplified by polymerase chain reaction using previously described primers.14 Control mice were littermates of conditional knockout animals that were homozygous for bcl-x fl, but lacked cre.
Analysis of peripheral blood
Three- to 9-month-old conditional bcl-x-/- mice were bled from the retro-orbital sinus to obtain blood for analyses prior to being killed. Some control mice were bled 0.5 mL and given intraperitoneal injections of an equal volume of sterile saline 4, 3, and 2 days prior to being killed to induce anemia and increase splenic erythropoiesis. Blood was collected in heparinized capillary tubes, diluted with phosphate-buffered saline (PBS) containing 1 mM EDTA (ethylenediaminetetraacetic acid), and analyzed for complete blood counts, reticulocytes, and reticulocyte maturity distributions19 using an Advia 120 automated cell counter (Bayer, Tarrytown, NY).20 Plasma samples were collected from centrifuged aliquots of blood for bilirubin determinations using a Beckman Coulter LX20 Chemistry Analyzer (Fullerton, CA).
Measurement of erythroid precursors in vivo
Spleens and femurs were removed from killed conditional bcl-x-/- mice, healthy controls, and bled controls. Spleens were weighed, sectioned, and filtered through nylon mesh to disperse the cells. Femurs were flushed with PBS with a 25-gauge needle to collect marrow cells. Splenic and bone marrow nucleated cells were stained with 0.25% methylene blue in 25% ethanol and counted with a hemacytometer. Total bone marrow nucleated cells were calculated based on one femur containing 7% of the total mouse marrow cells.21-25 Aliquots of nucleated cells from each spleen and marrow were suspended in 2% fetal bovine serum (FBS) in PBS to block nonspecific binding and labeled with R-phycoerythrin-conjugated antibodies to TER-119 (Becton Dickinson, San Jose, CA) on ice for 30 minutes. TER-119 is an erythroid-specific marker expressed from the proerythroblast stage through the mature erythrocyte.26 The cells were fixed with 2% paraformaldehyde in PBS on ice for 20 minutes and permeabilized in 70% ethanol/30% PBS. Double-stranded DNA ends were fluorescently labeled by terminal deoxynucleotidyl transferase-deoxyuridine triphosphate (dUTP) nick-end labeling (TUNEL) using fluorescein isothiocyanate (FITC) conjugated to dUTP (Boehringer Mannheim, Indianapolis, IN).27,28 The cells were labeled with 7-amino-actinomycin D (7-AAD; Molecular Probes, Eugene, OR), a fluorescent nucleic acid-binding dye, and analyzed by fluorescence-activated cell sorting (FACScan; Becton Dickinson) to determine the percentage of erythroid (PE+), nucleated (7-AAD+), and apoptotic (FITC+) cells. Data were analyzed using Modfit DNA modeling software linked to Winlist (both from Verity Software House, Topsham, ME). Percentages of nucleated TER-119+ and TER-119+/TUNEL+ cells in spleen or marrow samples were multiplied by the total nucleated cell numbers for each respective organ to determine the total number of nucleated erythroid and apoptotic nucleated erythroid cells in spleen, bone marrow, and in the total body (sum of spleen and marrow for each mouse).
Isolation and culture of erythroblasts
Spleen cells from one conditional bcl-x-/- mouse or pooled from 3 bled control mice were separated at 4°C by velocity sedimentation at unit gravity on continuous 1% to 2% bovine serum albumin (BSA) gradients.16 Rapidly sedimenting cells that were highly enriched with erythroblasts were cultured at 106 cells/mL in Iscove modified Dulbecco medium (IMDM) containing 1% deionized BSA, 30% FBS, 100 μg/mL streptomycin, 100 U/mL penicillin G, 0.1 mM α-thioglycerol, and 10 U/mL recombinant human EPO (OrthoBiotech, Bridgewater, NJ). In some experiments, EPO was not added to the culture medium. Cells were harvested from cultures at 0, 8, 20, 32, and 44 hours.
Analysis of proliferation and differentiation
To determine numbers of total nuclei (in erythroblasts and extruded nuclei), aliquots of harvested cell suspensions were counted with a hemacytometer as described (see “Measurement of erythroid precursors in vivo”). Viable cell numbers were calculated by multiplying the total nucleated cell numbers by the proportion of nonapoptotic (see “Analysis of apoptosis and cell-cycle phases of cultured cells”) cells. Cytocentrifuge preparations were stained with 3,3′-dimethoxybenzidine and hematoxylin and viewed with an Olympus BH-2 microscope using an SPlan 100, oil immersion, × 100 objective having a 1.25 numeric aperture (Olympus America, Melville, NY). At least 1000 cells were counted per slide to determine the percentages of erythroblasts, reticulocytes, and extruded nuclei. Numbers of reticulocytes per milliliter culture were calculated from these differential counts and the numbers of total nuclei as determined from methylene blue counts. Photomicroscopy was performed with an Olympus C-35AD-4 camera (Olympus America) using Ektachrome 64T film (Eastman-Kodak, Rochester, NY). Developed film was scanned with a Nikon Coolscan V ED (Nikon, Melville, NY), and scanned images were processed in Adobe Photoshop 7.0 (Adobe Systems, San Jose, CA).
Analysis of apoptosis and cell-cycle phases of cultured cells
Harvested cells were rinsed in PBS, fixed in 1% paraformaldehyde,27 permeabilized in 70% ethanol, and stored at -20°C until analyzed. Fixed, permeabilized cells were processed for TUNEL assays and stained for DNA content in PBS containing 40 μg/mL propidium iodide (Sigma, St Louis, MO). Flow cytometry was used to determine the percentage of apoptotic cells and the phases of cell cycle by quantifying DNA by the propidium staining of individual cells.
Western blot analysis
Harvested cells were rinsed in PBS, counted in methylene blue, pelleted, and lysed in 2 × Laemmli sample buffer.29 Protein content of an aliquot of cells was determined with the Bradford method.30 Samples were sonicated, heated to 95°C for 10 minutes, and electrophoretically separated on sodium dodecyl sulfate-polyacrylamide gels. Proteins were electrophoretically transferred to polyvinylidene fluoride membranes (Schleicher and Schuell, Keene, NH). The membranes were incubated with primary antibodies to Bcl-x (Becton Dickinson; catalogue no. 610212) and Bax (Upstate Biotechnology, Lake Placid, NY; catalogue no. 06-499). After washing, the membranes were incubated with species-specific secondary antibodies conjugated to horseradish peroxidase that were detected by chemiluminescence using a kit (Amersham, Piscataway, NJ).
Analysis of heme synthesis
Transferrin-bound 59Fe was prepared by incubating 4.8 mg human apotransferrin (Sigma) and 20 μCi (0.74 MBq) 59FeCl3 (1.7 Ci/mmol [63GBq] Fe, Amersham) in 0.2 mL 0.25 M Tris (tris(hydroxymethyl)aminomethane)-HCl (pH 8) and 10 mM NaHCO3 for 1 hour at 25°C. After incubation, 1.8 mL IMDM was added and the solution stored at 4°C. At various times, 50 μL transferrin-bound 59Fe solution was added to quadruplicate 0.5-mL cultures of erythroblasts. Two hours later, erythroblasts were harvested, pelleted by centrifugation, and lysed in 1.8 mL Drabkin solution (Sigma). After acidification with 0.2 mL 1 N HCl, 2 mL cyclohexanone was added and each sample mixed vigorously. Samples were separated into lower aqueous phase and upper cyclohexanone phase by centrifugation. Aliquots of the cyclohexanone phase containing the extracted heme were counted with a well-type γ counter.
Statistical analyses
Statistical analyses were done with SPSS for Windows, version 12.0 (SPSS, Chicago, IL). Statistical significance (P < .05) was determined by the independent-sample t test.
Results
Conditional bcl-x-/- mice have ineffective erythropoiesis
After 2 months of age, the conditional bcl-x-/- mice began to develop anemia and palpable splenomegaly, but they appeared healthy. After 4 months of age, they were less active than their healthy littermates, and they had pale ears and tails. Phenotypic parameters at the time the mice were killed are shown in Table 1. Conditional bcl-x-/- mice had a mean spleen mass of 5.2 g, whereas that of healthy control littermates was 0.1 g (P < .001) and that of bled controls was 0.3 g (P < .001).
The mean hemoglobin level of conditional bcl-x-/- mice was 4.3 g/dL compared to 15.8 g/dL in healthy controls (P < .001) and 6.5 g/dL in bled controls (P < .001). Similar differences were found in respective erythrocyte numbers (Table 1). The conditional bcl-x-/- mice had mean reticulocyte counts of 1.5 × 105/μL, which were significantly lower than unbled healthy control mice with a mean count of 2.7 × 105/μL (P < .001) and bled controls with a mean count of 14.0 × 105/μL (P < .001). The lower than normal reticulocyte counts in conditional bcl-x-/- mice indicated that Bcl-xL deficiency primarily caused anemia through deficient erythrocyte production rather than hemolysis. Peripheral blood smears of these mice did not show schistocytes, spherocytes, or erythrocyte fragments. Healthy control mice had only 10% early stage reticulocytes, with predominantly middle stage (40%) and late stage (50%) reticulocytes (Table 1). After bleeding of control mice, the distribution shifted to early reticulocytes (63%), similar to the distribution pattern seen in the conditional bcl-x-/- mice (55%). The mature erythrocytes of the bcl-x-/- mice were significantly larger than the mature erythrocytes of the bled and unbled controls (Table 1), consistent with macrocytosis that is often found in other types of ineffective erythropoiesis. Indirect hyperbilirubinemia in conditional bcl-x-/- mice (Table 1) indicated extensive destruction of hemoglobin-containing cells.
Analyses of the spleen and bone marrow cells further substantiated that the anemia of conditional bcl-x-/- mice is due primarily to ineffective erythropoiesis. Table 2 shows that the total body numbers of TER-119+ cells were 11-fold greater in conditional bcl-x-/- mice compared to bled controls and 33-fold greater compared to unbled controls. A significantly larger percentage of TER-119+ erythroid precursors was apoptotic in conditional bcl-x-/- mice (12%) compared to bled (4%, P < .001) or unbled (2%, P < .001) controls.
Bcl-xL-deficient erythroblasts respond to EPO but undergo apoptosis at later stages
Splenic cells from conditional bcl-x-/- mice were cultured with and without EPO and compared to splenic cells from bled controls. The splenic cells were 90% or more erythroblasts in all experiments for both conditional bcl-x-/- and bled control mice. Cells cultured with EPO were harvested at 0, 8, 20, 32, and 44 hours, but the bcl-x-/- erythroblasts without EPO were not examined at 44 hours because preliminary studies showed that more than 90% of cells were dead at this time. Harvested erythroblasts were fixed and stained for TUNEL assays (Figure 1A). When cultured with EPO, erythroblasts from conditional bcl-x-/- mice had significantly increased apoptosis percentages compared to bled controls at 8 hours (29% versus 12.2%, P < .001), 20 hours (45.5% versus 19%, P < .001), 32 hours (56.6% versus 20.5%, P < .001), and 44 hours (80.9% versus 30%, P < .001). When cultured without EPO, bcl-x-/- erythroblasts had increased percentages of apoptotic cells compared to the same cells cultured with EPO at 8 hours (44.6% versus 29%, P < .04), 20 hours (70.7% versus 45.5%, P < .01), and 32 hours (82.7% versus 56.6%, P < .01). Thus, despite having a marked increase in apoptosis at all times of culture with EPO when compared to erythroblasts of bled control mice, bcl-x-/- erythroblasts cultured with EPO had significantly reduced apoptosis at all times compared to the same cells cultured without EPO. These results demonstrate that some of the antiapoptotic effects of EPO are functional in erythroblasts in the absence of Bcl-xL.
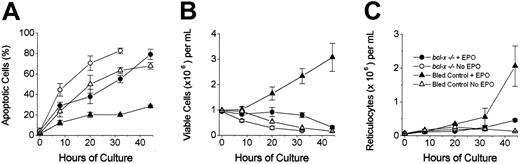
Apoptosis, viable cell counts, and reticulocyte production of cultured erythroblasts from conditional bcl-x-/- mice. (A) Percentage of TUNEL+ cells. (B) Viable cell numbers and (C) reticulocyte numbers from cultures of erythroblasts from conditional bcl-x-/- mice with EPO (•) or without EPO (○) and of erythroblasts from bled littermate controls with EPO (▴) and without EPO (▵). Data are mean ± SEM of 3 (controls) and 7 (conditional bcl-x-/-) independent experiments.
Apoptosis, viable cell counts, and reticulocyte production of cultured erythroblasts from conditional bcl-x-/- mice. (A) Percentage of TUNEL+ cells. (B) Viable cell numbers and (C) reticulocyte numbers from cultures of erythroblasts from conditional bcl-x-/- mice with EPO (•) or without EPO (○) and of erythroblasts from bled littermate controls with EPO (▴) and without EPO (▵). Data are mean ± SEM of 3 (controls) and 7 (conditional bcl-x-/-) independent experiments.
Numbers of viable erythroblasts are shown in Figure 1B. Bled control erythroblasts cultured with EPO accumulated due to proliferation with a relatively low rate of apoptosis. The bcl-x-/- erythroblasts cultured with EPO maintained a steady number through 32 hours due to balanced rates of cell proliferation and apoptosis. Between 32 and 44 hours, however, the number of viable erythroblasts fell sharply due to further increases in apoptosis in cultures of bcl-x-/- cells. The difference in viable cell numbers between bcl-x-/- erythroblasts and bled control erythroblasts cultured with EPO was significant at 20 hours (P < .03) and later (P < .01 at both 32 hours and 44 hours). Both bled control erythroblasts and bcl-x-/-erythroblasts cultured without EPO showed a rapid decline in numbers due to early death by apoptosis (Figure 1B). The difference in viable cell numbers between bcl-x-/-erythroblasts cultured with and without EPO was significant (P < .01) at 8, 20, and 32 hours.
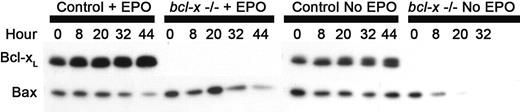
Figure 2 shows Western blots of whole cell lysates. The expression of Bcl-xL increased over time in the erythroblasts from bled controls. The bcl-x-/-erythroblasts did not express Bcl-xL at the level of sensitivity of these Western blots. Bax, a proapoptotic member of the Bcl-2 family of proteins, was present at all times of culture in all 3 groups of erythroblasts. The expression of Bax remained steady in erythroblasts of bled controls but decreased in erythroblasts from conditional bcl-x-/- mice.
Western blots of whole cell lysates from cultured erythroblasts of conditional bcl-x-/- mice and bled littermate controls. Bcl-xL is a 29-kDa protein, and Bax is a 21-kDa protein; 40 μg protein was loaded per lane.
Western blots of whole cell lysates from cultured erythroblasts of conditional bcl-x-/- mice and bled littermate controls. Bcl-xL is a 29-kDa protein, and Bax is a 21-kDa protein; 40 μg protein was loaded per lane.
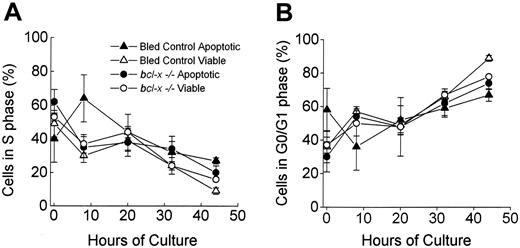
Figure 3 shows the percentage of cells in S phase (A) or G0/G1 phase (B) of the cell cycle at various times in culture. Viable bcl-x-/- erythroblasts had similar percentages at each time of culture when compared to either the viable bled control erythroblasts or the apoptotic bcl-x-/- erythroblasts. Each of these 3 erythroblast populations had approximately 50% of 0-hour erythroblasts in S phase (Figure 3A) indicating an actively proliferating population of erythroblasts. With passage of time in culture each of these 3 erythroblast populations had fewer cells in S phase, and the majority accumulated in G0/G1 phase (Figure 3B). These changes in cell cycle phase between 0 hour and later times (32 hours and 44 hours) were statistically significant (P < .05). This pattern is characteristic of differentiating erythroblasts, which rapidly proliferate until the late stages of differentiation, when they accumulate in a G0/G1 state prior to enucleation.27 The apoptotic bled control erythroblasts showed a similar trend with time but did not reach significance due to large variations in the 0-hour and 8-hour times. These variations are due to the low numbers of apoptotic cells in these cultures. The percentages of apoptotic versus viable cells in G0/G1 and S phases at each time examined were not significantly different, indicating that apoptosis occurred proportionally in all phases of cell cycle in bcl-x-/- erythroblasts and control erythroblasts, despite much higher apoptosis rates in the bcl-x-/- erythroblast populations.
Cell cycle phase of viable and apoptotic erythroblasts from conditional bcl-x-/-mice and bled littermate controls during culture with EPO. Percentage of cells in DNA synthesis (S phase; panel A) or in Gap 0/Gap 1 (G0/G1) phase (panel B) at various times of culture was determined for apoptotic (TUNEL+) and nonapoptotic (TUNEL-) cells. Results are mean ± SEM of 3 (controls) to 7 (conditional bcl-x-/-) independent experiments.
Cell cycle phase of viable and apoptotic erythroblasts from conditional bcl-x-/-mice and bled littermate controls during culture with EPO. Percentage of cells in DNA synthesis (S phase; panel A) or in Gap 0/Gap 1 (G0/G1) phase (panel B) at various times of culture was determined for apoptotic (TUNEL+) and nonapoptotic (TUNEL-) cells. Results are mean ± SEM of 3 (controls) to 7 (conditional bcl-x-/-) independent experiments.
bcl-x-/- erythroblasts produce fewer reticulocytes in vitro
Figure 1C shows that erythroblasts from bled controls cultured with EPO had prominent reticulocyte formation between 32 and 44 hours, yielding nearly 2 × 106 reticulocytes/mL culture at 44 hours. Even greater numbers of reticulocytes were formed in these cultures by 50 hours because most of the cells viable at 44 hours (70%) completed maturation and enucleated (data not shown). Compared to bled control erythroblasts, erythroblasts from conditional bcl-x-/- mice produced many fewer reticulocytes when cultured with EPO for 44 hours (0.5 × 106 reticulocytes/mL, P < .01). By 44 hours of culture, more than 80% of the bcl-x-/- cells cultured with EPO were dead, and no additional reticulocytes were produced after that time.
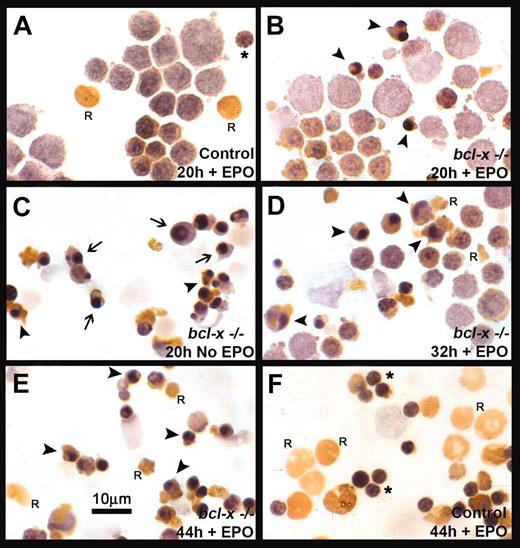
The fate of the bcl-x-/- proerythroblasts during their differentiation was determined by examining the morphologic appearance of the cultured cell populations. Whether obtained from conditional bcl-x-/- mice or controls, the majority of splenic cells at the initiation of culture (0 hours) were early erythroblasts, but a minority had initiated hemoglobin synthesis as detected by benzidine staining and had a more mature morphologic appearance. Erythroblasts from bled control mice at 20 hours of culture with EPO are shown in Figure 4A, whereas erythroblasts from bcl-x-/- mice cultured for 20 hours with EPO are shown in Figure 4B and those without EPO are shown in Figure 4C. At 20 hours of culture, the bcl-x-/- and bled control erythroblasts cultured with EPO did not differ in appearance, except that the minor portion of more mature, benzidine-positive cells that had accumulated hemoglobin in the bcl-x-/- population had irregular, dense nuclei (Figure 4B). In the cultures of erythroblasts from bled control mice, a few reticulocytes and extruded nuclei were present (Rs and asterisk, respectively, in Figure 4A). The bcl-x-/- erythroblasts cultured for 20 hours without EPO (Figure 4C) differed significantly from the same cells cultured with EPO (Figure 4B) in that the benzidine-negative, early stage erythroblasts were all abnormal, apoptotic-appearing cells. Arrows in Figure 4C designate these immature benzidine-negative cells that have condensed, fragmented, apoptotic-appearing nuclei, whereas arrowheads designate examples of mature, benzidine-positive cells with an apoptotic appearance, similar to those bcl-x-/- erythroblasts cultured with EPO (Figure 4B). Thus, immature as well as mature erythroblasts from bcl-x-/- mice underwent apoptosis when cultured without EPO (Figure 4C). Figure 4D shows that at 32 hours some bcl-x-/- erythroblasts cultured with EPO still appeared normal and were beginning to synthesize hemoglobin despite an increasing number of apoptotic-appearing mature, benzidine-positive cells (arrowheads) and a few small, irregular-appearing reticulocytes (Rs). In Figure 4E, bcl-x-/- cells cultured with EPO for 44 hours were composed mostly of benzidine-positive, apoptotic erythroblasts with condensed and fragmented nuclei as well as a few small, irregular reticulocytes (Rs). In Figure 4F, erythroblasts from bled control mice at 44 hours with EPO had enucleated, forming normal-appearing reticulocytes (Rs) and extruded nuclei (asterisks).
Morphologic appearance of cultured bcl-x-/- and bled control erythroblasts. Cytospin preparations of erythroblasts harvested at various times were stained with 3,3′-dimethoxybenzidine and hematoxylin and examined by light microscopy. (A) Bled control erythroblasts cultured with EPO for 20 hours. (B) bcl-x-/- erythroblasts cultured with EPO for 20 hours. (C) bcl-x-/- erythroblasts cultured without EPO for 20 hours. (D) bcl-x-/- erythroblasts cultured with EPO for 32 hours. (E) bcl-x-/- erythroblasts cultured with EPO for 44 hours. (F) Bled control erythroblasts cultured with EPO for 44 hours. Arrowheads indicate examples of apoptotic, benzidine-positive, mature cells that have accumulated hemoglobin; arrows indicate examples of apoptotic, benzidine-negative, immature cells that have not accumulated hemoglobin; asterisks indicate examples of extruded nuclei; and R indicates an example of a reticulocyte. Original magnification, × 560.
Morphologic appearance of cultured bcl-x-/- and bled control erythroblasts. Cytospin preparations of erythroblasts harvested at various times were stained with 3,3′-dimethoxybenzidine and hematoxylin and examined by light microscopy. (A) Bled control erythroblasts cultured with EPO for 20 hours. (B) bcl-x-/- erythroblasts cultured with EPO for 20 hours. (C) bcl-x-/- erythroblasts cultured without EPO for 20 hours. (D) bcl-x-/- erythroblasts cultured with EPO for 32 hours. (E) bcl-x-/- erythroblasts cultured with EPO for 44 hours. (F) Bled control erythroblasts cultured with EPO for 44 hours. Arrowheads indicate examples of apoptotic, benzidine-positive, mature cells that have accumulated hemoglobin; arrows indicate examples of apoptotic, benzidine-negative, immature cells that have not accumulated hemoglobin; asterisks indicate examples of extruded nuclei; and R indicates an example of a reticulocyte. Original magnification, × 560.
bcl-x-/- erythroblasts synthesize heme
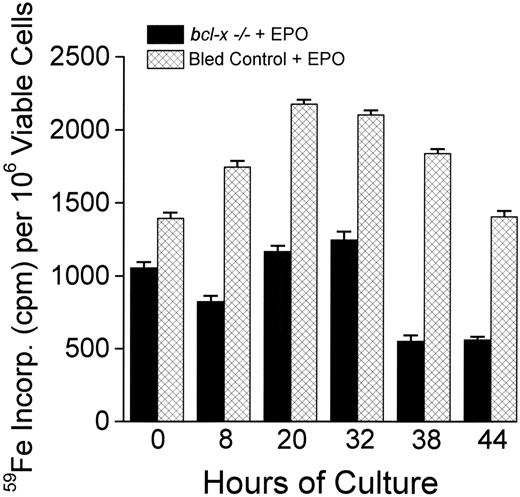
The photomicrographs in Figure 4 B-E show that bcl-x-/- cells synthesized hemoglobin, as shown by positive benzidine staining, but other reports have indicated that heme synthesis is impaired in the absence of Bcl-xL.15 We quantified heme synthesis by analyzing the incorporation of 59Fe into heme in erythroblasts cultured with EPO (Figure 5). The amount of 59Fe incorporated by cultured cells over 2-hour periods was measured at various times and expressed as counts per minute per 106 viable cells. Cells from bled control mice cultured with EPO had a peak in 59Fe incorporation from 20 to 32 hours of culture. The bcl-x-/-erythroblasts followed a similar pattern, but they had comparatively lower rates of 59Fe incorporation at all times. These results indicated that bcl-x-/- erythroblasts synthesize heme, but their ability to do so is reduced compared to erythroblasts from bled controls.
59Fe incorporation into heme by cultured erythroblasts from conditional bcl-x-/- mice and bled controls. At the indicated times, 59Fe-transferrin was added to quadruplicate cultures of erythroblasts from conditional bcl-x-/- mice or from bled control mice. After 2 hours of further incubation, incorporation of 59Fe into heme was quantified for each labeled culture and presented as counts per minute per 106 viable cells. Data are mean ± SEM of the quadruplicate cultures. The experiment shown is representative of 2 complete time-course experiments with 2 sets of erythroblast populations from conditional bcl-x-/- and bled control mice. For each of the 6 time points in the 2 independent experiments, the cells from bled controls incorporated significantly more 59Fe into heme per 106 viable cells than the bcl-x-/- erythroblasts.
59Fe incorporation into heme by cultured erythroblasts from conditional bcl-x-/- mice and bled controls. At the indicated times, 59Fe-transferrin was added to quadruplicate cultures of erythroblasts from conditional bcl-x-/- mice or from bled control mice. After 2 hours of further incubation, incorporation of 59Fe into heme was quantified for each labeled culture and presented as counts per minute per 106 viable cells. Data are mean ± SEM of the quadruplicate cultures. The experiment shown is representative of 2 complete time-course experiments with 2 sets of erythroblast populations from conditional bcl-x-/- and bled control mice. For each of the 6 time points in the 2 independent experiments, the cells from bled controls incorporated significantly more 59Fe into heme per 106 viable cells than the bcl-x-/- erythroblasts.
Discussion
Our results indicate that the major effect of Bcl-xL deficiency in vivo is ineffective erythropoiesis, rather than hemolytic anemia. As originally reported by Wagner et al,14 conditional bcl-x-/- mice are normal at birth, but they become progressively anemic as pubertal steroid hormones activate the conditional knockout of the bcl-x gene. Peripheral blood analyses revealed that the total number of reticulocytes was significantly lower in anemic conditional bcl-x-/- mice than in their normal littermate controls (Table 1). The extent of this reticulocytopenia was more evident when the conditional bcl-x-/- mice were compared to littermate controls that had been bled to make them anemic. In contrast, Wagner et al14 calculated that conditional bcl-x-/- mice had a 3-fold increase in the number of circulating reticulocytes when compared to normal littermates. Although genetically identical conditional bcl-x-/- mice were tested by Wagner et al14 and by us, one significant difference between their original study and that reported here is that they examined the mice at 3 months of age and we examined them at an average age that was 3 months older. The mice in our experiments reported here had greater splenomegaly and more severe anemia, indicating that they had a more severe phenotype when the peripheral blood was studied. The cultured erythroblasts from bcl-x-/- mice in our study exhibited no detectable Bcl-xL by Western blot analysis (Figure 2). Consistent with previous immunocytochemical results,14 the spleens of conditional bcl-x-/- mice had increases in the number of TER-119+ cells that were approximately 120-fold greater than normal controls and 18-fold greater than bled controls (Table 2). This massive erythroid hyperplasia would be expected to produce reticulocytes at even higher rates than found in our bled controls, which had a 5-fold increase in reticulocytes over unbled controls (Table 1). Thus, when the greatly increased numbers of erythroid progenitor cells in their spleens are considered, conditional bcl-x-/- mice had an extremely ineffective erythropoiesis.
Reticulocytes that were produced and released into circulation were further analyzed by the reticulocyte maturity index.19,20 The reticulocytes that were present in the blood of conditional bcl-x-/- mice were predominantly early reticulocytes, in contrast to the preponderance of late reticulocytes seen in the blood of the unbled littermate controls. The bled littermate controls, however, also showed a similar percentage of early reticulocytes as did the conditional bcl-x-/- mice. This shift to a majority of early stage reticulocytes is characteristic of severe erythropoietic stress. These increases in the proportions of immature reticulocytes in conditional bcl-x-/- mice and bled control mice contributed to the increased mean corpuscular volumes (MCVs) and red blood cell distribution widths (RDWs) in both groups, but the mature circulating erythrocytes of conditional bcl-x-/- mice were larger than those of unbled and bled controls (Table 1). Such macrocytosis and variability in size of mature erythrocytes is often found in ineffective erythropoiesis.
Conditional bcl-x-/- mice exhibited 12% apoptosis of nucleated TER-119+ cells, whereas bled controls exhibited 4% and unbled controls exhibited 2% (Table 2). In view of the very rapid removal of apoptotic cells in vivo,31 this increase in the percentage of apoptotic, nucleated TER-119+ cells in conditional bcl-x-/- mice provides a mechanism for ineffective erythropoiesis. Considering that nucleated splenic cells in conditional bcl-x-/- mice were 67% TER-119+ and 65% benzidine-positive (data not shown), the vastly increased numbers of benzidine-staining cells and the increased apoptosis in these spleens can also explain the hyperbilirubinemia. In most tissues, cells that undergo apoptosis become undetectable within 1 to 2 hours, mainly by rapid and efficient phagocytosis.31 In terms of splenic erythroblast turnover in mice with massive splenomegaly and ineffective erythropoiesis, splenic erythroblasts of mice with the acute erythroblastosis of Friend virus disease have been shown to have a daily turnover rate of 84%.32 Wagner et al described nuclear and nonnuclear cellular debris in extracellular areas of spleens from conditional bcl-x-/- mice,14 suggesting that some apoptotic erythroblasts may lyse prior to phagocytosis. Thus, in conditional bcl-x-/- mice, a steady state of 12% apoptotic TER-119+ cells that are rapidly removed by phagocytosis or lysis coupled with high proliferative rates (Figure 3) can result in complete turnover of a cohort of splenic erythroblasts in as little as 24 hours.
To examine in detail the differentiation and fate of bcl-x-/- erythroblasts, we explanted the erythroblasts and observed their differentiation in vitro. Our in vitro analyses showed that a large majority of erythroblasts undergo apoptosis at a late stage of maturation. The cumulative effects of apoptosis were most clearly evident in Figure 1B, in which viable cell numbers were 3 times greater at 32 hours and 10 times greater at 44 hours in EPO-treated cultures of bled control erythroblasts than in EPO-treated cultures of bcl-x-/- erythroblasts. Erythroblasts from bled controls survived, proliferated, and differentiated in culture, producing 2 reticulocytes at 44 hours per cell plated at 0 hours (Figure 1C). Conversely, splenic erythroblasts from conditional bcl-x-/- mice differentiated as shown by heme synthesis (Figure 5), benzidine positivity (Figure 4B,D-E), and progressive accumulation in the G0 phase that precedes enucleation (Figure 3), but apoptosis became predominant in the later erythroblast stages (Figure 4E) and only one reticulocyte was formed at 44 hours per 2 cells plated at 0 hours (Figure 1C). Similarly, conditional bcl-x-/- mice had decreased reticulocytes compared to controls (Table 1). Because Bcl-xL persists in immature reticulocytes,33 those reticulocytes that conditional bcl-x-/- mice are able to produce may undergo premature death, thereby contributing to the anemia of these mice through hemolysis. Determining the possible contribution of such hemolysis to the anemia would be difficult in the face of the extensive apoptosis of hemoglobin-containing erythroblasts, which elevated the serum indirect bilirubin (Table 1) and would increase serum levels of lactate dehydrogenase and decrease serum haptoglobin. Examination of blood smears, however, did not show any morphologic evidence of erythrocytic damage as might be expected with hemolysis due to an intrinsic erythrocyte defect.
The Bcl-xL-deficient cells underwent apoptosis proportionally in each phase of the cell cycle (Figure 3A-B). Normal murine erythroblasts that undergo apoptosis due to lack of EPO also do so in a cell cycle-independent manner.34 The predominance of apoptosis in late-stage bcl-x-/- erythroblasts is similar to ineffective erythropoiesis in megaloblastic anemias.35 However, in megaloblastic anemia, late-stage erythroblasts undergo apoptosis disproportionately in S phase rather than progressing through the cell cycle to the G0 phase that precedes enucleation.27 Folate deficiency and other causes of megaloblastic anemia impair DNA synthesis in erythroblasts, making these cells more vulnerable to apoptosis when they are in S phase. Bcl-xL, on the other hand, affects mitochondrial function, which is important in all stages of the cell cycle.
Although apoptosis of Bcl-xL-deficient erythroblasts cultured with EPO occurred at the stage of maximal hemoglobin synthesis, the cultured erythroblasts became benzidine positive (Figure 4B,D-E) and synthesized heme (Figure 5). The amount of heme synthesized per viable erythroblast, however, was less than in the littermate controls (Figure 5). Localization of Bcl-xL to the outer mitochondrial membrane suggests that it may play some role in heme synthesis because both early and late stages of heme production occur inside mitochondria.36 Minn et al7 characterized ion channels formed in the mitochondrial membrane by various Bcl-x mutants that do not cause apoptosis and postulated that Bcl-xL functions directly in the mitochondrial membrane by altering ion channels. Other important mitochondrial functions, such as oxidative respiration, could also be affected by Bcl-xL.
We compared bcl-x-/- erythroblasts cultured with and without EPO. If Bcl-xL were the primary mediator of the antiapoptotic effect of EPO in early stage erythroblasts, the majority of cells lacking Bcl-xL should die within the first 20 hours of culture with EPO, as has been shown previously with murine erythroblasts cultured without EPO.1 However, only 45% of bcl-x-/- erythroblasts cultured with EPO had undergone apoptosis at 20 hours (Figure 1A), whereas bcl-x-/- erythroblasts cultured without EPO exhibited 70% apoptosis at 20 hours (Figure 1A). As shown in Figure 4C, this increased apoptosis in bcl-x-/- erythroblasts cultured without EPO was due to the apoptosis of early stage cells prior to hemoglobin synthesis (ie, benzidine-negative cells). This antiapoptotic effect of EPO on early bcl-x-/- erythroblasts must be mediated through another antiapoptotic pathway that does not involve Bcl-xL. Our previous studies have shown that among other known antiapoptotic mediators Bcl-2 is not expressed in primary murine or human erythroblasts, A-1 is expressed early in murine differentiation, but not in an EPO-dependent manner, and Mcl-1 is expressed in an EPO-dependent manner in human erythroblasts and is a possible candidate for the antiapoptotic effect of EPO seen in bcl-x-/- erythroblasts.8 Conversely, the observed apoptosis in late-stage, hemoglobin-containing bcl-x-/- erythroblasts cultured with EPO (Figure 4B,D-E) is consistent with our previous studies demonstrating that the greatest accumulations of Bcl-xL occur in the late-stage, hemoglobin-synthesizing erythroblasts8 that are no longer dependent on EPO for survival.
Prepublished online as Blood First Edition Paper, May 17, 2005; DOI 10.1182/blood-2004-11-4344.
Supported by Merit Review Awards from the Department of Veterans Affairs (M.J.K. and M.C.B.) and National Institutes of Health grant T32 HL07751.
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.