Issue Archive
Table of Contents
BLOOD COMMENTARIES
CLINICAL TRIALS AND OBSERVATIONS
Fixed-duration epcoritamab plus R2 drives favorable outcomes in relapsed or refractory follicular lymphoma
Clinical Trials & Observations
The CD3×CD20 bispecific antibody epcoritamab synergizes with both lenalidomide and rituximab in preclinical models. Falchi and colleagues report an open-label, multicenter phase 1b/2 study evaluating fixed-duration epcoritamab with rituximab and lenalidomide (R2) in 108 patients with relapsed or refractory follicular lymphoma. Efficacy was impressive in these predominantly high-risk patients, with 88% achieving a complete response, many with elimination of measurable residual disease, and 76% remaining progression free at 2 years, while cytokine release syndrome, neutropenia, and infections are common toxicities. Phase 3 trials are now in progress.
GENE THERAPY
A prime editing strategy to rewrite the γ-globin promoters and reactivate fetal hemoglobin for sickle cell disease
Brief Report
Reactivating fetal hemoglobin (HbF) expression is a proven way to ameliorate the severity of sickle cell disease, but the most effective and permanent way to do this remains to be defined. Chalumeau et al explored optimization of multiplex prime editing as potential gene therapy for β-hemoglobinopathies. They demonstrate that multiple edits can be precisely incorporated in the γ-globin promoter, leading to superior reactivation of HbF expression in preclinical experiments and paving the way to clinical trials of next-generation gene editing.
IMMUNOBIOLOGY AND IMMUNOTHERAPY
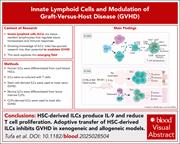
Innate lymphoid cells prevent graft-versus-host disease via IL-9–driven T-cell senescence
Innate lymphoid cells (ILCs) are lymphocytes that lack rearranged antigen-specific receptors and play a crucial role in maintaining immune homeostasis. Prior studies indicate a protective effect against graft-versus-host disease (GVHD), prompting Tufa et al to investigate the mechanism. The researchers found that ILCs induce T-cell senescence via secretion of interleukin-9 (IL-9) and thereby reduce alloreactive T-cell proliferation and consequent GVHD. These data support further clinical investigation of cellular therapy for GVHD.
LYMPHOID NEOPLASIA
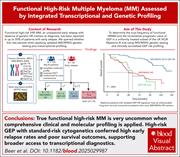
Challenging the concept of functional high-risk myeloma through transcriptional and genetic profiling
Clinical Trials & Observations
When patients with multiple myeloma without adverse genetic or clinical features suffer early relapse despite standard therapy, they are considered to have functional high-risk myeloma. Beer and colleagues retrospectively identified 25 such patients from a completed clinical trial and asked whether they could be identified as high risk at diagnosis in 2025 using the newly published high-risk definition from the International Myeloma Society (IMS) and International Myeloma Working Group (IMWG), which incorporates clinical and specific genetic features, and gene expression profiling. While 15 of those patients can now be identified as high risk by IMS/IMWG criteria alone, the addition of gene expression profiling increases identification to 23 out of 25. These data highlight the potential utility of routine gene expression profiling at diagnosis to better refine risk categorization.
MYELOID NEOPLASIA
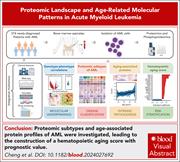
Proteomic subtypes enrich current acute myeloid leukemia nomenclature and reflect intrinsic pathogenesis alongside aging
Classification systems for acute myeloid leukemia (AML) currently integrate morphology, immunophenotype, and genomic features. Cheng et al sought to further inform biology-based classification by integrating genomic, transcriptomic, proteomic, and phosphoproteomic data from 374 patients with newly diagnosed AML. They identified a protein signature of hematopoietic aging that can be used in future studies to understand why AML is so deadly in older patients and to stratify patients by disease severity.
Improved diagnostic screening and classification of clonal mast cell diseases by ultrasensitive KIT p.D816V detection
Detection of the KIT p.D816V mutation is pivotal to the diagnosis of clonal mast cell disorders such as systemic mastocytosis, where clonality is proven in 90% of patients, and mast cell activation syndrome (MCAS), where evidence of clonality is lacking in many cases. Using a novel molecular assay, Flow-SuperRCA, Navarro-Navarro and colleagues demonstrate that increasing analytical sensitivity can reveal previously unrecognized clonal disease in subsets of patients with MCAS, supporting the integration of highly sensitive tools into diagnostic workups.
TRANSPLANTATION
Pretransplant targeting of TNFRSF25 and CD25 stimulates recipient Tregs in target tissues, ameliorating GVHD post-HSCT
Adoptive regulatory T-cell (Treg) transfer has shown promise in preclinical models and clinical trials for graft-versus-host disease (GVHD) prevention and treatment, but feasibility has proven a challenge. McManus et al demonstrate that in vivo expansion of Tregs in recipients prior to transplant is possible by activating TNFRSF25 (also known as death receptor 3) in combination with low-dose interleukin-2 in preclinical models. These tissue-resident Tregs become activated and are immunosuppressive, ameliorating GVHD while preserving graft-versus-leukemia activity. Their data suggests clinically amenable ways to better reduce the risk of GVHD.
BLOOD WORK
ERRATUM
-
Cover Image
Cover Image
![issue cover]()
Acute colonic graft-versus-host disease is characterized by the infiltration of CD4 (green) and CD8 (yellow/pink) lymphocytes, which interact with CD11c antigen-presenting cells (red) in close proximity to colonic villi enterocytes (orange cytoplasm and blue nuclei). See the article by McManus et al on page 2710.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals


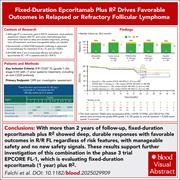


Better together: epcoritamab boosts R2 in FL
Clinical Trials & Observations