Key Points
Decitabine priming increases antileukemic effects of selinexor in AML in vitro and in vivo.
Decitabine priming allows for decreasing the dose of selinexor in patients, thus increasing tolerability without affecting antileukemic activity.
Abstract
The prognosis of acute myeloid leukemia (AML) is poor, highlighting the need for novel treatments. Hypomethylating agents, including decitabine are used to treat elderly AML patients with relative success. Targeting nuclear export receptor (exportin 1 [XPO1]) is a novel approach to restore tumor suppressor (TS) function in AML. Here, we show that sequential treatment of AML blasts with decitabine followed by selinexor (XPO1 inhibitor) enhances the antileukemic effects of selinexor. These effects could be mediated by the re-expression of a subset of TSs (CDKN1A and FOXO3A) that are epigenetically silenced via DNA methylation, and cytoplasmic-nuclear trafficking is regulated by XPO1. We observed a significant upregulation of CDKN1A and FOXO3A in decitabine- versus control-treated cells. Sequential treatment of decitabine followed by selinexor in an MV4-11 xenograft model significantly improved survival compared with selinexor alone. On the basis of these preclinical results, a phase 1 clinical trial of decitabine followed by selinexor in elderly patients with AML has been initiated.
Introduction
Acute myeloid leukemia (AML) is a clonal hematopoietic disorder characterized by genetic and epigenetic alterations leading to a block in differentiation and accumulation of leukemic blasts in blood and bone marrow (BM).1 Epigenetic silencing of genes involved in hematopoietic differentiation plays a critical role in myeloid leukemogenesis.2,3 Gene silencing caused by DNA hypermethylation can be reversed pharmacologically by inhibition of DNA methyltransferases (DNMTs) using azanucleosides such as decitabine.2,3 Our group recently reported a 47% complete response rate with a 10-day regimen of low-dose decitabine as a single agent in previously untreated older AML patients (>60 years).4 Although patients’ survival was not significantly better than that obtained with more intensive chemotherapy regimens (ie, 7 + 3), the single-agent decitabine regimen was well tolerated and had low toxicity. These results therefore suggest the opportunity to capitalize on this relatively nontoxic treatment and make it more effective by incorporating this compound into novel molecularly targeted approaches. Exportin 1 (XPO1) is a nuclear exporter involved in the active transport of a number of cargo proteins, including transcription factors and tumor suppressor proteins (TSPs; ie, p53 and p27), cell-cycle regulators (ie, Cdkn1a), and RNA molecules.5,6 Recent data indicate that TSP can be exported from the nucleus and thereby inactivated in cancer by hyperactive nuclear export.7 Indeed, XPO1 overexpression has been reported in several solid tumors and leukemias, including AML, and it is associated with worse outcome.8,9 Thus, XPO1 inhibition may result in increased levels of active TSP, and orally bioavailable selective inhibitors of nuclear export (SINE) that covalently bind and inhibit XPO1 are being explored as a novel therapeutic approach in solid tumors and hematologic malignancies.10,11 Our group recently reported the antileukemic activity of SINEs in vitro and in vivo in AML.11 SINEs displayed potent antiproliferative properties at submicromolar concentrations with regard to apoptosis, cell-cycle arrest, and myeloid differentiation in AML cell lines and patient blasts.11 Finally, using the FLT3-internal tandem duplication (ITD) –positive MV4-11 xenograft murine model, we show that treatment of mice with oral SINE significantly prolongs survival of leukemic mice.11 These preclinical studies have supported the development of a large phase 1 clinical trial with selinexor (last-generation SINE) in patients with advanced hematologic malignancies, including AML. Preliminary data indicate that selinexor is well tolerated, safe, and active in refractory/relapsed AML patients.12 However, considering the molecular complexity of AML, it is unlikely that this disease can be cured with monotherapy, and therefore we asked whether adding an already established effective drug such as decitabine to selinexor would enhance or improve its antileukemic effects in AML.
Methods
Cell lines
AML cell lines, MV4-11, MOLM-13 and OCI-AML3 were purchased from DSMZ, Germany. All cell lines were cultured in RPMI supplemented with 10% fetal bovine serum (FBS) and 100 U/mL penicillin and 100 μg/mL streptomycin.
Primary AML samples
Newly diagnosed untreated and frozen BM samples from AML patients were obtained from the Ohio State University Leukemia Tissue Bank after obtaining informed consent approved by the cancer institution review board.
Further detailed methods are provided in the Figure legends and in the supplemental Data (available on the Blood Web site).
Results and discussion
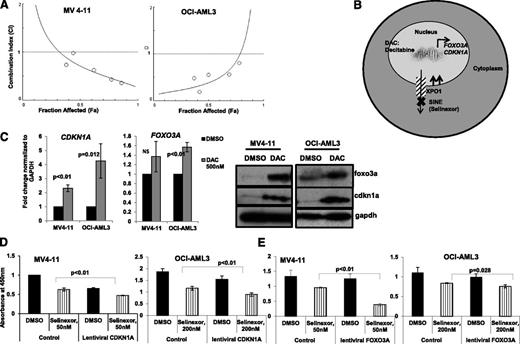
We initially treated two AML cell lines (OCI-AML3 and MV4-11) concomitantly with decitabine and selinexor at twofold dilutions of their individual concentration that inhibits 50% (IC50) values and measured cell proliferation by using the WST-1 assay at 48 hours. The combination index (CI) was calculated according to the Chou-Talalay method.13 The CIs for the different combinations were around 1 or above 1, indicating no synergy (supplemental Figure 1). Because decitabine is a cell cycle–dependent nucleoside analog, we reasoned that these results could be explained by the cell cycle arrest induced by selinexor. Next we asked whether sequential treatment would be more effective. For this approach, we used the WST-1 assay in which cells were exposed to decitabine (IC50 twofold dilutions, 4 μM to 250 nM) for 24 hours followed by selinexor (IC50 twofold dilutions, 400nm to 25nM) for 24 hours (supplemental Table 1). This sequential treatment resulted in CI values below 1, indicating synergy as calculated by the Chou-Talalay method (Figure 1A and supplemental Table 2). These results were validated by using a third AML cell line, MOLM-13 (supplemental Figure 2A). In addition, a significant induction of apoptosis was observed (supplemental Figure 3).
Decitabine priming enhances selinexor antileukemic effects in vitro. (A) CI plots of decitabine (DAC) with selinexor. The effect of the combinations was assessed by WST-1 assay after initial priming with DAC (24 hours) followed by selinexor treatment for 24 hours. The doses for both drugs were chosen according to their individual IC50 (twofold dilutions), which were determined by using the WST-1 assay (supplemental Table 1). Because DAC was given for 48 hours, we determined the DAC IC50 at 48 hours. The IC50 for selinexor was determined at 24 hours because the treatment with this drug was shorter. The effects of the combinations were calculated by using CalcuSyn software, where CI < 1 indicates synergy, CI = 1 is additive, and CI > 1 is antagonistic. (B) Schematic illustrating the hypothesis. (C) Fold change in CDKN1A and FOXO3a messenger RNA (mRNA) expression by real-time polymerase chain reaction (PCR) (24 hours) and western blot (48 hours) of the same to show change in protein expression. (D) WST-1 assay of cell lines treated with control or lentiviral vector expressing CDKN1A (p21) followed by selinexor treatment. (E) WST-1 assay of cell lines treated with control or lentiviral vector expressing FOXO3A followed by selinexor treatment. Selinexor was introduced to cell culture 24 hours after transfection. Assays were performed at indicated time points.
Decitabine priming enhances selinexor antileukemic effects in vitro. (A) CI plots of decitabine (DAC) with selinexor. The effect of the combinations was assessed by WST-1 assay after initial priming with DAC (24 hours) followed by selinexor treatment for 24 hours. The doses for both drugs were chosen according to their individual IC50 (twofold dilutions), which were determined by using the WST-1 assay (supplemental Table 1). Because DAC was given for 48 hours, we determined the DAC IC50 at 48 hours. The IC50 for selinexor was determined at 24 hours because the treatment with this drug was shorter. The effects of the combinations were calculated by using CalcuSyn software, where CI < 1 indicates synergy, CI = 1 is additive, and CI > 1 is antagonistic. (B) Schematic illustrating the hypothesis. (C) Fold change in CDKN1A and FOXO3a messenger RNA (mRNA) expression by real-time polymerase chain reaction (PCR) (24 hours) and western blot (48 hours) of the same to show change in protein expression. (D) WST-1 assay of cell lines treated with control or lentiviral vector expressing CDKN1A (p21) followed by selinexor treatment. (E) WST-1 assay of cell lines treated with control or lentiviral vector expressing FOXO3A followed by selinexor treatment. Selinexor was introduced to cell culture 24 hours after transfection. Assays were performed at indicated time points.
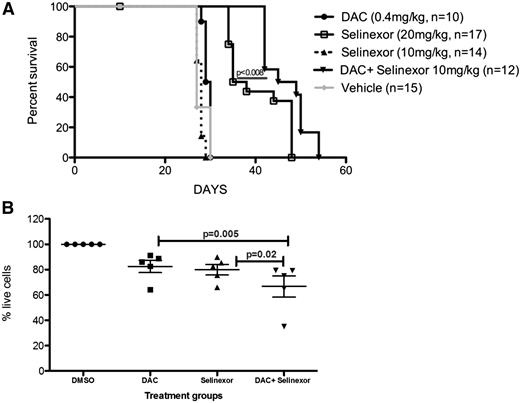
Thus, we hypothesized that these effects could be mediated by the re-expression of a subset of nuclear tumor suppressors (ie, CDKN1A (p21) and FOXO3A)14,15 that are epigenetically silenced via DNA methylation and whose cytoplasmic-nuclear trafficking is regulated by XPO16 (Figure 1B). We observed that decitabine treatment increased CDKN1A and FOXO3A expression levels at both the RNA and protein level in the AML cell lines OCI-AML3, MV4-11, and MOLM-13 (Figure 1C and supplemental Figure 2B), which supports this hypothesis. These 2 genes were also found upregulated in cell lines and BM samples from AML patients treated with hypomethylation agents.14,15 To further delineate the mechanism of this enhanced antileukemic activity, we overexpressed CDKN1A by using a lentiviral vector in both OCI-AML3 and MV4-11 cells (to mimic the priming effect of decitabine) and subsequently treated them with selinexor. Similar to the decitabine-selinexor treatment, ectopic CDKN1A and FOXO3A overexpression in OCI-AML3 and MV4-11 cells followed by selinexor treatment at values lower than IC50 resulted in significantly decreased cellular proliferation (Figure 1D-E) and increased apoptosis (supplemental Figures 4 and 5) as compared with selinexor alone. Expression levels of lentiviral-induced CDKN1A and FOXO3A were validated by real-time polymerase chain reaction (PCR) (supplemental Figure 6). We then tested the efficacy of the combination in vivo by using an established xenograft mouse model of AML. MV4-11 cells obtained from spleens of primary MV4-11 xenografts were transplanted into nonobese diabetic/severe combined immunodeficient (NOD-SCID) γ (NSG) mice via tail vein. Mice were monitored closely for clinical signs of leukemia as described in Methods. One week after leukemia cell injection, the mice were given either vehicle control, decitabine alone (0.4 mg/kg intraperitoneally twice per week), selinexor alone (20 mg/kg oral gavage twice per week), selinexor alone (10 mg/kg oral gavage twice per week), or decitabine (0.4 mg/kg intraperitoneally twice per week on Mondays and Tuesdays) followed by selinexor (10 mg/kg oral gavage twice per week given on Wednesdays and Fridays). All treatments were given for 3 weeks after leukemia cell injection. Single-agent selinexor at 10 mg/kg or decitabine alone had no effect in prolonging the survival of mice with respect to the control mice (vehicle control). In contrast, decitabine (0.4 mg/kg) followed by selinexor (10 mg/kg), significantly increased the survival of the mice even when compared with selinexor alone at higher dose (20 mg/kg; 47 vs 36.5 days; P < .008; Figure 2A). On day 25, separate cohorts of vehicle- and drug-treated mice were euthanized; spleens were harvested and photos were taken for comparative study of spleen size. The mice treated with the decitabine-selinexor combination exhibited smaller spleen size than the other groups and controls (supplemental Figure 7). Finally, we validated the efficacy of the sequential drug treatment in vitro by using primary AML blasts. In supplemental Table 3, we report patient’s cytogenetic and molecular characteristics and concentrations of decitabine and selinexor treatments. The initial priming by decitabine followed by selinexor treatment significantly decreased the percentage of live cells compared with either decitabine treatment alone (P = .005; Figure 2B) or selinexor treatment alone (P = .02; Figure 2B) as measured by apoptosis.
Decitabine priming enhances selinexor antileukemic effects in vivo. (A) Survival curve of NSG mice injected with MV4-11 xenografts and treated with indicated drugs. Survival comparison was made with a log-rank test. (B) Patients’ primary AML blasts were treated with DAC for 16 hours followed by selinexor for 24 hours. Controls included dimethylsulfoxide (DMSO), DAC alone, and selinexor treatments alone. Cell viability was measured by using Annexin V/propidium iodide (PI) staining, and DMSO treated cells were normalized to 100% for comparison between treatment groups.
Decitabine priming enhances selinexor antileukemic effects in vivo. (A) Survival curve of NSG mice injected with MV4-11 xenografts and treated with indicated drugs. Survival comparison was made with a log-rank test. (B) Patients’ primary AML blasts were treated with DAC for 16 hours followed by selinexor for 24 hours. Controls included dimethylsulfoxide (DMSO), DAC alone, and selinexor treatments alone. Cell viability was measured by using Annexin V/propidium iodide (PI) staining, and DMSO treated cells were normalized to 100% for comparison between treatment groups.
In summary, we show here that decitabine priming increased the antileukemic effects of selinexor in AML in vitro and in vivo. It should be underscored that the decitabine priming enhanced the antileukemic activity of selinexor at lower doses compared with the treatment of selinexor alone at higher doses. This is relevant to patients because it is now possible to use lower doses of selinexor to increase tolerability without compromising the antileukemia activity. On the basis of these preclinical results, we have launched a phase 1 clinical trial of decitabine followed by selinexor in newly diagnosed elderly (≥60 years) patients with AML who are not eligible for therapy and primary refractory/relapsed AML at The Ohio State University (OSU-13182; NCT02093403).
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Donna Bucci and David Lucas for providing us with primary AML samples from the Ohio State University Leukemia Tissue Bank.
Supported by National Institutes of Health, National Cancer Institute grants P50CA140158 and R01 CA188269, Leukemia and Lymphoma Society Scholar Award (R.G.) and Leukemia and Lymphoma Society Special Fellow Award (P.R.).
Authorship
Contribution: P.R., X.Y., R.S., and J.H. performed all the experiments; P.R., A.W., K.W., R.K., B.B., S.D., S.V., W.B., M.K., M.A.P., S.S., G.M., and R.G. designed research, analyzed data and manuscript; and P.R. and R.G. wrote the manuscript.
Conflict-of-interest disclosure: M.K. and S.S. are employees of Karyopharm Therapeutics, a clinical stage biopharmaceutical company that develops selective inhibitors of nuclear export-targeted therapeutics. The remaining authors declare no competing financial interests.
Correspondence: Ramiro Garzon, The Ohio State University, Comprehensive Cancer Center, Biomedical Research Tower, Room 1084, 460 West 12th Ave, Columbus, OH 43210; e-mail: ramiro.garzon@osumc.edu.
References
Author notes
P.R. and X.Y. contributed equally to this study.