Key Points
Exome sequencing of adult ETP-ALL reveals new recurrent mutations; in particular, DNMT3A is frequently mutated in adult ETP-ALL.
More than 60% of all adult patients with ETP-ALL harbor a mutation that could potentially be targeted by a specific therapy.
Abstract
Early T-cell precursor (ETP) acute lymphoblastic leukemia (ALL) is a high-risk subgroup of T-lineage ALL characterized by specific stem cell and myeloid features. In adult ETP-ALL, no comprehensive studies on the genetic background have been performed to elucidate molecular lesions of this distinct subgroup. We performed whole-exome sequencing of 5 paired ETP-ALL samples. In addition to mutations in genes known to be involved in leukemogenesis (ETV6, NOTCH1, JAK1, and NF1), we identified novel recurrent mutations in FAT1 (25%), FAT3 (20%), DNM2 (35%), and genes associated with epigenetic regulation (MLL2, BMI1, and DNMT3A). Importantly, we verified the high rate of DNMT3A mutations (16%) in a larger cohort of adult patients with ETP-ALL (10/68). Mutations in epigenetic regulators support clinical trials, including epigenetic-orientated therapies, for this high-risk subgroup. Interestingly, more than 60% of adult patients with ETP-ALL harbor at least a single genetic lesion in DNMT3A, FLT3, or NOTCH1 that may allow use of targeted therapies.
Introduction
T-lineage acute lymphoblastic leukemia (T-ALL) accounts for approximately 25% of all adult ALL. The novel high-risk subgroup of early T-cell precursor (ETP) represents 10% of all adult T-ALL. This subgroup is characterized by a specific immunophenotype (CD1-, CD5weak, CD8-, or coexpression of stem cell and/or myeloid markers) and distinct molecular features (FLT3 mutations and an absence of NOTCH1 mutations).1,2 ETP-ALL, regarded as stem cell–like leukemia, is associated with a high risk for treatment failure for both pediatric and adult patients. Because of the myeloid features of ETP-ALL, it was proposed that these patients might benefit from therapies used in myeloid malignancies, including high-dose cytarabine or epigenetic modulators.3
Although in pediatric ETP-ALL whole-genome sequencing has revealed a highly heterogeneous picture of genetic alterations,4 no comprehensive molecular analyses have been performed in adult ETP-ALL. Here we systematically screened for somatic mutations in adult ETP-ALL. We have analyzed exomes of 5 patients and subsequently verified mutations in DNMT3A and members of the polycomb repressor complex 2 (PRC2) in a larger cohort of adult patients with ETP-ALL.
Study design
Patients
We investigated paired bone marrow samples of 5 adult patients with ETP-ALL (supplementary Methods and supplementary Table 1, available on the Blood Web site) with sufficient genomic DNA at diagnosis and in remission (minimal residual disease5 level < 4 × 10−3) that had been sent to the reference laboratory within the German Acute Lymphoblastic Leukemia Multicenter (GMALL) study group. In addition, 68 adult patients with ETP-ALL (55 men, 13 women; median age, 38 years) were analyzed for the mutation status of selected genes (DNMT3A, EZH2, EP300, SH2B3, and SUZ12). For 52 (76%) of the 68 patients, clinical follow-up data were available (supplementary Tables 2 and 3). All patients gave written informed consent to participate in the study according to the Declaration of Helsinki. The studies were approved by the ethics board of the Johann Wolfgang Goethe-Universität of Frankfurt/Main in Germany.
Exome sequencing and mutation analysis
The methods are described in the supplemental Data. In brief, exome sequencing was performed for 5 adult patients with ETP-ALL, as previously reported,6,7 using exon capturing from genomic DNA (Sure Select target enrichment; Agilent, Santa Clara, CA), followed by 76-bp paired-end sequencing on an Illumina Genome Analyzer IIx platform (Illumina, San Diego, CA). Candidate variants were confirmed by capillary sequencing of genomic DNA.
Mutation analyses for EZH2 (exons 14-20), SH2B3 (exons 2-8), DNMT3A (exons 13-23), EP300 (exon 30), and SUZ12 (exons 14-15) were performed by Sanger sequencing in 68 adult patients with ETP-ALL. Primers are listed in the supplement (supplementary Table 4). All samples had been previously analyzed for FLT3 and NOTCH1 mutations.2
Statistical analyses were performed using SPSS software version 17 (SPSS Inc, Chicago, IL) and GraphPad Prism software version 5 (GraphPad Software Inc, La Jolla, CA).
Results and discussion
As no comprehensive analysis exists on the molecular background of the high-risk subgroup of adult ETP-ALL, we performed whole-exome sequencing in 5 adult patients (supplementary Table 1). At least 3.8 Gbp of exome sequence was generated for each sample (supplementary Table 5). We found a total of 63 nonsynonymous somatic mutations or indels in 5 patients with ETP-ALL (range, 6-16 per patient). Eleven mutations/indels affected cancer genes, according to the census of human cancer genes8 (see also http://www.sanger.ac.uk/genetics/CGP/Census). Recurrent mutations affected DNMT3A and FAT3 (FAT, tumor suppressor homolog 3) in 2 of the 5 patients. The DNA-methyl-transferase DNMT3A is a frequent mutational target in acute myeloid leukemia (AML; 20%),9 whereas FAT3 mutations were reported in ovarian carcinoma.10 New mutational targets identified involved genes in epigenetic regulation (MLL2, BMI1, and FAT1) and genes reported to be mutated in pediatric ETP-ALL and other ALL subgroups (JAK1, ETV6, NOTCH1, DNM2, and NF1)4,11,12 (supplementary Table 6).
Deregulated DNA methylation is a commonly found in many malignancies.13 DNMT3A is mutated in myelodysplastic syndrome (8%) and AML,9,14 where it is associated with a poor prognosis.9,15-18 As the same mutations occur in myelodysplastic syndrome and the corresponding secondary AML,19 DNMT3A mutations likely represent an early event in leukemogenesis.20 Until now, a single study has reported a single DNMT3A mutation in T-ALL, and just recently, a second paper described frequent mutations of DNMT3A in adult T-ALL, although not specifying ETP-ALL.21,22 Interestingly, no DNMT3A mutations were identified by whole-genome sequencing in pediatric ETP-ALL.4
By Sanger sequencing, we determined the frequency of DNMT3A mutations in a large cohort of adult ETP-ALL. In 16% of the 68 patients with ETP-ALL, DNMT3A was mutated, reflecting a mutation rate similar to that of AML, with a similar mutation pattern and mutational hot spot in exon 23. Amino acid R882 of DNMT3A was mutated in 5 ETP-ALL samples. Four of the 6 remaining mutations were previously described in AML (supplementary Figure 1).9,15,23
With respect to clinical characteristics, no difference was observed between DNMT3A mutated and wild-type patients regarding sex distribution. In addition, DNMT3A mutated and wild-type patients did not differ in the immunophenotype or the mutational status of NOTCH1 and FLT3 (Table 1 and supplementary Table 3). Thus, in contrast to AML, no association between DNMT3A and FLT3 mutations can be found.9,15,23 Similar to in AML,9,16 patients with ETP-ALL with DNMT3A mutations were significantly older (median, 63 vs 37 years; P = .016) than patients with DNMT3A wild-type (Table 1). The lack of DNMT3A mutations in pediatric ETP-ALL and the low rate of DNMT3A mutations in pediatric AML24,25 point toward age-specific genetic differences. Because of the occurrence of genetic alterations in epigenetic regulators, we verified genetic mutations, including members of PRC2 in a larger ETP-ALL cohort (n = 68). Mutations were found for EZH2 in 4 of 68 (6%) and SUZ12 in 1 of 68 (1%) of adult ETP-ALL (supplementary Figure 2). No mutation was found in EP300. Thus, in contrast to pediatric ETP-ALL, with a high rate of mutations in PRC2,4,21 we found a low rate of PRC mutations in adult ETP-ALL. DNMT3A mutations had no significant prognostic effect in this small cohort of adult ETP-ALL. Patients with at least a single mutation in epigenetic regulators (DNMT3A, SUZ12, EP300, or EZH2) showed a trend toward inferior survival compared with unaffected patients (1-year survival, 56% vs 88%; log rank, P value = .24; Breslow, P value = .16; supplementary Figure 3).
Characteristics of adult patients with ETP-ALL and comparison between DNMT3A mutated and DNMT3A wild-type patients
| Characteristic . | DNMT3mut (n = 11) . | DNMT3wt (n = 57) . | P . | ||
|---|---|---|---|---|---|
| n . | % . | n . | % . | ||
| Sex | .35 | ||||
| Female | 3 | 27.3 | 10 | 17.6 | |
| Male | 8 | 72.7 | 47 | 82.4 | |
| Age, y | .02 | ||||
| Median | 63 | 37 | |||
| Range | 24-73 | 17-74 | |||
| Clinical data available | .27 | ||||
| n | 7 | 64 | 45 | 79 | |
| FLT3 | .41 | ||||
| Mutated | 3 | 27.3 | 21 | 36.8 | |
| Wild-type | 8 | 72.7 | 36 | 63.2 | |
| NOTCH1 | .68 | ||||
| Mutated | 1 | 9.1 | 9 | 15.8 | |
| Wild-type | 10 | 90.9 | 48 | 84.2 | |
| EZH2 | .52 | ||||
| Mutated | 1 | 9.1 | 3 | 5.3 | |
| Wild-type | 10 | 90.9 | 54 | 94.7 | |
| SH2B3 | .49 | ||||
| Mutated | 0 | 0 | 4 | 7 | |
| Wild-type | 11 | 100 | 53 | 93 | |
| SUZ12 | .84 | ||||
| Mutated | 0 | 0 | 1 | 1.8 | |
| Wild-type | 11 | 100 | 56 | 98.2 | |
| Characteristic . | DNMT3mut (n = 11) . | DNMT3wt (n = 57) . | P . | ||
|---|---|---|---|---|---|
| n . | % . | n . | % . | ||
| Sex | .35 | ||||
| Female | 3 | 27.3 | 10 | 17.6 | |
| Male | 8 | 72.7 | 47 | 82.4 | |
| Age, y | .02 | ||||
| Median | 63 | 37 | |||
| Range | 24-73 | 17-74 | |||
| Clinical data available | .27 | ||||
| n | 7 | 64 | 45 | 79 | |
| FLT3 | .41 | ||||
| Mutated | 3 | 27.3 | 21 | 36.8 | |
| Wild-type | 8 | 72.7 | 36 | 63.2 | |
| NOTCH1 | .68 | ||||
| Mutated | 1 | 9.1 | 9 | 15.8 | |
| Wild-type | 10 | 90.9 | 48 | 84.2 | |
| EZH2 | .52 | ||||
| Mutated | 1 | 9.1 | 3 | 5.3 | |
| Wild-type | 10 | 90.9 | 54 | 94.7 | |
| SH2B3 | .49 | ||||
| Mutated | 0 | 0 | 4 | 7 | |
| Wild-type | 11 | 100 | 53 | 93 | |
| SUZ12 | .84 | ||||
| Mutated | 0 | 0 | 1 | 1.8 | |
| Wild-type | 11 | 100 | 56 | 98.2 | |
To further explore these genetic alterations as recurrent events, additional patients with ETP-ALL (n = 20) were analyzed by targeted next-generation sequencing (supplemental Data). In addition to DNMT3A, mutations in MLL2 (10%), previously linked to lymphoma,26 underscore the relevance of alterations in epigenetic regulators. Moreover, mutations in the cadherins FAT1 (25%) and FAT3 (20%) implicate alterations in cell adhesion, interaction mechanisms, and activation of the Wnt pathway.27 In particular, FAT1 may act as a tumor suppressor.27 Finally mutations DNM2 (35%) and JAK1 (15%)4 point to molecular targets for novel therapies (supplementary Figure 4, supplementary Figure 5, and supplementary Table 7).
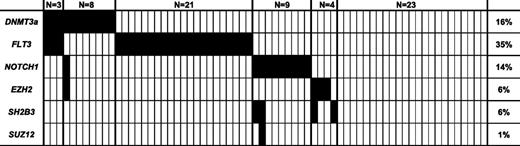
In conclusion, adult ETP-ALL displays a distinct mutation spectrum, particularly affecting genes involved in epigenetic regulation (in particular, MLL2, DNMT3A, and PRC2). This mutation spectrum is different for pediatric patients, with a lower rate of PRC2 mutations and a higher rate of DNMT3A mutations pointing toward distinct molecular alterations in adult ETP-ALL. This might result from preexisting lesions in the hematopoietic progenitors, as it was shown that TET2 mutations result in an age-related myeloid lineage bias in elderly individuals.28 DNMT3A mutations in adult ETP-ALL show a similar frequency to that seen in AML, are located at the same hot spot, and are in conjunction with mutations in other epigenetic regulators of potential unfavorable prognostic effect, underscoring the stem cell/myeloid origin of ETP-ALL. These data may provide a potential rationale to study epigenetic directed therapies in the high-risk subgroup of ETP-ALL. Importantly, we can now define at least 3 different molecular subgroups of adult ETP-ALL characterized by alterations in epigenetic regulators (25%), mutations in FLT3 (35%) and other kinases (JAK pathway), and the presence of NOTCH1 mutations (15%) (Figure 1).2 In total, more than 60% of all adult patients with ETP-ALL harbor alterations that can potentially be molecularly targeted by new treatment approaches such as demethylating agents, kinase inhibitors, and γ secretase inhibitors.
The spectrum of mutations in DNMT3A, FLT3, NOTCH1, EZH2, SH2B3, and SUZ12 in 68 adult patients with ETP-ALL.
The spectrum of mutations in DNMT3A, FLT3, NOTCH1, EZH2, SH2B3, and SUZ12 in 68 adult patients with ETP-ALL.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Liliana H. Mochmann for critical reading of the manuscript.
This work was supported by grants from the Deutsche Krebshilfe (Mildred Scheel Professur) and Gutermuth-Stiftung (C.D.B.) and the Deutsche Krebshilfe (70-2657-Ho2 [D.H.], BMBF 01GI 9971 [D.H. and N.G.], and 109031 [P.A.G. and S.K.B.]).
Authorship
Contribution: M.N. contributed to the research, analyzed data, and wrote the manuscript; S.S. supervised the reference laboratory and reviewed the manuscript; N.G. supervised the GMALL study center and reviewed the manuscript; D.H. supervised the GMALL study group; S.H., C.S., N.P.K., B.K., S.V., A.G., S.K., H.B., T.R., M.B., J.H., and S.K.B. contributed to the research; W.-K.H. contributed to the study analysis and reviewed the manuscript; P.A.G. designed the research, contributed to the data analysis, and edited the manuscript; C.D.B. designed the research, contributed to the data analysis, and edited the manuscript; and P.A.G. and C.D.B. jointly supervised the study.
Conflict-of-interest disclosure: P.A.G. and S.K. received honoraria from Illumina. The remaining authors declare no competing financial interests.
Correspondence: Claudia D. Baldus, Charité, University Hospital Berlin, Campus Benjamin Franklin, Department of Hematology and Oncology, Hindenburgdamm 30, 12203 Berlin, Germany; e-mail: claudia.baldus@charite.de.
References
Author notes
P.A.G. and C.D.B. contributed equally to this study.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal