Abstract
Thrombotic thrombocytopenic purpura (TTP) is the prototypical microangiopathy characterized by disseminated microthromboses, hemolytic anemia, and ultimately organ dysfunction. A link with deficiency of the von Willebrand factor–cleaving protease (ADAMTS13) has been demonstrated, but additional genetic and/or environmental triggers are thought to be required to incite acute illness. Here we report that 4 days of ADAMTS13 functional inhibition is sufficient to induce TTP in the baboon (Papio ursinus), in the absence of inciting triggers because injections with an inhibitory monoclonal antibody (mAb) consistently (n = 6) induced severe thrombocytopenia (< 12 × 109/L), microangiopathic hemolytic anemia, and a rapid rise in serum lactate dehydrogenase. Immunohistochemical staining revealed the characteristic disseminated platelet- and von Willebrand factor–rich thrombi in kidney, heart, brain, and spleen but not lungs. Prolonged inhibition (14 days, n = 1) caused myocardial ischemic damage and asplenia but not death. Control animals (n = 5) receiving equal doses of a noninhibitory anti-ADAMTS13 mAb remained unaffected. Our results provide evidence for a direct link between TTP and ADAMTS13 inhibition and for a mild disease onset. Furthermore, we present a reliable animal model of this disease as an opportunity for the development and validation of novel treatment strategies.
Introduction
von Willebrand factor (VWF) is a multimeric glycoprotein that bridges platelets to injured arterial vessels through interactions with both subendothelial collagen and platelet membrane receptors. Unusually large VWF multimers (UL-VWFs) are released as VWF precursors into the bloodstream by stimulated endothelial cells.1 These high-molecular-weight proteins are abnormally adhesive, being able to bind and cross-link platelets in circulation even in the absence of endothelial injury.2 Normally, UL-VWFs are rapidly cleaved by circulating VWF-cleaving protease (ADAMTS13),3 which generates VWF multimers of sizes seen in normal plasma.4 The inability to process UL-VWF in cases of ADAMTS13 deficiency can cause disseminated platelet-rich thrombi, which block terminal arterioles,1,5 leading to hemolytic anemia with ischemic organ failure and ultimately death in patients with thrombotic thrombocytopenic purpura (TTP). Diagnosis is based on signs of concurrent thrombocytopenia with hemolytic anemia and fragmented red blood cells (schistocytes) in the absence of other identifiable primary causes.6
ADAMTS13 deficiency can be hereditary by mutations in the ADAMTS13 gene3 or acquired by inhibiting autoantibodies to ADAMTS13.7 The former is currently treated by infusion of fresh frozen plasma, which contains donor ADAMTS13 to overcome the deficiency. The latter often requires plasma exchange to both replenish the diminished proteolytic activity and remove inhibitors. These plasma therapies could effectively reduce mortality to approximately 20%,8 but morbidity still is considerable and not seldom as a consequence of the plasma therapy.9,10 Safer therapeutic strategies are therefore required11 and could focus on the inhibition of the platelet-VWF interaction12 or on the reconstitution of enzyme by infusion of a recombinant ADAMTS13 preparation.13 However, the current Adamts13−/− mouse model does not consistently present with TTP features,14,15 hampering preclinical evaluation of novel potential therapeutic approaches.
Motto et al have indeed demonstrated that TTP can be triggered by injection of Escherichia coli derived shigatoxin in a subset of Adamts13−/− mice provided the “susceptible” genetic background CASA/Rk.15 The authors concluded that unidentified genetic and environmental modifiers contribute significantly to the development of acute disease. This was strengthened by the variable onset of TTP in the CASA/Rk Adamts13−/− animals (ie, although a small number of mice spontaneously developed TTP symptoms, others did not present with TTP even after stimulation with shigatoxin).
In humans, triggers are not always distinctively identifiable, although some observations on pregnancy,16,17 infection,18 and surgery19 as precipitating factors of acute illness in the background of ADAMTS13 deficiency have been reported. On the other hand, some patients with congenital ADAMTS13 deficiency present with recurrent TTP from childhood on,20 without reports of a trigger (eg, proband C and proband D in Matsumoto et al21 and patient 05 I-1 in Schneppenheim et al22 ), so-called Upshaw-Schulman syndrome (MIM #274150). Hence, identification and classification as well as pathophysiologic explanation of the exact role and mechanism of triggers remain obscure.
In this work, we have examined the effect of ADAMTS13 inhibition on primate hematophysiology in vivo to determine whether additional triggers would be required to provoke TTP and to develop a reliable animal model for this disease.
Methods
mAb characterization
Hybridomas were generated23 from mice primed with 10 μg purified human recombinant (full-length) ADAMTS13 (rADAMTS13), and monoclonal antibodies (mAbs) were produced on large scale in a bio-incubator (Celline CL 350, Integra Biosciences). The proteins were purified using protein A coupled Sepharose FF (GE Healthcare), dialyzed to phosphate-buffered saline, pH 7.4. All preparations were controlled for purity by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and Coomassie staining, for inhibitory activity against baboon plasma ADAMTS13 by FRETS-VWF73 assay and for endotoxin content using the LAL precipitation assay following instructions from the provider (Lonza Switzerland).
Two mAbs were selected for further study: 3H9 as an inhibitor to ADAMTS13 and 5C11 as a noninhibiting control. Measurement of ADAMTS13 activity in the presence of various concentration of either mAb was with 2μM FRETS-VWF73 and baboon plasma as a source of ADAMTS13 at 3% (vol/vol) as described.24 Reactions contained Pefabloc SC (Roche Diagnostics) to inhibit serine proteases. Animals injected with the ADAMTS13 inhibitor 3H9 are in the so-called “subject” group, and animals injected with control 5C11 are in the “control” group.
Binding of rADAMTS13 to 5C11 and 3H9 was assessed by enzyme-linked immunosorbent assay (ELISA). mAbs were immobilized onto an 96-well plate followed by incubation with serial dilutions of rADAMTS13. Detection of bound enzyme was with horseradish peroxidase-labeled anti-V5 (anti-V5–HRP; Invitrogen) and o-phenylendiamine as chromogenic substrate. All rADAMTS13 proteins contain a V5 epitope fused to the C-terminus. Apparent dissociation constants were calculated by iterative fitting to the quadratic binding equation using Prism Version 5 software (GraphPad).
3H9 and 5C11 epitopes were mapped to rADAMTS13 metalloprotease domain and a rADAMTS13 mutant lacking the second thrombospondin-1 repeat, respectively, using immunoprecipitation. Hereto, 10nM of recombinant protein was mixed with 5nM of mAb. Recombinant protein A coupled to Sepharose beads was used to precipitate the complexes by centrifugation. Bound domains were visualized by sodium dodecyl sulfate–polyacrylamide gel electrophoresis followed by Western blotting with anti-V5–HRP and chemiluminescence.
Baboon treatment, injections, and sampling
Housing, treatment, phlebotomy, and care for the Cape baboons (Papio ursinus) as well as the final protocol were approved by the Control Committee on Animal Experimentation of the University of the Free State (Bloemfontein, South Africa) in accordance with the National Code for Animal Use in Research, Education, Diagnosis and Testing of Drugs and Related Substances in South Africa before engaging any experimentation. All animals were male, weighed between 10 and 20 kg, and were disease-free for at least 6 months. Animals were anesthetized by intramuscular delivery of 10 mg/kg ketamine hydrochloride. Injections and blood sampling were performed by venipuncture of the femoral vein while under anesthesia. All antibody injections were at 600 μg/kg in physiologic phosphate buffer.
Blood analysis
All common blood parameters were determined blindly by automated and standardized methods in the Tertiary National Health Laboratory Service, Universitas Hospital, Bloemfontein, South Africa.
Schistocytes were counted by an expert hematologist not involved in this study. Samples were blinded, and counting was done manually. When less than 1% schistocytes were observed, the smear was considered normal.
ADAMTS13 antigen was measured by ELISA as described25 using normal human pooled plasma (n = 20) as a reference set at 100%. The concentration of murine mAbs in baboon plasma was determined by a sandwich ELISA as previously described.26 Residual ADAMTS13 activity in baboon plasma was determined by FRETS-VWF73 as described27 with modifications.24 ADAMTS13 activity at baseline (before mAb injection) was taken as a standard set to 100%. To control for antibody-antigen dissociation as a consequence of diluting the samples, measurements were carried out at room temperature, and the initial velocity (first 20 minutes) was measured every 30 seconds. Effects of antibody-antigen dissociation were, however, never observed as both antibodies have a small koff.
Tissue preparation and analysis
Animals were killed by intravenous injection of 200 mg/kg pentobarbitone (Euthapent, Kyron Laboratories) immediately followed by dissection and macroscopic inspection of lung, liver, heart, brain, kidney, and spleen. Wedges of lung, heart, brain, kidney, and spleen were dissected and fixed in 10% buffered formaldehyde for 24 hours. Liver sections were not included for microscopic analysis. A Tissue Tek mictrotome/cryostat device (Bayer Healthcare) was used for processing and embedding. Hematoxylin and eosin staining was by standard techniques. Staining for VWF and platelets was with a polyclonal anti-VWF (P0226) and the mAb antihuman glycoprotein IIIa clone Y2/51 (M0753), respectively, both peroxidase labeled (Dako Denmark). 3-3′-Diaminobenzidine was used as a chromogenic substrate. The Martius Scarlet Blue (MSB) technique was used for staining fibrin. This stain colors erythrocytes yellow, connective tissue blue, nuclei black to violet, and muscle and fibrin red. We used an Olympus BX41 microscope with a 100×/1.25 numeric aperture oil immersion objective. Digital image acquisition was with a Colorview IIIu camera and analySIS LS Report software (Version 2.6).
Statistics
Significance between datasets was assessed by the Student t test or the Mann-Whitney U test depending on the result of the Kolmogorov-Smirnov test for normality. Welch correction to the Student t test was performed if parametric datasets were found not to have equal variances by F test (Prism Version 5, GraphPad). P values were calculated comparing mean values of 3H9 with 5C11-injected animals using .05 as a cutoff for significance.
Results
3H9 is an inhibitory anti-ADAMTS13 monoclonal antibody
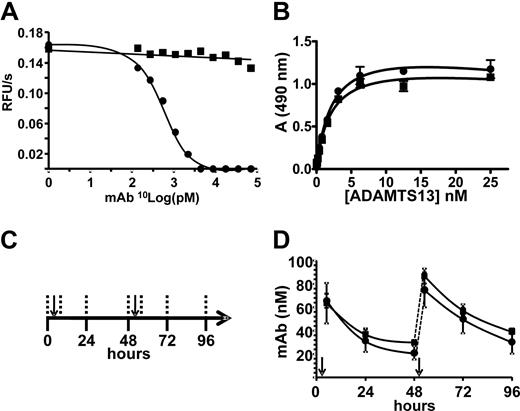
A series of mAbs was developed using purified full-length human rADAMTS13 as an antigen in Balb/c mice. The anti-ADAMTS13 mAb 3H9 binds an epitope in the metalloprotease domain of ADAMTS13 (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). 3H9 inhibits human ADAMTS13 function (not shown) and cross-inhibits ADAMTS13 in baboon plasma (Figure 1A). The noninhibitory anti-ADAMTS13 mAb 5C1128 binds to the second thrombospondin type 1 repeat (supplemental Figure 2) and serves as a control. Both mAbs have comparable affinity for rADAMTS13 with apparent dissociation constants of 2.4 ± 0.4nM and 2.2 ± 0.4nM (mean ± SD; n = 3) for 3H9 and 5C11, respectively (Figure 1B).
3H9 inhibits baboon ADAMTS13. (A) Enzyme activity was measured using FRETS-VWF73 as a substrate and baboon plasma as a source of ADAMTS13 in the presence of increasing concentrations of either 3H9 (●) or 5C11 (■). Change in fluorescence in function of time is shown in function of the mAb concentration. (B) Binding of rADAMTS13 to immobilized 3H9 (●) and 5C11 (■) is shown as an increase in absorbance (A, 490 nm) in function of free rADAMTS13 concentration (n = 3). Nonlinear regression to the quadratic binding equation was performed (solid line). Error bars represent SD. (C) Baboons were injected with boluses of 600 μg/kg of mAb at the time points indicated by the arrow. Blood was sampled at the time points indicated by the vertical dashed lines. (D) Concentration of mAb was determined ex vivo in citrated plasma samples from subject (●, n = 6) and control baboons (■, n = 5) and expressed as mean ± SD in function of time. The dashed lines indicate the rise in murine immunoglobulin titer after the second injection. Arrows indicate moments of injection.
3H9 inhibits baboon ADAMTS13. (A) Enzyme activity was measured using FRETS-VWF73 as a substrate and baboon plasma as a source of ADAMTS13 in the presence of increasing concentrations of either 3H9 (●) or 5C11 (■). Change in fluorescence in function of time is shown in function of the mAb concentration. (B) Binding of rADAMTS13 to immobilized 3H9 (●) and 5C11 (■) is shown as an increase in absorbance (A, 490 nm) in function of free rADAMTS13 concentration (n = 3). Nonlinear regression to the quadratic binding equation was performed (solid line). Error bars represent SD. (C) Baboons were injected with boluses of 600 μg/kg of mAb at the time points indicated by the arrow. Blood was sampled at the time points indicated by the vertical dashed lines. (D) Concentration of mAb was determined ex vivo in citrated plasma samples from subject (●, n = 6) and control baboons (■, n = 5) and expressed as mean ± SD in function of time. The dashed lines indicate the rise in murine immunoglobulin titer after the second injection. Arrows indicate moments of injection.
Systemic inhibition of ADAMTS13 in baboons injected with 3H9
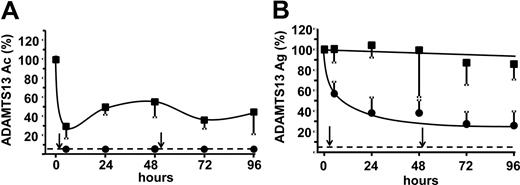
Two boluses of 600 μg/kg 3H9 and 5C11 were administered intravenously to 6 and 5 baboons, respectively, over the course of 2 days with a 96-hour follow-up regimen (Figure 1C). Antibody injections resulted in a mean initial plasma mAb concentration of more than 50nM, which declined similarly for both mAbs (Figure 1D). Consequently, plasma ADAMTS13 activity fell below detection limit (< 5%, Figure 2A), and antigen decreased to approximately 40% in subject animals (Figure 2B). ADAMTS13 activity was reduced to approximately 50% in control animals despite normal antigen levels and no measurable functional inhibition in vitro (Figures 1–2). Neither VWF antigen (supplemental Figure 3) nor multimer patterns (supplemental Figure 4) changed significantly over the course of the study in either group.
ADAMTS13 is inhibited and partially cleared in baboons injected with 3H9. (A) The residual mean ADAMTS13 activity (Ac) and (B) antigen (Ag) levels were measured in citrated plasma from subject (●, n = 6) or control baboons (■, n = 5) relative to baseline (0 hours) and are shown in function of time. Error bars represent SD, and dashed horizontal lines indicate the lower detection limit of the performed assay. Arrows indicate moments of injection.
ADAMTS13 is inhibited and partially cleared in baboons injected with 3H9. (A) The residual mean ADAMTS13 activity (Ac) and (B) antigen (Ag) levels were measured in citrated plasma from subject (●, n = 6) or control baboons (■, n = 5) relative to baseline (0 hours) and are shown in function of time. Error bars represent SD, and dashed horizontal lines indicate the lower detection limit of the performed assay. Arrows indicate moments of injection.
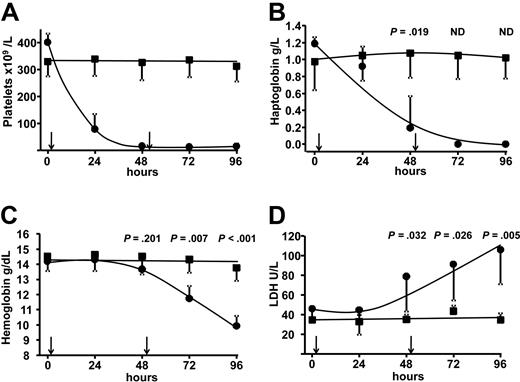
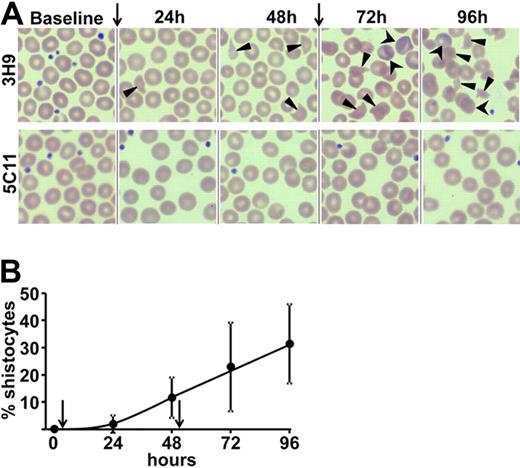
Inhibition of ADAMTS13 consistently causes thrombocytopenia and schistocytic hemolytic anemia
All subject animals developed thrombocytopenia within 24 hours, with platelet counts decreasing further to 12 ± 7 × 109/L after 48 hours (Figure 3A). As a consequence, some animals had minor bleeding events, which spontaneously resolved (supplemental Figure 5). Intravascular hemolysis became apparent as haptoglobin decreased to below the detection limit of the assay 72 hours after injection (Figure 3B) coinciding with a decrease in hemoglobin less than 70% of baseline (Figure 3C). Schistocytes were observed in peripheral blood smears, confirming the presence of fragmentation hemolysis (Figure 4A). The schistocyte count increased over time (Figure 4B), indicating that fragmentation was taking place continuously. Serum lactate dehydrogenase (LDH) levels, as a marker for tissue damage29 and hemolysis, increased approximately 3-fold (Figure 3D) with no signs of intravascular coagulation (supplemental Table 1). None of the animals had signs of renal failure as evidenced by normal urea and creatinine levels (supplemental Table 2). One baboon had signs of myocardial ischemia by elevated serum troponin-T at 72 hours (0.08 μg/L) and 96 hours (0.26 μg/L). All animals behaved normally throughout the study with no noticeable signs of discomfort as evaluated by expert caretakers. Control animals had normal platelet counts, no bleeding (not shown), no evidence of intravascular hemolysis, no elevated LDH (Figure 3), and no schistocyte formation (Figure 4A).
Hematologic parameters indicate acute thrombocytopenia and intravascular hemolysis after inhibition of ADAMTS13. (A-D) Hematologic parameters were determined in blood samples from subject (●, n = 6) or control animals (■, n = 5), and mean values ± SD are shown. (A) Subject animals were thrombocytopenic from 24 hours onwards, dropping further to less than 12 × 109/L at 48 hours. (B) In subject animals, haptoglobin levels fell below the detection limit from 72 hours onwards. Regular statistics could no longer be performed (ND) for these time points. (C) Hemoglobin levels were significantly lower in the subject group from 72 hours onwards. (D) Total serum LDH activity increased significantly at 48 hours, indicating organ and erythrocyte damage. Arrows indicate time points of injection.
Hematologic parameters indicate acute thrombocytopenia and intravascular hemolysis after inhibition of ADAMTS13. (A-D) Hematologic parameters were determined in blood samples from subject (●, n = 6) or control animals (■, n = 5), and mean values ± SD are shown. (A) Subject animals were thrombocytopenic from 24 hours onwards, dropping further to less than 12 × 109/L at 48 hours. (B) In subject animals, haptoglobin levels fell below the detection limit from 72 hours onwards. Regular statistics could no longer be performed (ND) for these time points. (C) Hemoglobin levels were significantly lower in the subject group from 72 hours onwards. (D) Total serum LDH activity increased significantly at 48 hours, indicating organ and erythrocyte damage. Arrows indicate time points of injection.
Peripheral blood smears indicate thrombocytopenia, schistocytes, and reticulocytes in baboons with functional inhibition of ADAMTS13. (A) Peripheral blood smears from a representative animal from each group are shown. Blood was taken and prepared at the moments indicated above the panel. A decrease in platelet numbers as well as the gradual appearance of schistocytes (▴) and reticulocytes (■) is seen in smears from subject but not control animals. Preparation and staining were automated and according to the May-Grunwald-Giemsa protocol. Original magnification (all panels) ×400. (B) Red blood cells were counted manually and blindly in peripheral blood smears from all subject animals (n = 6).The mean percentage ± SD of schistocytes is plotted as a function of time. (A-B) Arrows indicate time points of mAb injection.
Peripheral blood smears indicate thrombocytopenia, schistocytes, and reticulocytes in baboons with functional inhibition of ADAMTS13. (A) Peripheral blood smears from a representative animal from each group are shown. Blood was taken and prepared at the moments indicated above the panel. A decrease in platelet numbers as well as the gradual appearance of schistocytes (▴) and reticulocytes (■) is seen in smears from subject but not control animals. Preparation and staining were automated and according to the May-Grunwald-Giemsa protocol. Original magnification (all panels) ×400. (B) Red blood cells were counted manually and blindly in peripheral blood smears from all subject animals (n = 6).The mean percentage ± SD of schistocytes is plotted as a function of time. (A-B) Arrows indicate time points of mAb injection.
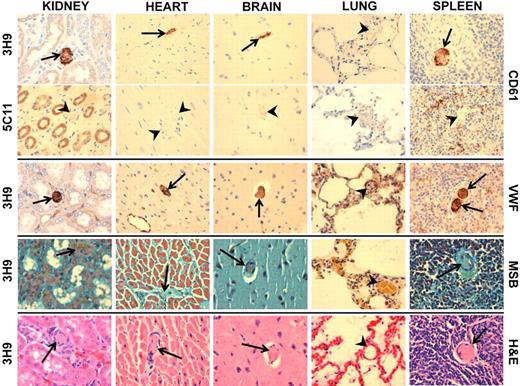
Baboons injected with 3H9 have immunohistochemical features characteristic of TTP
Histologic sections of kidney, heart, spleen, and brain revealed numerous eosinophilic (hyaline) inclusions in small vessels of a subject but not control animal killed after 96 hours of treatment (Figure 5; supplemental Figure 6). Immunohistochemical staining confirmed that the thrombi were characteristic of TTP as these were enriched in VWF and platelet antigen CD61, whereas fibrin was lacking. Thrombi were not detected in lungs, which is consistent with postmortem pathologic studies of human TTP.30 The combination of the hematologic and histologic findings provides sufficient evidence for TTP in all subject animals, suggesting a direct link between inhibition of ADAMTS13 activity and TTP.
Histopathologic analysis confirms disseminated platelet- and VWF-rich aggregates in multiple organs. Tissue sections of kidney, heart, brain, lung, and spleen (indicated above the panel) were prepared and stained as shown to the right; hematoxylin and eosin (H&E), immunohistochemical staining for platelet antigen CD61 and for VWF as well as a Martius yellow, Brilliant crystal scarlet 6R, and Soluble blue (MSB) stain for fibrin. The MSB stain colors both muscle and fibrin bright red and erythrocytes yellow/orange, and nuclei and connective tissue stains blue/purple. Arrows indicate thrombi, and arrowheads indicate open vessels. Original magnification (all panels) ×400.
Histopathologic analysis confirms disseminated platelet- and VWF-rich aggregates in multiple organs. Tissue sections of kidney, heart, brain, lung, and spleen (indicated above the panel) were prepared and stained as shown to the right; hematoxylin and eosin (H&E), immunohistochemical staining for platelet antigen CD61 and for VWF as well as a Martius yellow, Brilliant crystal scarlet 6R, and Soluble blue (MSB) stain for fibrin. The MSB stain colors both muscle and fibrin bright red and erythrocytes yellow/orange, and nuclei and connective tissue stains blue/purple. Arrows indicate thrombi, and arrowheads indicate open vessels. Original magnification (all panels) ×400.
Advanced TTP by continuous injections of 3H9
The experiment with 2 injections of ADAMTS13 inhibitor and 96-hour follow-up induced TTP with limited organ damage except to the myocardium in one of the animals, but without evidence of discomfort. We hypothesized that prolonged inhibition of ADAMTS13 would increase the chance of advanced ischemic organ damage and raise the model to advanced or end stage. One animal continuously received injections of 3H9 every 48 hours for 12 days with blood analysis every 24 hours. The immunoglobulin titer showed a cyclic pattern corresponding to the bolus infusions but without accumulation (supplemental Figure 7). As expected, all initial hematologic indications characteristic of TTP gradually increased during the study. The animal remained thrombocytopenic with an average platelet count of 34 × 109/L (supplemental Figure 8A), serum LDH levels increased further to approximately 5-fold, and haptoglobin remained undetectable (supplemental Figure 8B). Severe anemia set in from day 6 but then leveled at 5 g/dL (supplemental Figure 8C). Blood smears became increasingly indicative for severe schistocytic hemolysis with a large number of reticulocytes and eventually Howell-Jolly bodies (supplemental Figure 8D). The latter were thought to indicate functional hyposplenia probably because of widespread microvascular thrombosis of the spleen with autosplenectomy. At day 6, a sudden but transient increase in troponin-T (0.41 μg/L with cutoff < 0.03; supplemental Figure 9) suggested some myocardial ischemic necrosis. Cardiac ischemia is observed in the majority of TTP patients and is associated with increased mortality and morbidity according to a recent study.31 However, this animal never became noticeably ill, and 4 days after cessation of injections all parameters returned to baseline with no further complications.
Discussion
Our data show that inhibition of ADAMTS13 in baboons consistently causes the characteristic hematologic picture of TTP without the requirement of additional inciting triggers. Consequently, ADAMTS13 function is essential for maintaining microvascular integrity in nonhuman primates. This is in contrast to common laboratory mice where congenital deficiency of ADAMTS13 is prothrombotic but insufficient to cause spontaneous TTP.14,15 Differences between murine and primate physiology may account for this. For instance, certain modifiers, including other proteases32 that can substitute for ADAMTS13 activity, may process VWF more efficiently in mice than in primates.
The consistency of the response to inhibition of ADAMTS13 in baboons is rather unexpected because TTP in human cases with congenital ADAMTS13 deficiency20 as well as in the susceptible Adamts13−/− mouse strain (CASA/Rk)15,33 has a variable time of onset. One possible explanation for this heterogeneity in human congenital TTP is that numerous ADAMTS13 mutations may result in diverse plasma ADAMTS13 activities below the detection limit of currently available assays (∼ 5%),34 which would still be sufficient to prevent spontaneous recurrent TTP.20,35 This is substantiated by the observation that women with a specific hereditary ADAMTS13 deficiency get acute TTP only on pregnancy, although their equally deficient brothers remain asymptomatic.36 Furthermore, a subset of TTP patients attains remission after plasma exchange treatment despite ADAMTS13 levels less than 5%.37-40 In addition, some polymorphisms drastically decrease ADAMTS13 activity41,42 with no reported medical consequences. Our findings are in line with this because the control animals injected with 5C11 have reduced ADAMTS13 activity as well, yet without signs of disease. Contrary to this, Upshaw-Schulman syndrome is the rare congenital TTP variant that spontaneously sets in immediately after birth and is characterized by a chronic relapsing course requiring prophylactic infusion of donor plasma to constantly replenish the deficient enzyme.21,22,43 Taken together, this implies that a threshold ADAMTS13 activity, probably less than 5%, underlies spontaneous precipitation of disease44 (ie, in the absence of an obvious external inciting trigger). We assume that ADAMTS13 inhibition in the subject baboons is below this critical level because the 3H9 plasma concentrations achieved in these animals exceed the dissociation constant of the antibody-antigen interaction by far, indicating all ADAMTS13 molecules are occupied with inhibitor. This does not, however, rule out that TTP can be incited when ADAMTS13 activity levels are above threshold because patients with measurable ADAMTS13 activity may still develop TTP.37 Although in that context, triggers such as pregnancy or infection probably play a substantial role by precipitating acute illness through a currently unknown mechanism. Therefore, our results do not exclude supplementary roles for triggers; rather, they situate them in a specific context.
Another significant difference with the current Adamts13−/− mouse model is that half of the shigatoxin-treated CASA/Rk mice died,15 whereas all baboons in our experiment survived. Even systemic inhibition of ADAMTS13 for as long as 2 weeks in a selected animal did not cause death. Before plasma exchange treatment, the average duration of hospitalization of TTP patients was 14 days before death,45,46 not taking into account a potential presymptomatic period. This could mean that the human and primate organs tolerate the process of ongoing thrombosis for a relatively long time. This may be because thrombi in TTP are disseminated in multiple organs47,48 and there allocate to terminal arterioles rather than to large afferent vessels. It is, therefore, possible that additional exogenous triggers accelerate the disease. lifting it to an advanced stage by acting synergistically with the ADAMTS13 deficiency and rendering organs more susceptible to the consequences of microangiopathy. This has been observed in a patient homozygous for the 4314insA ADAMTS13 mutation who presented with mild TTP symptoms, which however exacerbated during pregnancy.49 In that respect, certain triggers may not function merely to incite disease, and it therefore remains difficult to speculate how much longer the one animal with long-term ADAMTS13 inhibition could have survived the ongoing TTP.
Our model particularly reflects the early stages of acute acquired idiopathic TTP. In humans, this phase is poorly described, mostly because patients who seek medical assistance generally already have signs of organ damage (ie, advanced-stage TTP).50 Our data confirm that the early stages do not cause considerable discomfort, which is in line with the minor signs of organ dysfunction in the baboons with TTP. In addition, in humans, TTP has been suggested to present mildly36,50,51 before precipitating as an acute perceptible bout with symptoms of failing organs. Our study thus confirms and justifies the newly adapted diagnostic standard for TTP,6,45 including thrombocytopenia with schistocytic hemolytic anemia in the absence of a primary illness but no longer requiring former criteria of advanced disease, such as neurologic and renal dysfunction. Consequently, our baboon model of TTP is ideally suited for preclinical testing of new treatment strategies because it provides consistency without animal discomfort. Moreover, the model can be used to address the role, effect, and nature of reported triggers.
Taken together, our results show that ADAMTS13 activity is essential for microvascular integrity in primates as TTP spontaneously and quickly occurs after ADAMTS13 inhibition in the absence of additional triggers. We are the first to demonstrate the initial stages of acquired idiopathic TTP, suggesting that these may go by relatively unnoticed as measurable organ failure and/or death are not seen before 96 hours of ADAMTS13 inhibition. Consequently, our model offers an opportunity for clinical and basic research on TTP by providing a framework for alternative therapies and novel insights.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank J. Evan Sadler and Piermannuccio Mannucci for helpful discussions, expertise, advice, and support; Denise Stuart and Gerda Le Roux for their assistance with histology slide preparations; Raf Sciot and Cathy Beukes for help with histology interpretation; and Elson Mberi for blindly counting schistocytes on peripheral blood smears.
This work was supported by the KU Leuven (grant GOA/09/829), the Flemish Fonds voor Wetenschappelijk Onderzoek (grant FWO G.0299.06), and the Department of Hematology and Cell Biology, University of the Free State (internal funds). H.B.F. is a fellow of the Flemish Fonds voor Wetenschappelijk Onderzoek. P.J.A. is supported by the American Heart Association (grant-in-aid 09GRNT2220282).
Authorship
Contribution: H.B.F. and J.R. designed research, performed experiments, and interpreted data; H.B.F. provided essential reagents and wrote the paper; J.R. and V.J.L. were responsible for the animal study design and supervised animal experimentation; J.R. coordinated the animal experimentation; K.V. designed research, provided essential reagents, interpreted data, coordinated tool development, and wrote the paper; H.D. designed research and provided essential reagents; I.P., N.V., S.L., and W.J.v.R. performed experiments; V.J.L. and P.N.B. assisted as experts in clinical hematology and pathology; P.J.A. provided essential reagents and revised the manuscript; U.B. performed VWF multimer analysis; and all authors critically reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests. The authors had no financial interest in the development of an animal model for TTP.
Correspondence: Hendrik B. Feys, Laboratory for Thrombosis Research, Katholieke Universiteit Leuven Campus Kortrijk, E Sabbelaan 53, 8500 Kortrijk, Belgium; e-mail: hendrik.feys@kuleuven-kortrijk.be.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal