Key Points
Peptidic C3 inhibitors of the compstatin family (Cp40) efficiently prevent hemolysis and opsonization of PNH erythrocytes in vitro.
Pharmacokinetic studies show that sustained therapeutic concentrations can be achieved with both Cp40 and its PEGylated derivative, PEG-Cp40.
Abstract
Paroxysmal nocturnal hemoglobinuria (PNH) is characterized by complement-mediated intravascular hemolysis due to the lack of CD55 and CD59 on affected erythrocytes. The anti-C5 antibody eculizumab has proven clinically effective, but uncontrolled C3 activation due to CD55 absence may result in opsonization of erythrocytes, possibly leading to clinically meaningful extravascular hemolysis. We investigated the effect of the peptidic C3 inhibitor, compstatin Cp40, and its long-acting form (polyethylene glycol [PEG]-Cp40) on hemolysis and opsonization of PNH erythrocytes in an established in vitro system. Both compounds demonstrated dose-dependent inhibition of hemolysis with IC50 ∼4 µM and full inhibition at 6 µM. Protective levels of either Cp40 or PEG-Cp40 also efficiently prevented deposition of C3 fragments on PNH erythrocytes. We further explored the potential of both inhibitors for systemic administration and performed pharmacokinetic evaluation in nonhuman primates. A single intravenous injection of PEG-Cp40 resulted in a prolonged elimination half-life of >5 days but may potentially affect the plasma levels of C3. Despite faster elimination kinetics, saturating inhibitor concentration could be reached with unmodified Cp40 through repetitive subcutaneous administration. In conclusion, peptide inhibitors of C3 activation effectively prevent hemolysis and C3 opsonization of PNH erythrocytes, and are excellent, and potentially cost-effective, candidates for further clinical investigation.
Introduction
Paroxysmal nocturnal hemoglobinuria (PNH) is a complex hematologic disorder characterized by the expansion of hematopoietic cells deficient in glycophosphatidylinositol-anchored surface proteins, including the complement regulators CD55 and CD59.1 Affected erythrocytes suffer from uncontrolled complement activation on their surface, and subsequent membrane attack complex (MAC)-mediated intravascular hemolysis.2 The therapeutic anti-C5 antibody eculizumab (Soliris, Alexion) has proven effective in controlling intravascular hemolysis in vivo, leading to remarkable clinical benefit in a majority of PNH patients.3,4 Yet, persistent C3 activation occurring during eculizumab treatment may lead to progressive deposition of C3 fragments on affected erythrocytes and subsequent C3-mediated extravascular hemolysis, possibly limiting the hematologic benefit of anti-C5 treatment.5,6 Thus, upstream inhibition of the complement cascade seems an appropriate strategy to improve the results of current complement-targeted treatment.7,8 Indeed, it has been recently documented that protein inhibitors of the alternative pathway (AP) of complement activation, such as the CD21/factor H (FH) fusion protein TT30 (Alexion) or the engineered complement regulator mini-FH, efficiently prevent both hemolysis and C3 deposition of PNH erythrocytes.9,10 Despite their high efficacy in vitro, the use of large proteins may potentially face challenges concerning pharmacokinetic properties and immunogenicity. Smaller inhibitors based on the compstatin family of peptidic, complement-targeted drugs may therefore offer an alternative option for the treatment of PNH.
Compstatin was originally discovered as a 13-residue cyclic peptide that selectively binds to human and nonhuman primate (NHP) forms of the central complement component C3 and its active fragment C3b.11 It thereby prevents the essential conversion of C3 to C3b and impairs all initiation, amplification, and terminal pathways of complement.12 Given their ability to block complement activation regardless of the initiation pathway, compstatin derivatives are considered promising candidate drugs for treating different complement-mediated diseases.13 One compstatin analog (originally termed 4[1MeW]; see supplemental Figure 1 on the Blood Web site for an overview of relevant analogs) has demonstrated beneficial results in phase 1 clinical trials for the treatment of age-related macular degeneration14 and is under clinical development by Potentia Pharmaceuticals. The same analog is being developed by Apellis Pharmaceuticals for other indications.13 Moreover, compstatin analogs showed promising results in various disease models ranging from hemodialysis to sepsis.12,15,16 In contrast to the local or time-restricted administration of compstatin in the above-mentioned clinical situations, therapeutic intervention in a chronic systemic disease such as PNH imposes higher demands on drug properties, particularly concerning pharmacokinetics. Over the past decade, optimization studies have been conducted to develop compstatin derivatives with improved characteristics for systemic use.17-19 The current lead analog Cp40 (clinically developed by Amyndas Pharmaceuticals)13 shows strong binding affinity for C3b (KD ∼0.5 nM) and a plasma half-life (t1/2 ∼12 hours) that exceeds typical peptide drugs.18 Despite these favorable properties, it is anticipated that a long-acting derivative of Cp40 based on site-specific addition of polyethylene glycol (PEG) moieties may benefit a sustained pharmacologic complement inhibition as needed in PNH.
By investigating the efficacy of Cp40 and its long-acting PEGylated derivatives regarding the protection of PNH erythrocytes in vitro and evaluating their pharmacokinetic properties in NHP, we describe a novel potential treatment option for PNH.
Methods
Human samples
Peripheral blood was collected from healthy volunteers (as a source for ABO-matched normal sera) and patients suffering from purely hemolytic PNH. For consistency, blood was serially drawn from the same 2 untreated patients who exhibited a large PNH cell population (>10% on erythrocytes, >50% on granulocytes) for all experiments. Additionally, serum was collected from a PNH patient on eculizumab just after dosing; this was used for testing the effect of anti-C5 on C3 fragment deposition in vitro. Blood was collected in standard EDTA and serum Vacutainer tubes (BD Pharmingen, Milan, Italy) after venipuncture according to standard procedures, following informed consent as approved by the local Institutional Review Board. This study was conducted in accordance with the Declaration of Helsinki.
Complement inhibitors
Cp40 (dTyr-Ile-[Cys-Val-Trp(Me)-Gln-Asp-Trp-Sar-Ala-His-Arg-Cys]-mIle-NH2; 1.7 kDa) was produced by solid-phase peptide synthesis as previously described.18 Two forms of long-acting Cp40 were prepared: for N-terminal PEGylation (PEG-Cp40), a Y-shaped PEG moiety with an average molecular weight of 40 kDa (Y-40K-NHS; JenKem Technology, Allen, TX) was added to the N-terminal amine of Cp40 via a N-hydroxysuccinimide group. The PEGylation reagent (120 mg/mL in acetonitrile/water 1:1) was mixed with Cp40 (5 mg/mL) and N-methylmorpholine (12 µL/mL), and the reaction mixture was rotated overnight at room temperature.20 Subsequently, the pH was adjusted to 2 to quench the reaction. For C-terminal PEGylation (Ac-Cp40-K-PEG), the N terminus of Cp40 was protected by acetylation and an extra lysine residue was added at its C terminus during peptide synthesis; the PEGylation reagent was coupled to the C-terminal lysine as described above. A linear, sequence-scrambled compstatin derivative (Sar-Sar-Trp(Me)-Ala-Ala-Asp-Ile-His-Val-Gln-Arg-mIle-Trp-Ala-NH2) was synthesized as an inactive control. All peptides were purified by reversed-phase high-performance liquid chromatography, characterized by mass spectrometry (MS), and tested for the absence of endotoxin (<0.03 EU/mL).
Evaluation of complement inhibition activity and C3 binding
The ability of compstatin analogs to inhibit complement activation was evaluated using an established enzyme-linked immunosorbent assay (ELISA)-based method, based on the detection of C3b deposition after activation of normal human serum (NHS) by immune complexes.17,18 Inhibitor concentrations of 0.01 µM to 10 µM were used.
The characterization of binding properties to C3 is described in supplemental “Methods.”
Assessment of PNH erythrocyte lysis and opsonization
Compstatin analogs were evaluated using an established in vitro system assessing both intravascular hemolysis and C3 fragment deposition (as a surrogate marker for C3-mediated extravascular hemolysis) on PNH erythrocytes.9 Erythrocytes were obtained from peripheral blood after three washings in saline, and subsequently incubated with Mg2+-supplemented sera from ABO-matched healthy individuals (NHS) at final hematocrits of 2%; to reduce interexperiment variability, pooled sera from at least 3 subjects (all with plasma C3 in the normal range) were used. AP activation was achieved by acidification using HCl (1:20 of HCl 0.1 N), which resulted in a pH drop to a value between 6.7 and 6.9. Cp40, its PEGylated derivatives, or an inactive control peptide were added to the tubes at different concentrations before complement activation. After a 24-hour incubation at 37°C in acidified NHS (AcNHS), hemolysis was quantified by flow cytometry after staining of the erythrocyte pellet with a fluorescein isothiocyanate-conjugated anti-C3 polyclonal antibody (Ab14396; Abcam, Cambridge, UK) and a PE-conjugated anti-CD59 monoclonal antibody (59-PE; Valter Occhiena, Torino, Italy), as previously described.9,21
The same anti-C3/anti-CD59 staining also served to assess opsonization by evaluating the deposition of C3 fragments on erythrocytes exposed to AP activation in the presence of C3 inhibitors using flow cytometry at the end of the hemolytic assay. The anti-C3 used in this study (Ab14396) has been shown to bind both C3b and its degradation fragments, iC3b and C3dg.9
Injection of compstatin derivatives in NHPs
Pharmacokinetic evaluation was performed at the Association for Assessment and Accreditation of Laboratory Animal Care International-accredited SICONBREC (Makati City, Philippines) in cynomolgus monkeys (Macaca fascicularis). For PEG-Cp40, 2 healthy animals were sedated and injected intravenously with 50 mg/kg of the compound (corresponding to ∼2 mg/kg of unmodified Cp40 when accounting for the >20-fold size difference) dissolved in saline for injection. Blood samples (1 to 2 mL) were collected immediately before and at various time points after compound injection (1 and 2 hours; 1, 2, 4, 7, 9, and 14 days) and mixed with EDTA to prevent coagulation. In addition, Cp40 was administered via subcutaneous injection. Initially, a single injection of 2 mg/kg Cp40 was administered to 2 animals and blood samples were collected before and after the injection (2, 5, and 30 minutes; 1, 2, 4, 6, and 24 hours). Based on the results of this single dose, a regimen of repetitive subcutaneous injections was developed: Cp40 (1 mg/kg) was injected in 2 animals every 12 hours (4 doses in total) and blood was collected at various time points (0.5, 4, 8, and 12 hours after each injection) as described above; and a final blood collection was performed after 72 hours (ie, 36 hours after the last injection). Blood samples were centrifuged at ∼800 × g for 10 minutes to obtain plasma, and immediately frozen until further analysis. All NHP studies were performed in accordance with animal welfare laws and regulations, as approved and enforced by the SICONBREC IACUC.
Monitoring of plasma levels of inhibitors and C3
Total inhibitor levels (C3-bound and free) were determined by extracting compstatin analogs from plasma samples using solid-phase extraction (SPE) and quantifying them by reversed-phase liquid chromatography coupled with MS, essentially as described before and in supplemental “Methods.”18
The baseline plasma level of C3 before the start of each experiment was determined using ELISA as previously described.18 In addition, western blotting was performed to monitor C3 levels during the course of treatment. Plasma samples at various time points of each treatment were diluted 10-fold in phosphate-buffered saline; 1 µL of each diluted sample was subjected to 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis under reducing conditions and transferred to nitrocellulose membranes before detection with a peroxidase-conjugated polyclonal goat antihuman C3 antibody (MP Biomedicals, Solon, OH). Plasma levels of transferrin, detected with a peroxidase-conjugated polyclonal rabbit antihuman transferrin antibody (Acris, San Diego, CA), were analyzed as an internal control after stripping the anti-C3 antibody.
Results
Design and activity of Cp40 and its PEGylated derivatives
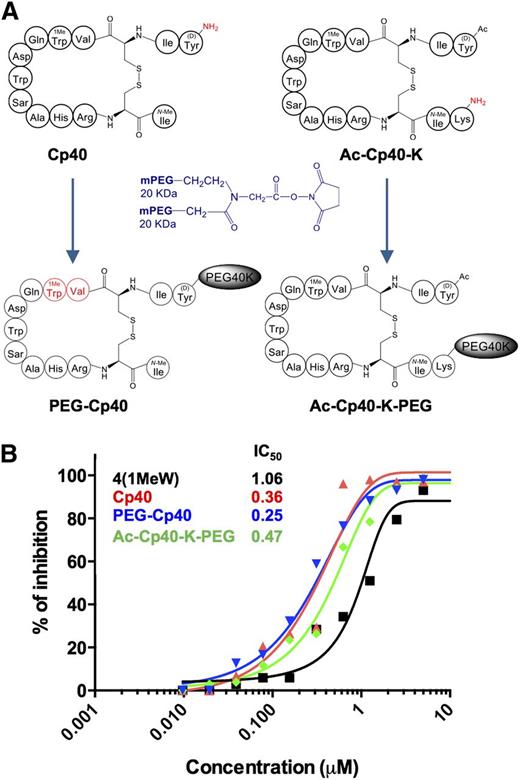
Although Cp40 exhibits favorable pharmacokinetic properties,18 we aimed to further increase the plasma residence of the inhibitor by adding a 40-kDa PEG moiety as a means of reducing renal filtration. The crystal structure of compstatin with a C3 fragment revealed that the terminal amino acids of this cyclic peptide are not essential for binding and may be modified.22 Derivatives of Cp40 were therefore prepared that contained PEG either directly linked to the N terminus (PEG-Cp40) or to the C terminus after introducing a lysine residue (Ac-Cp40-K-PEG) (Figure 1A). Characterization of the binding to C3 showed that both PEGylated analogs featured slower association rates, due to either an impact of the larger molecule on the diffusion rate or lower accessibility to the binding site of surface-bound C3; however, the complex stability (ie, dissociation rate constant) was similar to unmodified Cp40 (supplemental Figure 2). As the primary target for Cp40 is circulating C3, and PEGylated Cp40 derivatives are expected to remain above saturating concentrations for an extended time, the association rate is considered less important for overall activity of the inhibitors. Indeed, a comparison of the compstatin derivatives in a complement activation assay showed that the inhibitory activity of PEG-Cp40 was highly comparable to Cp40, with Ac-Cp40-K-PEG exhibiting a minor rise in IC50. Cp40 and its PEGylated forms were more potent than compstatin analog 4(1MeW), which features a lower degree of structural modification (Figure 1B and supplemental Figure 1).13,23
Preparation and characterization of compstatin Cp40 and long-acting derivatives thereof. (A) Schematic representation of the PEGylation strategy: PEG-Cp40 was prepared by adding a reactive two-arm branched PEG moiety of 40 kDa to the unprotected amino terminus of Cp40. In the case of Ac-Cp40-K-PEG, the N terminus was acetylated, a C-terminal lysine residue was added to the peptide during synthesis, and the PEG reagent was reacted with the lysine side chain. The dipeptide fragment used for the mass spectrometric quantification of PEG-Cp40 in plasma is indicated in red. (B) Evaluation of the complement inhibitory activity of Cp40 and its PEGylated derivatives using a complement activation ELISA. The clinically developed analog 4(1MeW)14 is shown as a control (for more information on individual compstatin analogs, see also supplemental Figure 1). The panel shows a representative plot out of 3 separate experiments.
Preparation and characterization of compstatin Cp40 and long-acting derivatives thereof. (A) Schematic representation of the PEGylation strategy: PEG-Cp40 was prepared by adding a reactive two-arm branched PEG moiety of 40 kDa to the unprotected amino terminus of Cp40. In the case of Ac-Cp40-K-PEG, the N terminus was acetylated, a C-terminal lysine residue was added to the peptide during synthesis, and the PEG reagent was reacted with the lysine side chain. The dipeptide fragment used for the mass spectrometric quantification of PEG-Cp40 in plasma is indicated in red. (B) Evaluation of the complement inhibitory activity of Cp40 and its PEGylated derivatives using a complement activation ELISA. The clinically developed analog 4(1MeW)14 is shown as a control (for more information on individual compstatin analogs, see also supplemental Figure 1). The panel shows a representative plot out of 3 separate experiments.
Effects of Cp40 and PEGylated derivatives on hemolysis and opsonization of PNH erythrocytes
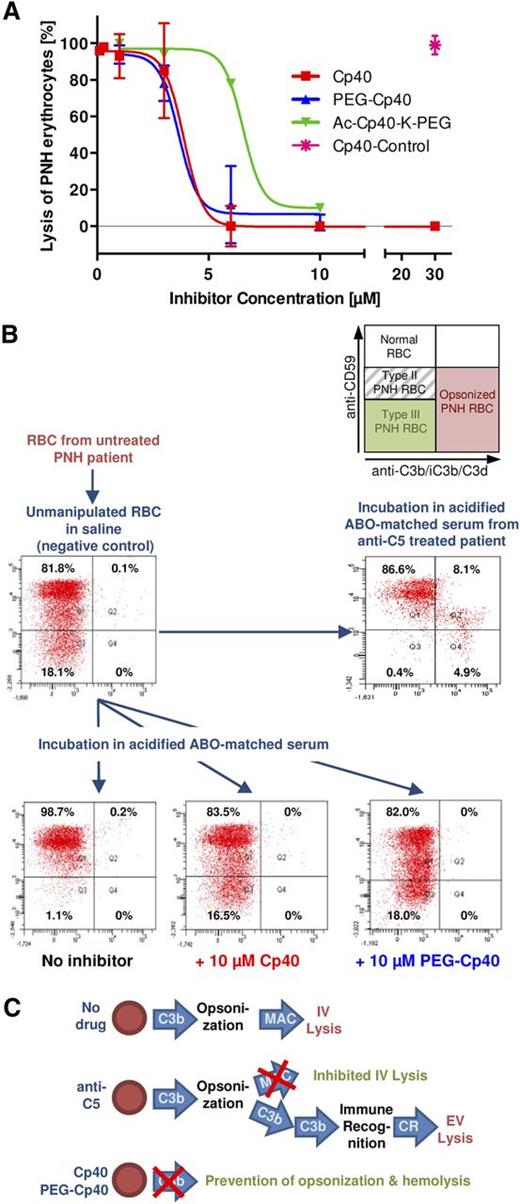
The activity of Cp40 and its long-acting derivatives for preventing intravascular hemolysis was tested in an established in vitro model using patient-derived erythrocytes.9,10 A total of 10 experiments were performed on erythrocytes obtained from 2 untreated PNH patients. Activation of the AP in the absence of inhibitors resulted in almost complete hemolysis of PNH erythrocytes (97 ± 3% after 24 hours). When added to NHS before acidification, Cp40 resulted in a concentration-dependent inhibition of hemolysis, with an IC50 of ∼4 µM and full inhibition at 6 µM (Figure 2A). A control peptide did not exert any effect on hemolysis (99 ± 1%) even at concentrations up to 30 µM. PEG-Cp40 resulted in a similar inhibitory potency (IC50 ∼4 µM; full inhibition ∼6 µM), whereas Ac-Cp40-K-PEG showed a reduced activity (IC50 ∼7 µM; full inhibition ∼10 µM; Figure 2A). Thus, inhibition of AP-mediated complement activation with compstatin analogs efficiently disabled MAC formation on CD55−/CD59− PNH erythrocytes. Due to the lower activity of Ac-Cp40-K-PEG in the complement activation assay and the hemolysis model, this derivative was not included in subsequent studies.
Effect of C3 inhibitors on hemolysis and C3 fragment deposition of PNH erythrocytes. (A) Dose-response curves from the in vitro hemolysis assay with Cp40 (red) and its long-acting derivatives PEG-Cp40 (blue) and Ac-Cp40-K-PEG (green). Lysis of PNH erythrocytes (y-axis) is expressed as a relative percentage of the lysis observed without any inhibitor (in each experiment, 100% represents the lysis observed in AcNHS) relative to the concentration of the C3 inhibitors (x-axis). Curves represent the mean of 10 experiments performed on samples obtained from 2 PNH patients; error bars represent standard deviations. (B) Flow cytometry assessment of C3 fragment deposition on the surface of erythrocytes from untreated PNH patients. Dot plots show intact erythrocytes as gated by physical parameters; CD59 (59-PE monoclonal Ab; y-axis) vs C3 fluorescein isothiocyanate (Ab14396 polyclonal Ab; x-axis). Scheme of erythrocyte populations and potential pattern of C3-fragment deposition on normal, type II, and type III PNH erythrocytes as observed in the fluorescence-activated cell sorter plots (top); unmanipulated fresh erythrocytes (negative control) and erythrocytes incubated in the presence of eculizumab (acidified ABO-matched serum from a patient on eculizumab, positive control for C3 deposition) (middle, from left to right); and erythrocyte pellets after incubation in acidified ABO-matched NHS in the absence of inhibitors (positive control for hemolysis) and in the presence of blocking concentrations of Cp40 and PEG-Cp40. Plots show representatives out of the 10 experiments (bottom, from left to right). (C) Schematic representation of activity spectrum of Cp40 in comparison with anti-C5 therapy. Eculizumab only blocks MAC formation and thus intravascular lysis, thereby enabling possible C3 opsonization of surviving erythrocytes and subsequent extravascular hemolysis. C3 inhibitors such as Cp40 prevent C3 activation upstream, thereby preventing both intravascular lysis and possible C3-mediated extravascular lysis via CR.
Effect of C3 inhibitors on hemolysis and C3 fragment deposition of PNH erythrocytes. (A) Dose-response curves from the in vitro hemolysis assay with Cp40 (red) and its long-acting derivatives PEG-Cp40 (blue) and Ac-Cp40-K-PEG (green). Lysis of PNH erythrocytes (y-axis) is expressed as a relative percentage of the lysis observed without any inhibitor (in each experiment, 100% represents the lysis observed in AcNHS) relative to the concentration of the C3 inhibitors (x-axis). Curves represent the mean of 10 experiments performed on samples obtained from 2 PNH patients; error bars represent standard deviations. (B) Flow cytometry assessment of C3 fragment deposition on the surface of erythrocytes from untreated PNH patients. Dot plots show intact erythrocytes as gated by physical parameters; CD59 (59-PE monoclonal Ab; y-axis) vs C3 fluorescein isothiocyanate (Ab14396 polyclonal Ab; x-axis). Scheme of erythrocyte populations and potential pattern of C3-fragment deposition on normal, type II, and type III PNH erythrocytes as observed in the fluorescence-activated cell sorter plots (top); unmanipulated fresh erythrocytes (negative control) and erythrocytes incubated in the presence of eculizumab (acidified ABO-matched serum from a patient on eculizumab, positive control for C3 deposition) (middle, from left to right); and erythrocyte pellets after incubation in acidified ABO-matched NHS in the absence of inhibitors (positive control for hemolysis) and in the presence of blocking concentrations of Cp40 and PEG-Cp40. Plots show representatives out of the 10 experiments (bottom, from left to right). (C) Schematic representation of activity spectrum of Cp40 in comparison with anti-C5 therapy. Eculizumab only blocks MAC formation and thus intravascular lysis, thereby enabling possible C3 opsonization of surviving erythrocytes and subsequent extravascular hemolysis. C3 inhibitors such as Cp40 prevent C3 activation upstream, thereby preventing both intravascular lysis and possible C3-mediated extravascular lysis via CR.
A major advantage targeting early complement activation (ie, at the level of C3) in PNH is the possible effect on continuous opsonization of PNH erythrocytes, which is thought to contribute to extravascular lysis.1,8 We tested the antiopsonic activities of Cp40 and PEG-Cp40 using the assay described above. Flow cytometric analysis of PNH erythrocytes after incubation in AcNHS confirmed the disappearance of type III PNH erythrocytes due to intravascular lysis in the absence of inhibitors (Figure 2B). However, in the presence of inhibitory concentrations of Cp40 and PEG-Cp40, this population remained intact. Importantly, no C3 fragment deposition was detectable on surviving erythrocytes when using a polyclonal antibody that reacts with opsonic C3 fragments (Figure 2B). This was in contrast to observations with anti-C5 treatment in the same in vitro assay (performed using serum from a patient just dosed with eculizumab; Figure 2B),24 and in vivo,9 which preserved the type III population but led to a marked increase in C3-derived opsonins on the surface of these erythrocytes. These data confirm that inhibition at the level of C3 activation counterbalances the lack of both CD55 and CD59 on PNH erythrocytes, thereby fully disarming the harmful activity of complement (Figure 2C).9
Pharmacokinetic profile of PEG-Cp40 in NHPs
The effect of PEGylation on the plasma half-life of Cp40 was assessed by pharmacokinetic profiling of PEG-Cp40 in NHP after a single intravenous injection (Figure 3A). Blood samples spanning a period of 2 weeks postinjection from 2 animals showed a reproducible pharmacokinetic profile with a slow terminal elimination phase and a t1/2 value of 5.5 days (Figure 3B). Inhibitor concentrations appeared to be independent on the individual baseline level of plasma C3 and, at the dosage used in this study, remained above target level for at least 1 week (Figure 3B). No signs of adverse effects were detected in either of the animals treated with PEG-Cp40. As C3 undergoes a turnover in plasma (through mechanisms that have not been fully elucidated),25-27 we investigated whether the strong binding of a PEGylated inhibitor at saturating concentrations may influence the plasma profile of C3. Since the PEG moiety caused interference with antibody-based methods for C3 quantitation (eg, ELISA; data not shown), western blot analysis was employed for semiquantitative analysis of C3 levels during the course of the experiment. Upon injection with PEG-Cp40, both animals showed bands for the C3 α- and β-chain growing in intensity and reaching peak levels between days 4 and 7 (Figure 3C), thereby suggesting slow accumulation of plasma C3 in the presence of PEG-Cp40. Hence, PEGylation creates a long-acting form of Cp40 with >10-fold increased plasma residence, but the administration of PEGylated compstatin may potentially affect the plasma profile of C3.
Pharmacokinetic evaluation of PEG-Cp40 in NHPs. (A) Dose scheme for PEG-Cp40 administration: a single dose of 200 mg PEG-Cp40 was injected intravenously into 2 cynomolgus monkeys at time 0 (green arrow) and blood samples were drawn at various time points (red arrows). Given the size difference between Cp40 (1.7 kDa) and PEG-Cp40 (∼40 kDa), the selected dose corresponds to ∼2 mg of active peptide per kg. (B) Monitoring of PEG-Cp40 plasma concentrations as determined by ultra performance liquid chromatography-high definition mass spectrometry (after fragmentation using subtilisin-A and SPE). Baseline levels of plasma C3 (measured by ELISA in T0 sample) are depicted as dotted lines for each animal. Note that the 1 and 2 hour postinjection blood draws were not included in this analysis. (C) Change of plasma C3 levels during the treatment with PEG-Cp40; western blot analysis after 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (reducing conditions) was performed with plasma samples collected at different time points and a polyclonal C3 antibody was used for detection (top). Although the antibody recognized both chains of C3, the reactivity with the α-chain was generally higher. Plasma levels of an unrelated protein (transferrin) were used as an internal control on the same membrane after stripping and reprobing with a transferrin antibody (bottom). Panel shows a representative blot from at least 2 independent analyses of samples from 2 animals each.
Pharmacokinetic evaluation of PEG-Cp40 in NHPs. (A) Dose scheme for PEG-Cp40 administration: a single dose of 200 mg PEG-Cp40 was injected intravenously into 2 cynomolgus monkeys at time 0 (green arrow) and blood samples were drawn at various time points (red arrows). Given the size difference between Cp40 (1.7 kDa) and PEG-Cp40 (∼40 kDa), the selected dose corresponds to ∼2 mg of active peptide per kg. (B) Monitoring of PEG-Cp40 plasma concentrations as determined by ultra performance liquid chromatography-high definition mass spectrometry (after fragmentation using subtilisin-A and SPE). Baseline levels of plasma C3 (measured by ELISA in T0 sample) are depicted as dotted lines for each animal. Note that the 1 and 2 hour postinjection blood draws were not included in this analysis. (C) Change of plasma C3 levels during the treatment with PEG-Cp40; western blot analysis after 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (reducing conditions) was performed with plasma samples collected at different time points and a polyclonal C3 antibody was used for detection (top). Although the antibody recognized both chains of C3, the reactivity with the α-chain was generally higher. Plasma levels of an unrelated protein (transferrin) were used as an internal control on the same membrane after stripping and reprobing with a transferrin antibody (bottom). Panel shows a representative blot from at least 2 independent analyses of samples from 2 animals each.
Subcutaneous injection of unmodified Cp40 as a multidose regimen
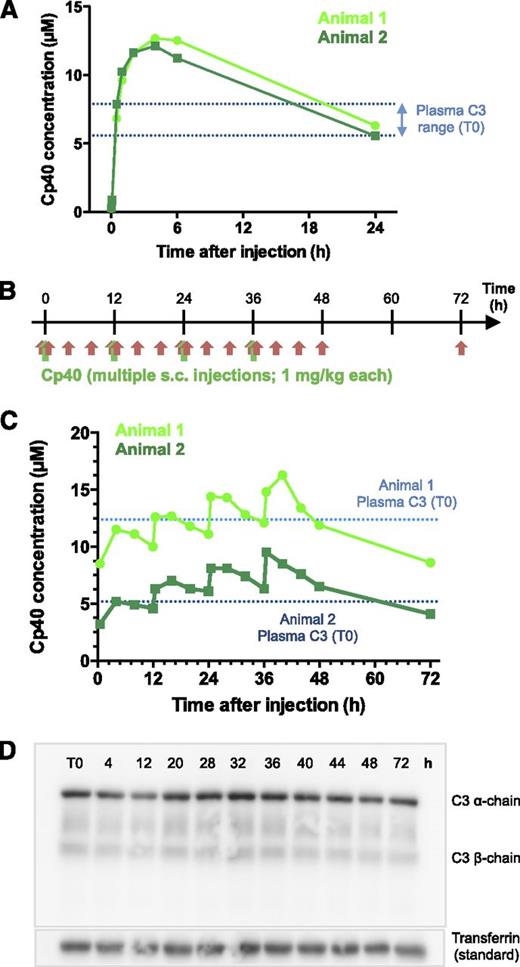
Although PEG-Cp40 exhibited enhanced plasma residence, unmodified Cp40 itself showed a beneficial pharmacokinetic profile with a half-life of 12 hours.18 Therefore, we evaluated the potential of subcutaneous injection of Cp40 as an alternative strategy for long-term systemic administration. A single subcutaneous injection of 2 mg/kg Cp40 resulted in an immediate increase in plasma inhibitor levels, with a peak at 4 hours and detectable Cp40 concentrations 24 hours postinjection (Figure 4A). In comparison with previous experiments with single intravenous injections,18 Cp40 reached a lower peak concentration but remained in excess of the C3 level for an extended period, likely due to continuous absorption from the subcutaneous depot. This pharmacokinetic profile suggested that saturating inhibitor levels may be reached with repetitive injections of Cp40 at the range of its half-life even at a lower dose. To verify this hypothesis, we employed a dosing schedule of 4 consecutive subcutaneous injections of 1 mg/kg at 12-hour intervals (Figure 4B). Analysis of Cp40 levels in plasma showed that each injection raised the inhibitor concentration within 0.5 to 4 hours, followed by a steady yet incomplete elimination (Figure 4C), hence closely resembling the profile of the single subcutaneous injection (Figure 4A). In contrast to the intravenous injection of PEG-Cp40 (Figure 3B), the plasma concentration of unmodified Cp40 in the subcutaneous regimen appeared to be influenced by the C3 level of the treated animal; importantly, saturating inhibitor concentrations could be reached within 2 to 3 injection cycles for both animals (Figure 4C). While a direct pharmacodynamic assessment of the Cp40 treatment was limited by the absence of an in vivo PNH model, and by the fact that plasma samples were collected in EDTA (which impairs direct use in complement functional assays), the assumption that antihemolytic activity can be maintained throughout the treatment period was supported by an in vitro model using plasma from one of the animals used in the subcutaneous treatment study (supplemental Figure 3). No adverse effects were observed in the animals, and no increase of C3 levels was detected during this multidose treatment (Figure 4D). Therefore, subcutaneous administration of Cp40 presents a valuable option for long-term systemic treatment of PNH and other complement-related diseases.
Subcutaneous administration of Cp40 in NHPs. (A) Pharmacokinetic profile of Cp40 in plasma samples collected 2, 5, and 30 minutes and 1, 2, 4, 6, and 24 hours after a single subcutaneous injection (2 mg/kg) in cynomolgus monkeys. Baseline levels of plasma C3 (measured by ELISA) are depicted as dotted lines for each animal. (B) Dose scheme for optimized Cp40 administration study: 4 doses of Cp40 (1 mg/kg each) were injected subcutaneously into 2 cynomolgus monkeys at a time interval of 12 hours (green arrows) and blood samples were collected 30 minutes, and 4, 8, and 12 hours after each injection, with an additional collection 72 hours after the start of the experiment (red arrows). (C) Monitoring of Cp40 plasma concentrations as determined by ultra performance liquid chromatography-high definition mass spectrometry (after SPE). Baseline levels of plasma C3 (measured by ELISA in T0 sample) are depicted as dotted lines for each animal. The dependence of the Cp40 concentration profiles on the baseline C3 level of each animal is expected to be caused by target-dependent elimination kinetics, as suggested in previous studies.18 (D) Plasma levels of C3 (top) and transferrin (internal standard; bottom) during the treatment with Cp40 as determined by western blot analysis (in analogy to Figure 3C). Panel shows a representative blot from at least 2 independent analyses of samples from 2 animals each.
Subcutaneous administration of Cp40 in NHPs. (A) Pharmacokinetic profile of Cp40 in plasma samples collected 2, 5, and 30 minutes and 1, 2, 4, 6, and 24 hours after a single subcutaneous injection (2 mg/kg) in cynomolgus monkeys. Baseline levels of plasma C3 (measured by ELISA) are depicted as dotted lines for each animal. (B) Dose scheme for optimized Cp40 administration study: 4 doses of Cp40 (1 mg/kg each) were injected subcutaneously into 2 cynomolgus monkeys at a time interval of 12 hours (green arrows) and blood samples were collected 30 minutes, and 4, 8, and 12 hours after each injection, with an additional collection 72 hours after the start of the experiment (red arrows). (C) Monitoring of Cp40 plasma concentrations as determined by ultra performance liquid chromatography-high definition mass spectrometry (after SPE). Baseline levels of plasma C3 (measured by ELISA in T0 sample) are depicted as dotted lines for each animal. The dependence of the Cp40 concentration profiles on the baseline C3 level of each animal is expected to be caused by target-dependent elimination kinetics, as suggested in previous studies.18 (D) Plasma levels of C3 (top) and transferrin (internal standard; bottom) during the treatment with Cp40 as determined by western blot analysis (in analogy to Figure 3C). Panel shows a representative blot from at least 2 independent analyses of samples from 2 animals each.
Discussion
Although eculizumab has dramatically improved the treatment of PNH,3,4,28 there are unmet clinical needs, as approximately one-third of PNH patients insufficiently respond to the drug and remain dependent on transfusions.3,4 Diverse factors may be responsible for the insufficient response to anti-C5 therapy. Bone marrow failure is the most obvious reason for a poor hematologic response, and this condition may require additional or alternative specific etiologic treatment (ie, either bone marrow transplantation or immunosuppression).29 “Breakthrough” intravascular hemolysis has been described in about 10% to 15% of PNH patients,30 potentially requiring increased dosages of eculizumab. Moreover, the deposition of C3 fragments on PNH erythrocytes has been observed in almost all PNH patients on eculizumab.5,6,31-33 This opsonization of PNH erythrocytes, and their subsequent recognition by complement receptors (CR) on phagocytic cells, results in extravascular hemolysis that is considered another, and likely the most important, cause for the insufficient response to eculizumab. Upstream complement inhibition at the level of C3 or the C3 convertase has therefore been considered a promising approach.8,13 Successful in vitro studies have been conducted with an antibody against C3b (mAb 3E7),34 the fusion protein TT30 that combines regulatory domains of FH with the iC3b/C3d-binding domains of CD21,9,35 and a novel engineered inhibitor that links the regulatory and surface recognition areas of FH (mini-FH).10 TT30 is currently being evaluated in a phase 1 clinical trial enrolling PNH patients.36 Although these inhibitors prevent both opsonization and hemolysis, their protein nature may unfavorably affect clinical development.13 In this study, we identify members of the compstatin family of C3 inhibitors as promising candidates for the development of improved treatment strategies for PNH. We demonstrate that Cp40 and its long-acting derivative PEG-Cp40 prevent both intravascular hemolysis and opsonization in vitro, while featuring distinct pharmacokinetic profiles that provide alternatives for tailoring treatment regimens. This proof-of-efficacy for upstream complement inhibition using small-size inhibitors marks an important step toward the development of comprehensive and cost-effective novel complement-targeted treatments.
Complement inhibition at the level of C3 faces specific challenges, since high plasma levels (∼0.7 to 1.5 mg/mL) and rapid turnover of this central component27 requires comparatively large inhibitor doses for achieving sustained target saturation in a stoichiometric fashion.13,27 In comparison with protein-based C3 inhibitors, Cp40 offers advantages concerning drug burden due to its small size (1.7 kDa); moreover, given its high plasma stability and its tight binding to circulating C3, Cp40 features a pharmacokinetic profile that is more favorable than that typically seen with peptidic drugs.18,37 Our study now indicates the clinical potential of Cp40, even in its nonmodified form, in diseases that require systemic long-term treatment. Due to the high bioavailability and sustained plasma profile after subcutaneous administration in NHP, therapeutic concentrations sufficient for sustained complement inhibition (supplemental Figure 3) could be achieved after repetitive injections at a comparatively low dose of 1 mg/kg. This anticipates a regimen of twice-daily (or even daily) injection, potentially allowing for patient self-administration as it is currently evaluated for other complement-targeted drugs.36,38 A subcutaneous regimen based on our preclinical data would translate to a daily dose of 140 mg of unmodified Cp40 for a 70 kg patient. Given the recent improvements in peptide production, the cost of which can drop below $1 per amino acid per gram during scale-up,37 compstatin may likely be more cost-effective in comparison with current eculizumab treatment or other protein-based complement inhibition.
Despite these advantages, long-term inhibition of plasma C3 may benefit from measures that prolong the half-life of Cp40 in a target-independent manner, and lead us to investigate PEGylation strategies that are commonly applied to therapeutic proteins and peptides.39-41 PEGylation at the N terminus of Cp40 appears particularly attractive, as it can be performed without intermediate steps (such as acetylation and the addition of lysine residues required for Ac-Cp40-K-PEG) and minimally affects the inhibitory efficacy. With a >10-fold increase in plasma residence, the addition of a 40-kDa PEG group improved the pharmacokinetic properties to a range that is closer to eculizumab and other therapeutic antibodies,42,43 possibly allowing dosage intervals of 1 to 2 weeks. This enhancement of half-life can be attributed to reduced glomerular filtration of the large PEGylated compound, primarily in the free circulating form, when compared with the ∼20-fold smaller parent peptide. In agreement with this hypothesis, and in contrast to unmodified Cp40, the plasma concentrations of PEG-Cp40 were largely independent of the baseline C3 level of the treated animal, thereby suggesting a slow, target-independent initial elimination. While no adverse reactions to PEG-Cp40 were observed in the treated animals during the time frame of the pharmacokinetic study, the detected accumulation of plasma C3 was unanticipated. The metabolic turnover of C3 is described to be more rapid and complex compared with other plasma proteins, and may involve clearance via activation (through the so-called tick-over mechanism), degradation, and uptake of fragments through cellular CR.27 Our data suggest that PEG-Cp40 may result in a reduced turnover of C3 that circulates in a stable complex with this 40-kDa inhibitor, whereas at least within the 3-day treatment period, no comparable accumulation of C3 was observed after injection of unmodified Cp40. Although the consequences of this accumulation may be marginal in vivo if the inhibitor stays in excess of C3, the impact of this finding on therapeutic efficacy, the potential need of dose escalation, and possible rebound effects warrants further investigation. Furthermore, although generally considered safe, PEGylation may change the immunogenicity and safety profiles of peptide/protein drugs, and cases of anti-PEG antibodies or vacuolation have been described.39,40 Finally, PEGylation causes a profound increase in production cost compared with the parent peptide, which, however, may be at least partially offset by reduced dosage intervals. 44
Whereas PNH is primarily driven by AP activation, many aspects concerning initiation and exacerbation of the erythrocyte-directed complement attack are not yet elucidated; contributions of the classical and/or lectin pathways cannot be excluded, especially at times of infection and subsequent hemolytic crises. Indeed, clinical observations suggest that massive complement activation during infections may overpower terminal complement inhibition as delivered by eculizumab (A.M.R. and R.N., personal communication),30 resulting in intravascular hemolysis due to “pharmacodynamic breakthrough” that likely results from an excess in C3 and C5 convertase, which may cleave free C5 that becomes transiently available from the C5:anti-C5 complex. Given that it is unclear which complement pathway is dominant during these paroxysms, compstatin analogs would offer an advantage not only over C5-targeted inhibition but also over pathway-specific C3 convertase inhibitors and ensure maximum efficacy for preventing hemolysis in all circumstances. On the other hand, concerns have been raised about chronic impairment of C3 activation, particularly regarding increased susceptibility for infections and immune-complex–mediated diseases. Although such conditions have been described for subjects with inherited C3 deficiency, there is no consistent clinical phenotype.13,45,46 Moreover, previous studies reported that low residual levels of C3 are sufficient for microbial defense,47,48 and even complete C3 inhibition leaves some opsonic functions intact (eg, via C4b and pattern recognition molecules of the classical/lectin pathway). To date, preclinical and clinical evaluation of complement inhibitors have resulted in favorable safety profiles.13 Severe infection has not emerged as a frequent complication in PNH patients receiving eculizumab,30 though Neisseria meningiditis infection remains a rare but potentially life-threatening event requiring a specific vaccination program. Consistently, anti-meningococcal vaccination was also invoked in the clinical trials of the AP-specific inhibitor TT30,36 and will have to be considered (possibly combined with prophylactic antimicrobial therapy) in future clinical trials with compstatin analogs or other C3 inhibitors. In this safety perspective, given that the in vivo effects of long-term broad C3 inhibition are not known, repetitive subcutaneous injections of unmodified Cp40 should be favored over PEG-Cp40, since the drug could be phased out more efficiently, if needed. It will be only through extended clinical investigations that potential risks and clinical benefits entailed by each strategy of complement-targeted modulation in PNH can be established to select ideal candidate agents for clinical development. Due to their comparatively small size and peptidic nature, compstatin analogs have the advantage of substantially lower production costs,37 making them very appealing when seeking an affordable treatment option that is accessible to the majority of PNH patients worldwide.
In conclusion, we demonstrate that two members of the compstatin family (ie, Cp40 and its PEGylated derivative), efficiently prevent C3 activation and opsonization on PNH erythrocytes in vitro, which predicts the inhibition of both MAC-mediated intravascular and C3-mediated extravascular hemolysis in vivo. PEGylation of compstatin appears to be an intriguing strategy to reach long-term C3 inhibition in systemic complement-related diseases due to its enhanced plasma residence and high efficacy, but additional studies will be needed to evaluate its effects on plasma C3 profiles and suitable dose regimens. Meanwhile, subcutaneous injection of Cp40 offers an attractive alternative for immediate translational plans of systemic administration with distinct therapeutic advantages. Thus, this family of peptidic C3 inhibitors represents a novel class of complement therapeutics that is moving forward to clinical translation in PNH and other complement-mediated diseases.
The online version of this article contains a data supplement.
There is an Inside Blood commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Lucio Luzzatto for critical discussion of the data, Dr Yingxue Li for his help with the purification of compstatin analogs, and Dr Malvina Papanastasiou for her support with validating the MS results.
This work was supported by National Institutes of Health grants AI068730, AI030040, AI097805 (National Institute for Allergy and Infectious Diseases), EY020633 (National Eye Institute), and GM094447 (National Institute of General Medical Sciences) (J.D.L. and/or D.R.), a grant from the European Commission (FP7-DIREKT 602699) (J.D.L.), and a pilot grant from the Penn-CHOP Blood Center for Patient Care and Discovery (D.R.).
Authorship
Contribution: A.M.R., D.R., and J.D.L. conceived the study; A.M.R. performed the experimental work in the PNH studies with the help of P.R., C.P., M.R., R.N., and M.S.; E.S.R., Y.H., Z.L., and H.C. prepared compounds and performed the biochemical and pharmacokinetic studies with the help of F.L., R.A.D., and R.R.G.R.; A.M.R., D.R., L.D.V., F.P., R.N., D.R., and J.D.L contributed to the interpretation and discussion of the data; the manuscript was written by A.M.R., D.R., R.N., and J.D.L.; and all the authors critically revised the manuscript and contributed to the preparation in its final version.
Conflict-of-interest disclosure: D.R. and J.D.L. are the inventors of patents and/or patent applications that describe the use of complement inhibitors for therapeutic purposes. J.D.L. is the founder of Amyndas Pharmaceuticals, which is developing complement inhibitors for clinical applications. The remaining authors declare no competing financial interests.
Correspondence: Antonio M. Risitano, Hematology, Department of Clinical Medicine and Surgery, Federico II University of Naples, Via Pansini 5, 80131 Naples, Italy; e-mail: amrisita@unina.it; and Daniel Ricklin, Department of Pathology and Laboratory Medicine, University of Pennsylvania, 422 Curie Blvd, Philadelphia, PA 19104; e-mail: ricklin@upenn.edu.
References
Author notes
A.M.R. and D.R. contributed equally to this study.