Abstract
Background: The combination of tyrosine kinase inhibitors (TKIs) with chemotherapy is highly effective in Philadelphia chromosome positive (Ph+) acute lymphoblastic leukemia (ALL). Ponatinib is a more potent BCR-ABL inhibitor, and is effective against the T315I clone which commonly causes disease recurrences. The combination of hyper-CVAD with ponatinib may produce better response rates and higher likelihood of eradication of minimal residual disease (MRD) as compared to that reported with other TKIs.
Methods: Patients with newly diagnosed Ph+ ALL received 8 cycles of hyper-CVAD alternating with high dose methotrexate and cytarabine every 21 days. Ponatinib was given at 45 mg po daily for the first 14 days of cycle 1 then continuously for the subsequent 7 cycles. Patients in complete response (CR) received maintenance with ponatinib 45 mg daily and vincristine and prednisone monthly for 2 years followed by ponatinib indefinitely. After an increased incidence of vascular toxicities was recognized, patients were offered the option to switch TKIs or to continue with a reduced dose of ponatinib of 30 mg with further decrease to 15 mg in patients in CMR. The evaluation of MRD status was performed by multicolor flow cytometry (FCM), and reverse transcription polymerase chain reaction (RT-PCR). The objective of this study is to evaluate response rates, CR duration, and overall survival (OS), and to assess the safety of this regimen. Rituximab and intrathecal chemotherapy were given for the first 4 courses.
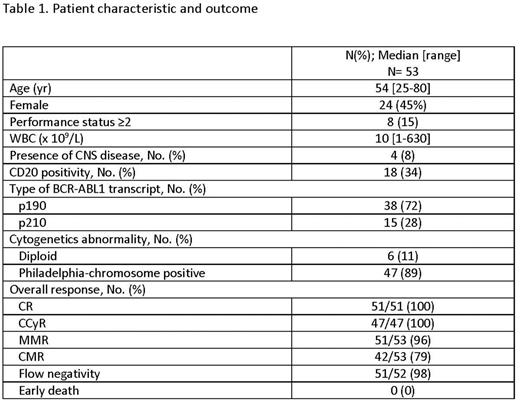
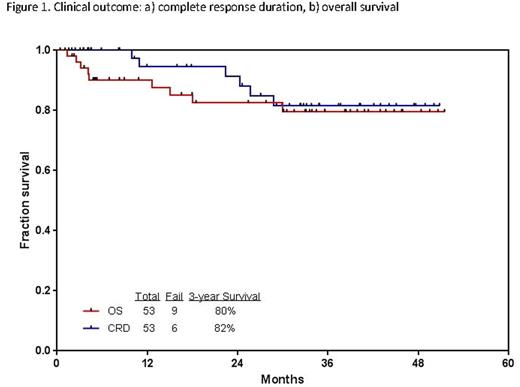
Results: To date, 53 patients with untreated Ph+ ALL and 4 patients previously treated (2 patients in CR; 2 patients not in CR) have received a median of 6 cycles (2-8); 11 patients are receiving maintenance in CR; 10 patients underwent allogeneic stem cell transplantation (ASCT) after a median of 4 cycles. Baseline patient characteristics and outcomes are described in table 1. The overall complete cytogenetic response (CCyR), major molecular response (MMR), and complete molecular response (CMR) rates were 100%, 96%, and 79%, respectively. The median time to MMR and CMR were 3 weeks (range, 2-14) and 11 weeks (range, 2- 96), respectively. The median time to MRD negativity by 6-color flow cytometry (FCM) was 3 weeks (range, 3-14). Median time to platelet and neutrophil recovery for cycle 1 was 22 days (range, 17-35) and 18 days (range, 13-29), respectively, and 22 days (range, 0-35) and 16 days (range, 0-28) for subsequent cycles. Grade ≥ 3 toxicity included infections during induction (47%), increased liver function tests (34%), thrombotic events (8%), myocardial infarction (6%), hypertension (15%), skin rash (15%), and pancreatitis (19%). With a median follow up of 33 months (range, 2-51), 44 81(%) patients remain alive and in CR (41 in CR1, and 3 in CR2). Six patients died in CR: 1 patient died in CR from an unrelated cardiac event 4 months after being taken off therapy and placed on imatinib, 1 from multiple organ failure due to sepsis (C2D13), 1 from non-ST elevation myocardial infarction (C2D41; ponatinib 45 mg daily), 1 from potential myocardial infarction (C4D42; ponatinib 30 mg daily), 1 from head injury after a fall (C4D13), and 1 from sepsis post allogeneic stem cell transplantation. Of 44 patients alive at the last follow-up, 20 (46%) patients remained on ponatinib (15 mg daily in 15, and 30 mg daily in 5), 12 (27%) switched to another TKI (9 to dasatinib, 2 to nilotinib, and 1 to imatinib), 8 (18%) underwent ASCT, 3 (7%) relapsed, and 1 (2%) had positive MRD by FCM and RT-PCR. No further vascular events were observed in patients receiving lower doses of ponatinib. The 3-year CR duration and OS rates are 82% and 80%, respectively (Figures 1). Of 10 patients who underwent ASCT while in first CR, 8 patients are alive in CR, 1 died of sepsis in CR, and 1 relapsed and died of disease progression. Landmark analysis at 4 months by ASCT showed no difference in 3-year CR duration (no ASCT, 79%; ASCT, 88%; p=0.48), and 3-year OS (no ASCT, 92%; ASCT, 79%; p=0.31).
Conclusion: The combination of hyperCVAD with ponatinib is highly effective in patients with Ph+ ALL. Due to the vascular events observed, the ponatinib dose was modified to 30 mg daily during consolidation with subsequent reduction to 15 mg in patients in CMR without further episode of cardiovascular events.
Jabbour:ARIAD: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Novartis: Research Funding; BMS: Consultancy. Pemmaraju:incyte: Consultancy, Honoraria, Research Funding; novartis: Consultancy, Honoraria, Research Funding; LFB: Consultancy, Honoraria; stemline: Consultancy, Honoraria, Research Funding; cellectis: Consultancy, Research Funding; affymetrix: Research Funding. DiNardo:Celgene: Research Funding; Agios: Other: advisory board, Research Funding; Abbvie: Research Funding; Daiichi Sankyo: Other: advisory board, Research Funding; Novartis: Other: advisory board, Research Funding. Konopleva:Cellectis: Research Funding; Calithera: Research Funding. Jain:BMS: Research Funding; Celgene: Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; ADC Therapeutics: Consultancy, Honoraria, Research Funding; Incyte: Research Funding; Novimmune: Consultancy, Honoraria; Servier: Consultancy, Honoraria; Pharmacyclics: Consultancy, Honoraria, Research Funding; Abbvie: Research Funding; Infinity: Research Funding; Novartis: Consultancy, Honoraria; Genentech: Research Funding; Seattle Genetics: Research Funding. Wierda:Novartis: Research Funding; Abbvie: Research Funding; Acerta: Research Funding; Gilead: Research Funding; Genentech: Research Funding. Cortes:ARIAD: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Teva: Research Funding. O'Brien:Pharmacyclics, LLC, an AbbVie Company: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal