Abstract
Arterial occlusive disorders are a leading cause of human morbidity. We hypothesized that ectopic expression of fibrinolytic proteins in platelets could be used to favorably alter the hemostatic balance at sites of thrombosis. To test our hypothesis, we directed murine urokinase-type plasminogen activator transgene expression to platelets using a platelet factor 4 promoter. Urokinase was selectively expressed and stored in the platelets of these mice. These transgenic mice had altered platelet biology and a bleeding diathesis similar to that seen in patients with Quebec platelet disorder, affirming the role of ectopic urokinase expression as the etiology of this inherited disease. These mice were resistant to the development of occlusive carotid artery thrombosis in the absence of systemic fibrinolysis and displayed rapid resolution of pulmonary emboli. Moreover, transfusion of urokinase-expressing platelets into wild-type mice prevented formation of occlusive arterial thrombi. These studies show the feasibility of delivering fibrinolytic agents to sites of incipient thrombus formation through selective storage in platelets and offer a new strategy to prevent thrombosis and hemorrhage.
Introduction
Thrombus formation is a complex, multistep, and highly regulated process. Platelets contribute to this process by adhering to sites of vascular injury, where they are activated and form aggregates that provide a provisional seal. Platelets contribute to the subsequent growth and stability of thrombi in part through the release of von Willebrand factor (VWF), fibrinogen, and other coagulation proteins such as factor V1 from their α-granules. Activated platelets also release proteins that inhibit thrombolysis, chief among which is plasminogen activator inhibitor-1 (PAI-1). More than 90% of the circulating PAI-1 is stored in platelet α-granules,2 although much of this is in an inactive form.2-4 Nonetheless, this pool of PAI-1 is thought to be one of the main reasons why platelet-rich thrombi are especially resistant to thrombolytic therapy.5,6
Paradoxically, platelets also contain small amounts of profibrinolytic proteins, including urokinase-type plasminogen activator (u-PA) and plasminogen.6-9 However, these proteins are found at very low levels, and their activity is overwhelmed by the large amounts of PAI-1. Recently, the effect of changing this balance in platelet fibrinolytic proteins has been described. The etiology of Quebec Platelet Disorder (QPD) has been ascribed to ectopic expression of an excess of u-PA in megakaryocytes and platelets.10 QPD is a rare bleeding disorder not responsive to platelet transfusion but responsive to antifibrinolytic agents, such as tranexamic acid.11-13 QPD platelets contain predominantly activated 2-chain urokinase (tcu-PA). The etiology for the bleeding diathesis is not clear, but the process may in part be due to local release of activated u-PA within thrombi leading to premature lysis. However, degradation of multiple platelet α-granular proteins, including VWF and factor V, presumably by plasmin generated as a result of urokinase, may interfere with thrombus development as well.
We have been interested in modulating the biologic behavior of platelets by ectopically expressing proteins of interest inside platelets. Our initial goal was to see if ectopically expressed proteins carrying a signal peptide would be stored within platelets and released specifically at sites of injury. Second, we were interested in the potential use of this approach to alter the prothrombotic role of platelets as a means to modify pathologic thrombus development. To do so, we chose to express u-PA transgenically in mice to see whether we could tip the hemostatic balance locally without causing systemic fibinolysis and bleeding characteristic of transgenic overexpression of u-PA in the liver.14 The recent description of the role of platelet u-PA in QPD provided support for this strategy. We found that the resultant transgenic animals do indeed express u-PA in their platelets in the absence of systemic fibrinolysis. These animals have a characteristic bleeding diathesis that is predominantly at the time of parturition and that can be controlled by tranexamic acid. This animal model supports the hypothesis that ectopic expression of u-PA in platelets is the etiology of QPD. These mice were found to be resistant to forming occlusive carotid arterial thrombi and rapidly lysed pulmonary venous thrombi. In addition, transfusion of small numbers of u-PA–expressing platelets into wild-type recipients prevented the formation of stable, occlusive carotid arterial thrombi. Thus, these animals provide new insights into the contribution of activated platelets to thrombus stability and offer a potential new strategy to prevent inopportune thrombus development.
Materials and methods
Vector construct and characterization of transgenic mice
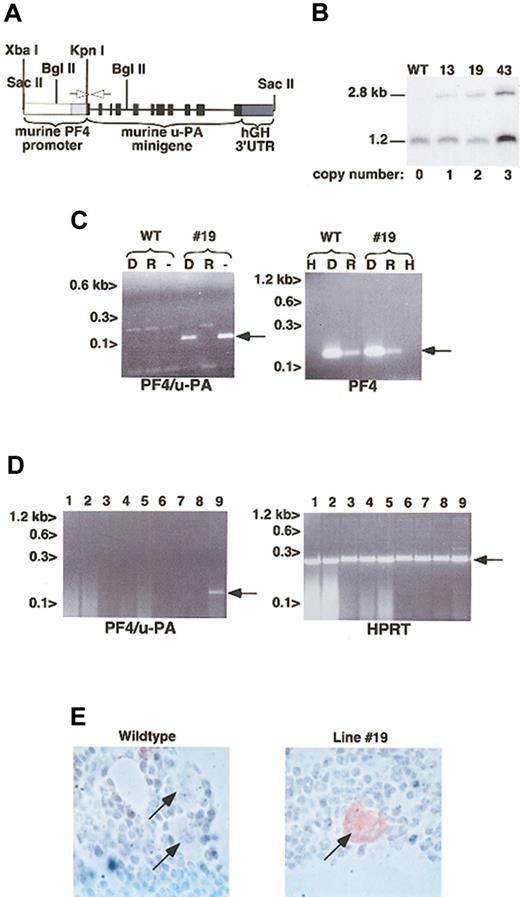
A total of 1.2 kb of the 129 SV murine platelet factor 4 (PF4) proximal promoter region plus its 5′-untranslated region (5′-UTR)15 was polymerase chain reaction (PCR) amplified with an artificial upstream XbaI site and a downstream KpnI site added (Figure 1A). This promoter was used to replace the albumin enhancer/promoter of a murine u-PA minigene expression construct previously described that contains a 3′-UTR and polyadenylation sequence from the human growth hormone (hGH) gene.14 A 10.2-kb SacII fragment containing this final construct was used to create transgenic mice by pronuclear injections following standard methods at the University of Pennsylvania Transgenic Mice Core Facility. Genomic DNA was isolated from mouse tails using a QIAamp DNA Mini Kit (Qiagen, Valencia, CA). Positive founder lines were detected by Southern blots.16 Genomic DNA was digested with BglII and separated on a 1% (wt/vol) agarose gel. The probe used was the mouse PF4 proximal promoter from -680 to -360 bp upstream of the transcriptional start site,15 and the final probed membrane was exposed on a PhosphorImaging screen (Amersham Biosciences, Sunnyvale, CA), and the intensity of bands was quantitated. The copy number was determined by comparing the intensity of the 2.8-kb transgene PF4 band with the native genomic 1.2-kb PF4 band. Founder animals and their offspring were also characterized by genomic PCR analysis using a mouse PF4 5′-UTR 5′-CACTTAAGAGCCCTAGACCCATTTCC-3′ sense primer and a mouse u-PA exon 2 5′-CTGGGCTCTAGACAGCAGT-3′ antisense primer, which generates a 479-bp genomic and a 114-bp cDNA band.
Establishment of transgenic mice expressing u-PA in their platelets. (A) Schematic representation of the 10.2-kb Sac II insert containing the 1.2-kb murine XbaI/KpnI PF4 promoter (open box) plus 5′-UTR (light gray box) followed by the 11-exon murine u-PA gene (black boxes) and ending with the hGH 3′-UTR and polyadenylation sequence (dark gray box). The 2.8-kb Bgl II fragment detected for the transgene in the genomic Southern blot in panel B is indicated. PCR was performed to confirm founder lines using primers complementary to the mouse PF4 5′-UTR and exon 2 of the murine u-PA gene (data not shown). The same primers were used for the RT-PCR in panel C indicated as open arrows. (B) Genomic Southern blot analysis of Bgl II-digested DNA from a wild-type animal and the 3 lines that had offspring is shown. Copy number determined by phosphorimaging is indicated below. (C) RT-PCR of platelet total RNA for the 114-bp transgenic u-PA message is shown, as is the 185-bp PF4 message as a positive control of the platelet nature of the RNA. - indicates RT-PCR; D, pretreatment with RNase-free DNase prior to RT-PCR; R, pretreatment with DNase-free RNase prior to RT-PCR; H, water used instead of first-strand cDNA. Arrows point to the expected cDNA bands. (D) RT-PCR of multiple tissues. Only bone marrow showed the 114-bp transgenic u-PA band, but all samples showed the 249-bp HPRT+ control cDNA band. 1 indicates spleen; 2, liver; 3, lung; 4, heart; 5, kidney; 6, adrenal; 7, tongue; 8, brain; 9, bone marrow. Arrows point to the expected cDNA bands. (E) Immunohistochemical detection of u-PA in wild-type and line no. 19 bone marrow. Several morphologically recognizable megakaryocytes are indicated by arrows. Original magnification, × 1000; samples were stained with hematoxylin.
Establishment of transgenic mice expressing u-PA in their platelets. (A) Schematic representation of the 10.2-kb Sac II insert containing the 1.2-kb murine XbaI/KpnI PF4 promoter (open box) plus 5′-UTR (light gray box) followed by the 11-exon murine u-PA gene (black boxes) and ending with the hGH 3′-UTR and polyadenylation sequence (dark gray box). The 2.8-kb Bgl II fragment detected for the transgene in the genomic Southern blot in panel B is indicated. PCR was performed to confirm founder lines using primers complementary to the mouse PF4 5′-UTR and exon 2 of the murine u-PA gene (data not shown). The same primers were used for the RT-PCR in panel C indicated as open arrows. (B) Genomic Southern blot analysis of Bgl II-digested DNA from a wild-type animal and the 3 lines that had offspring is shown. Copy number determined by phosphorimaging is indicated below. (C) RT-PCR of platelet total RNA for the 114-bp transgenic u-PA message is shown, as is the 185-bp PF4 message as a positive control of the platelet nature of the RNA. - indicates RT-PCR; D, pretreatment with RNase-free DNase prior to RT-PCR; R, pretreatment with DNase-free RNase prior to RT-PCR; H, water used instead of first-strand cDNA. Arrows point to the expected cDNA bands. (D) RT-PCR of multiple tissues. Only bone marrow showed the 114-bp transgenic u-PA band, but all samples showed the 249-bp HPRT+ control cDNA band. 1 indicates spleen; 2, liver; 3, lung; 4, heart; 5, kidney; 6, adrenal; 7, tongue; 8, brain; 9, bone marrow. Arrows point to the expected cDNA bands. (E) Immunohistochemical detection of u-PA in wild-type and line no. 19 bone marrow. Several morphologically recognizable megakaryocytes are indicated by arrows. Original magnification, × 1000; samples were stained with hematoxylin.
All biologic studies described below were done with transgenic animals that had been backcrossed at least 4 generations onto a C57BL/6 background. Wild-type littermates served as controls. Cardiac or portal vein blood was drawn from mice into 1/10 volume of 3.8% sodium citrate. All studies were approved by the Animal Care and Use Committee of the Children's Hospital of Philadelphia.
Transgenic u-PA message detection
Murine platelet RNA was isolated using RNA STAT-60 (Tel-Test, Friendswood, TX) as previously described.15 Tissues (about 100 mg each) from these animals were collected, rinsed vigorously with saline, disaggregated in 500 μL RNA STAT-60, and RNA was isolated.15 Some platelet RNA samples were pretreated with DNase-free RNase (1 U/10 μL reaction; Sigma, St Louis, MO) or RNase-free DNase (1 U/10 μL reaction; Life Technologies, Gaithersburg, MD) for 1 hour at 37°C. Reverse transcription was performed using the SuperScript II Reverse Transcriptase Kit (Life Technologies). PCR amplification of the transgenic u-PA cDNA was accomplished using the 2 primers discussed above. Platelet-specific control reverse transcriptase (RT)–PCR primers for PF4 message were sense 5′-GTCCAGTGGCACCCTCTTGA-3′ and antisense 5′-AATTGACATTTAGGCAGCTGA-3,17 with an expected cDNA product of 185 bp. RT-PCR for the housekeeping gene human phosphoribosyltransferase (HPRT) used primers 5′-GCTGGTGAAAAGGACCTCT-3′ and 5′-CACAGGACTAGAACACCTGC-3′, with an expected cDNA product of 249 bp.18 Platelet murine transgenic u-PA cDNA band was isolated using a QIAkwik Gel Extraction Kit (Qiagen) and directly sequenced using an ABI 373A automated sequencer (ABI Instruments, Foster City, CA).
Immunohistochemical staining for murine urokinase
Spleen and bone marrow aspirates from wild-type and murine u-PA transgenic mice were stained for murine u-PA expression using a mouse monoclonal antimurine u-PA antibody (A10, Molecular Innovations, Southfield, MI) as the primary antibody and a biotinylated antimouse immunoglobulin (ARK detections system, DAKO, Carpinteria, CA) as the secondary antibody. Specifically, formalin-fixed, paraffin-embedded 5-μm sections were deparaffinized in xylene and rehydrated. Endogenous peroxidase activity was quenched with 0.9% peroxide in methanol for 20 minutes. Slides were then treated with trypsin (1 mg/mL in phosphate-buffered saline [PBS]) for 10 minutes at 37°C. After incubation with the monoclonal antimurine u-PA antibody (0.5 μg/mL) and then with biotinylated ARK reagent for 15 minutes at room temperature, the slides were stained at room temperature for 2 hours. Slides were washed and incubated with Streptavidin-HRP (DAKO) for 15 minutes at room temperature. Slides were again washed, and DAB reagent (DAKO) was applied for 5 minutes at room temperature. Slides were counterstained with dilute (1:10) hematoxylin for 30 seconds.
Zymogram and immunoblot studies
Platelet-rich plasma (PRP) was obtained as previously described.15 Platelet counts were determined using a HemaVet counter (Triad Associates, Concord, CA). The platelets were pelleted at 800g for 5 minutes and resuspended immediately in 1 × NuPage Sample Buffer (Invitrogen, Carlsbad, CA). For zymography, samples (0.5 to 10 μg per lane) were size fractionated under nonreducing conditions using a 12% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) containing 0.4% nonfat dry milk (Carnation Instant Skim Milk Powder, Nestle, Fulton, NY), with or without addition of 20 μg/mL human plasminogen (American Diagnostica, Greenwich, CT), and then renatured with 0.5% Triton X-100 in PBS, pH 7.4, for 1 hour.14 The gel was incubated at 37°C for 3 hours. A control lane containing 0.1 ng human 2-chain urokinase (American Diagnostica) was included in each gel.
Platelet samples were prepared as above, and immunoblots were performed as previously described,15 except that 4% to 8% gradient gels were used (NuPAGE Novex Bis-Tris Gels, Invitrogen). Gels were run under nonreducing conditions, except when studying platelet fibrinogen, where 1 μL of reducing agent (NuPAGE Sample Reducing Agent) was added per sample. Mouse u-PA was detected with A10 added at a 1:75 dilution and detected with a biotinylated antimouse monoclonal antibody followed by peroxidase-conjugated streptavidin (StreptABComplex/HRP, DAKO). Murine VWF was detected using a 1:200 dilution of a horseradish peroxidase (HRP)–conjugated rabbit antihuman VWF polyclonal antibody (DAKO), and murine fibrinogen was detected using a 1:100 dilution of an HRP-conjugated goat antihuman fibrinogen polyclonal antibody (Rockland Immunochemicals, Gilbertsville, PA). To study the in vitro digestion of factor V by platelet lysates in Nupage LDS Sample Buffer (Invitrogen), 10 ng plasma-derived human factor V was digested with either human tcu-PA (10 pg; American Diagnostica) or with 2.5 μg total murine platelet lysate prepared from 1.3 × 106/μL platelets in the presence or absence of plasminogen (1 μg). The platelet lysate was prepared by resuspending the platelets in 10 μL water and adding 1 μL 10% Triton X-100. The resultant digest was then separated by SDS-PAGE. Factor V was detected using a 1:100 dilution of an HRP-conjugated sheep antihuman factor V polyclonal antibody (Affinity Biologicals, Hamilton, ON, Canada) as the primary antibody.
Hematologic studies
Blood counts were measured using a Hemavet 850 (CDC Technologies, Oxford, CT) calibrated for murine blood. Dried blood smears were stained using Wright-Giemsa reagent, and the red cell and platelet morphology was examined. Fibrin D-dimers were measured in plasma samples obtained according to manufacturer's instructions (Asserachrom D-Di, American Bioproducts, Diagnostica Stago, Asnieres, France) using the enclosed human D-dimer control. Platelet aggregation studies were performed as described previously.19 Aggregation and dense granule adenosine triphosphate (ATP) release were measured in a lumiaggregometer (Chrono-Log, Havertown, PA). Agonists studied included collagen (1-5 μg/mL), adenosine diphosphate (ADP) (1-5 μM), epinephrine (50 μM), and thrombin (0.1-1 U/mL) (Bachem, Torrance, CA). Marrow samples from wild-type and transgenic mice were stained for mouse u-PA expression using the murine antimouse u-PA A10 primary antibody as described previously.15 Bleeding times were done as previously described.20
Carotid artery thrombi
FeCl3-induced arterial injury was performed in 6- to 8-week-old animals.6,21 The right common carotid artery was exposed by blunt dissection, and a miniature Doppler flow probe (Model 0.5VB; Transonic Systems, Ithaca, NY) was positioned around the artery. A 1 × 2–mm2 strip of No. 1 Whatman filter paper (Fisher Scientific, Pittsburgh, PA) soaked in 10% FeCl3 was then applied to the adventitial surface of the artery for 2 minutes. The field was flushed with saline, and blood flow was monitored for 30 minutes. The time to initial complete occlusion and the presence or absence of arterial occlusion at 30 minutes was recorded.
To study the effects of platelet transfusion, 1.2 × 108 to 1.5 × 108 gel-filtered platelets in 300 μL gel-filtering buffer (4 mM NaH2PO4, 5 mM HEPES [N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid], 137 mM NaCl, 2.6 mM KCl, 5 mM glucose, 1 mM MgCl2) were prepared as previously described19 and infused into the left jugular vein immediately before the FeCl3 patch was applied. Platelets were used within 2 hours of collection. Total blood counts were measured immediately before and 2 minutes after platelet infusion.
Pulmonary microemboli model
125I-labeled human microemboli, 1.5 to 3.5 μm3 in size, were prepared.22 Transgenic and wild-type animals were injected with these particles. At various time points (2 to 60 minutes) the animals were humanely killed, the lungs removed, washed free of blood, and the amount of 125I activity measured using a ZM Coulter Counter (Coulter Electronics, Hialeah, FL). Autoradiograms of lungs from wild-type and transgenic mice 30 minutes after injection of the microemboli were performed by exposing the tissues to X-OMAT film (Kodak, Rochester, NY).
Results
Establishment of transgenic mice expressing u-PA message
The rat PF4 proximal promoter was the first promoter used to drive megakaryocyte-specific expression of a reporter gene LacZ in transgenic mice.23 Based on this knowledge, we placed a homologous 1.2-kb region of the mouse PF4 proximal promoter, which also drives megakaryocyte-specific expression of LacZ in transgenic mice (data not shown), immediately upstream of a mouse u-PA minigene with a hGH 3′-UTR14 (Figure 1A). Seven transgenic founders were obtained with copy numbers ranging from 1 to more than 20 copies per haploid genome. Figure 1B shows a genomic Southern blot of the 3 lines with the fewest copy numbers of the transgene—nos. 13, 19, and 49—and the transgene copy number per haploid genome. These 3 male founders had offspring (Figure 1B), although the line no. 49 transgene did not transmit well (see “Clinical course and hematologic studies”), and therefore these mice were not available for most studies. All 3 female founders had high transgene copy number and, when pregnant, died peripartum from uterine hemorrhage (see “Clinical course and hematologic studies”). The final male founder had a high copy number (more than 20) and never produced offspring. By RT-PCR analysis of total platelet RNA, line nos. 13, 19, and 49 expressed a transgenic u-PA message in their platelets as shown in Figure 1C for line no. 19. Direct sequence analysis of this RT-PCR product for all 3 lines confirmed that the first intron was appropriately spliced out (data not shown). Aside from the marrow, no other tissue tested was positive for transgenic-derived u-PA mRNA (Figure 1D). Immunohistochemistry of the bone marrow showed detectable u-PA only in morphologically recognizable megakaryocytes in the transgenic animals but not in wild-type marrow (Figure 1E).
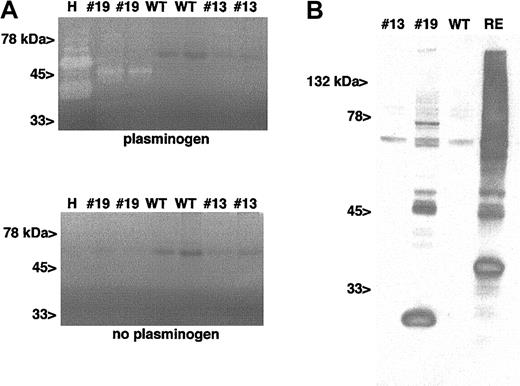
u-PA activity in the platelets
We then examined whether these animals expressed u-PA in their platelets. Total platelet protein was separated on a nonreducing gel containing casein with or without supplemental plasminogen. A prominent band likely representing tcu-PA at about 45 kDa was seen with platelets from line no. 19 (Figure 2A, top), similar to what has been previously described for murine u-PA and consistent with the fact that mouse u-PA is not glycosylated.14 Line no. 13 and wild-type lanes had no detectable zones of lysis, although twice as much platelet protein was loaded compared with the no. 19 line lanes. Omission of plasminogen from the zymogram (Figure 2A, bottom) or the inclusion of the selective u-PA inhibitor amiloride in the zymogram (data not shown) abolished lysis induced by transgenic platelet lysates and the human tcu-PA control. These results are similar to those reported for QPD platelets.10
Detection of u-PA activity and antigen in line no. 19 platelet lysate. (A) Zymogram of 2 separate preparations of lysates from line no. 19 and no. 13 platelets and wild-type platelets in a gel containing (top) or lacking (bottom) 20 μg/mL plasminogen. H indicates human tcu-PA (0.1 ng). From left to right, the platelet lanes had the following amounts of protein added: no. 19, 0.5 μg; no. 19, 0.1 μg; WT, 1 μg; WT, 2 μg, no. 13, 1 μg; and no. 13, 2 μg. (B) Nonreduced Western blot of platelet lysates (10 μg per lane) for line no. 19 and no. 13, wild type, and renal extract (RE) (30 μg per lane) immunoblotted with A10.
Detection of u-PA activity and antigen in line no. 19 platelet lysate. (A) Zymogram of 2 separate preparations of lysates from line no. 19 and no. 13 platelets and wild-type platelets in a gel containing (top) or lacking (bottom) 20 μg/mL plasminogen. H indicates human tcu-PA (0.1 ng). From left to right, the platelet lanes had the following amounts of protein added: no. 19, 0.5 μg; no. 19, 0.1 μg; WT, 1 μg; WT, 2 μg, no. 13, 1 μg; and no. 13, 2 μg. (B) Nonreduced Western blot of platelet lysates (10 μg per lane) for line no. 19 and no. 13, wild type, and renal extract (RE) (30 μg per lane) immunoblotted with A10.
To confirm the presence of u-PA in the transgenic platelets, total platelet proteins were separated by size on a nonreducing gel and then immunoblotted with A10, an antimurine u-PA monoclonal antibody (mAb). A major doublet was seen at about 45 kDa in line no. 19 total platelet lysate that comigrates with a band in the renal extract (RE) control, consistent with tcu-PA. This band was not seen in platelet lysates from wild-type littermates (Figure 2B). A higher, less intense band, consistent with either single-chain uPA (scu-PA) or an otherwise modified tcu-PA as previously described,24 was also seen, which migrates similar to a band in renal extract (RE). Thus, as with QPD platelet lysates, the major form of u-PA in the transgenic platelets appears to be tcu-PA.10
Also, as with QPD platelet lysates, a few high-molecular-weight species were observed that likely include covalent complexes between PAI-1 and tcu-PA and low-molecular-weight proteolytic derivatives of u-PA.8 The typical low-molecular-weight u-PA species commonly observed in biologic specimens (about 30 kDa; see RE lane in Figure 2B) was not a feature of platelet lysates. Rather, as observed with QPD platelets, a somewhat smaller low-molecular-weight u-PA species was observed in transgenic mouse platelet lysates. None of these mouse u-PA bands were detected when a comparable amount of platelet lysate from wild-type and line no. 13 mice was studied. This lack of detectable u-PA in line no. 13 is consistent with the lack of u-PA activity seen in the zymogram (Figure 2A) and in the clinical course of these animals (see below).
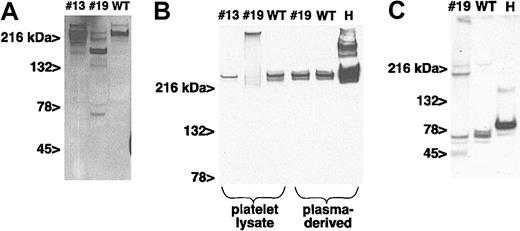
α-Granular proteins
Several α-granular proteins, including VWF, fibrinogen, and factor V, undergo proteolysis in QPD platelets due to the ectopically expressed u-PA.10 We tested whether the presence of mouse u-PA in platelets led to a similar expression of proteolytic activity. As seen in Figure 3A, VWF underwent extensive digestion in the line no. 19 platelets, compared with the intact high-molecular-weight VWF seen in the littermate wild-type sample. Consistent with the immunoblot for mouse u-PA, no degradation of VWF was seen in platelets from line no. 13 mice.
α-Granular protein digestion. (A) Western blot of platelet lysate (2.5 μg per lane) from line no. 13 and no. 19 and wild-type mice immunoblotted with a rabbit antihuman VWF polyclonal antibody. (B) Western blot of nonreduced gel of platelet lysates as above or plasma (3 μg per lane for mouse and 6 μg per lane for human) proteins. H indicates human plasma preparation. Murine and human fibrinogen were detected using a goat antihuman fibrinogen polyclonal antibody. (C) Same as panel B except that the samples were only of platelet lysates and the gel was performed under reducing conditions.
α-Granular protein digestion. (A) Western blot of platelet lysate (2.5 μg per lane) from line no. 13 and no. 19 and wild-type mice immunoblotted with a rabbit antihuman VWF polyclonal antibody. (B) Western blot of nonreduced gel of platelet lysates as above or plasma (3 μg per lane for mouse and 6 μg per lane for human) proteins. H indicates human plasma preparation. Murine and human fibrinogen were detected using a goat antihuman fibrinogen polyclonal antibody. (C) Same as panel B except that the samples were only of platelet lysates and the gel was performed under reducing conditions.
Platelet α-granular fibrinogen was also degraded in transgenic line no. 19, but not in line no. 13 or in wild-type platelets, as assessed on a nonreducing SDS-PAGE gel (Figure 3B). In contrast, plasma fibrinogen was not degraded in line no. 19 mice. This finding clearly contrasts with the systemic fibrinolysis that develops in the previously described u-PA–overexpressing transgenic mice that were generated using a liver-specific promoter.14 Platelet fibrinogen immunoblots of line no. 19 lysate consistently contained high-molecular-weight complexes that entered the gel poorly (Figure 3B). These high-molecular-weight complexes were absent on a reduced gel (Figure 3C), suggesting that they represent disulfide-bonded, cross-linked, fibrinogen-derived products generated by u-PA and plasmin.
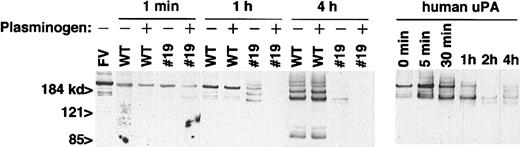
We also tested whether total platelet lysates from the transgenic mice could proteolyze human factor V in a manner similar to that seen in QPD. Platelet lysates were incubated with human factor V for up to 4 hours (Figure 4). Platelet lysates from line no. 19 mice digested factor V rapidly, with degradation nearly complete by 4 hours, similar to that seen with exogenously added human u-PA. Platelets from wild-type littermates also degraded factor V but at a much slower rate. The addition of exogenous plasminogen to the total platelet lysate enhanced factor V digestion by line no. 19 but had little effect on the rate of digestion by wild-type platelets. This would suggest that the amount of plasminogen available in α-granules in the transgenic line no. 19 platelets is rate limiting for maximal protein degradation.
In vitro degradation of factor V by platelet lysate. Factor V (FV) (10 ng per lane) was digested with 2.5 μg per lane of the indicated platelet lysate or human u-PA (5 μg per lane) for the indicated amount of time at room temperature. + indicates plasminogen (1 μg per lane) added; –, no added plasminogen.
In vitro degradation of factor V by platelet lysate. Factor V (FV) (10 ng per lane) was digested with 2.5 μg per lane of the indicated platelet lysate or human u-PA (5 μg per lane) for the indicated amount of time at room temperature. + indicates plasminogen (1 μg per lane) added; –, no added plasminogen.
Clinical course and hematologic studies
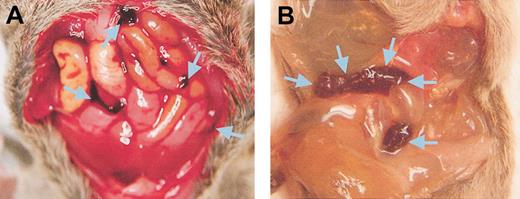
Fewer line no. 19 and no. 49 transgenic mice were born than expected. Assuming that 50% of the offspring from a cross between a hemizygous animal and a wild-type animal should be transgenic, line no. 19 showed a 68% mortality rate (57 transgenic animals versus 175 wild-type littermates at weaning) and line no. 49 showed an 85% mortality rate (2 transgenic and 12 wild type). Line no. 13 had a very low mortality rate, consistent with little platelet u-PA expression (71 transgenic and 80 wild type). At day 16.5 of gestation, line no. 19 embryos looked normal and appeared at the expected frequency (10 transgenic and 11 wild type), indicating that transgenic animals were lost peripartum. Surviving transgenic animals were normal for weight and growth, although occasional spontaneous deaths occurred among the adults secondary to subcutaneous or internal hemorrhage. Shown are autopsies on 2 such adult line no. 19 animals, 1 with free blood in the opened peritoneum (Figure 5A) and the other with free blood filling a small intestinal loop (Figure 5B). However, when 10 line no. 19 animals and 10 littermate wild-type controls were specifically observed for more than 1 year, no deaths were observed in either group, suggesting a low rate of death in the line no. 19 animals.
Examples of spontaneous hemorrhage in mice expressing u-PA in their platelets. (A) Mouse with peritoneal lining opened showing free blood in the peritoneal space indicated by arrows. (B) Mouse with a loop of small bowel filled with free blood indicated by arrows.
Examples of spontaneous hemorrhage in mice expressing u-PA in their platelets. (A) Mouse with peritoneal lining opened showing free blood in the peritoneal space indicated by arrows. (B) Mouse with a loop of small bowel filled with free blood indicated by arrows.
As noted above, none of the female founder lines survived birthing. This was also true for pregnant line no. 19 and no. 43 transgenic females. In line no. 19, none of 9 pregnant females survived giving birth, exsanguinating from uterine bleeding peripartum (data not shown). Litter sizes were normal, with embryos containing equal numbers of wild-type and transgenic animals, and all embryos appeared normal in size (data not shown). Three pregnant line no. 19 females were given tranexamic acid (20 mg/mL), an inhibitor of plasminogen activation, in their drinking water25 during the last week of pregnancy and all survived. One lost her pups at birth, and the other 2 had small litters consisting of 3 pups each (2 of these 6 were transgenic).
Complete blood counts performed on line no. 19 adult mice and wild-type littermate controls (n = 10 each) showed nearly identical platelet counts and hemoglobin levels (data not shown). Peripheral blood smears were normal, including normal platelet numbers and appearance and no evidence of red cell schistocytes or spherocytes (data not shown). Platelet aggregation and ATP release in response to collagen (1-5 μg/mL), ADP (1-5 μM), epinephrine (50 μM), and thrombin (0.1-1 U/mL) were also normal (data not shown). D-dimer measurements were not detected in the line no. 19 mice (data not shown). Together with the measurements of plasma fibrinogen (Figure 3B), these studies confirm that line no. 19 mice do not have systemic fibrinolysis.
Carotid artery thrombosis model
Tail bleeding times were normal in line no. 19 mice when compared with wild-type littermate controls (5.8 ± 3.2 versus 5.1 ± 3.4 minutes [n = 7 each], respectively), but this test has previously proven to be an insensitive measurement of thrombotic tendency.26 We therefore employed a FeCl3 carotid artery injury thrombosis model that has been used successfully to demonstrate a bleeding diathesis in diverse mouse backgrounds.6,21 This approach also enabled us to study the effect of ectopic expression of u-PA in platelets on thrombus development and stability.
Unlike wild-type littermates and line no. 13 mice, few transgenic animals expressing platelet u-PA formed complete occlusive coronary artery thrombi after FeCl3-induced injury (Table 1), and those that occluded tended to reopen rapidly. At 30 minutes, only 5% of occlusive thrombi formed in the u-PA mice remained, as opposed to the more than 85% of thrombi in controls (Table 1). Supplementing the transgenic animals in their drinking water with 20 mg/mL of tranexamic acid reversed this protection from occlusive coronary artery thrombosis.
Pulmonary microemboli model
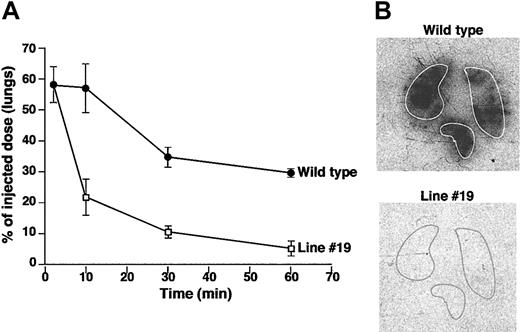
We then asked whether the u-PA–containing platelets are also effective on the venous side of the circulation and would lead to rapid dissolution of pulmonary microemboli. We had previously shown that the lysis of 125I-labeled fibrin microparticles depends on u-PA as an intravenous infusion of u-PA into u-PAnull mice normalized the rate of fibrinolysis.22 We wondered whether u-PA–containing platelets would similarly enhance fibrin clot breakdown. As shown in Figure 6, fibrinolysis was dramatically accelerated in line no. 19 compared with wild-type mice. Differences were already evident at 2 minutes. By 10 minutes, at a time when there was minimal fibrinolysis in wild-type mice, more than 80% of the clot burden had already been cleared from the lungs of line no. 19 mice.
Pulmonary microemboli lysis study. (A) Solid circles show residual labeled microemboli remaining in the lungs of wild-type mice at the indicated times (n = 6). Open squares show the residual radioactivity in the lungs of line no. 19 mice studied in parallel (n = 6). Mean ± 1 SD is shown. (B) Representative autoradiograph of whole lung at the 30-minute time point. The animal genotype and the outline of the lungs are indicated.
Pulmonary microemboli lysis study. (A) Solid circles show residual labeled microemboli remaining in the lungs of wild-type mice at the indicated times (n = 6). Open squares show the residual radioactivity in the lungs of line no. 19 mice studied in parallel (n = 6). Mean ± 1 SD is shown. (B) Representative autoradiograph of whole lung at the 30-minute time point. The animal genotype and the outline of the lungs are indicated.
Platelet transfusion/carotid artery studies
Based on these studies, which showed that platelet-expressed u-PA both prevented untoward arterial thrombosis and accelerated lysis of venous emboli, we wondered whether transfusion of u-PA–containing platelets would interfere with thrombus development and stability in wild-type animals. Platelet transfusions equivalent to about 10% of the total circulating platelets in an animal were given from line no. 19 animals to wild-type littermate controls prior to exposing the carotid artery to an FeCl3 injury. Wild-type animals that received u-PA–containing platelets were protected against the development of thrombosis to the same extent as line no. 19 mice (Table 2). Transfusion of buffer alone or wild-type platelets into wild-type mice did not prevent the development of occlusive thrombi. As anticipated from the above data, giving wild-type platelets to line no. 19 mice did not confer resistance to arterial thrombosis.
To test whether protection from thrombosis seen in wild-type animals receiving line no. 19 platelets was attributable to the released u-PA or to the released degraded α-granular proteins, wild-type animals were placed on drinking water containing tranexamic acid. A week later, carotid artery injury was performed on these wild-type mice after they had received an infusion of platelets from the line no. 19 animals. It was anticipated that platelet-associated plasminogen activation would be inhibited in tranexamic acid–treated recipients, leading to loss of protection from thrombosis if released u-PA is the primary mechanism by which line no. 19 platelets interfere with normal thrombus development. As hypothesized, recipient wild-type animals on tranexamic acid lost their resistance to arterial occlusion notwithstanding transfusion of transgenic platelets, suggesting that the released u-PA contributes significantly to the observed antithrombotic effect. The converse experiment, infusing platelets from a line no. 19 animal that had been on tranexamic acid for 1 week to wild-type littermates, showed that the infused platelets conferred resistance to arterial thrombosis. This would also support the conclusion that line no. 19 platelets interfere with thrombosis in wild-type animals primarily because ectopically expressed u-PA is released from the infused platelets.
Discussion
Platelets target to sites of vascular injury where they preferentially release their granular contents. We have been interested in determining whether developing megakaryocytes could be altered to express either antithrombotic or prohemostatic proteins, which would be stored in platelet granules and be released in a concentrated fashion directly at a site of injury. As a test of principle, we directed the expression of u-PA to platelets of transgenic mice using a megakaryocyte-specific PF4 promoter. We hypothesized that platelet u-PA would be stored in platelets and might be released within developing thrombi when platelets were activated. The u-PA would be partially counterbalanced by PAI-1, which is present in platelet α-granules of both human and mice platelets.27 However, we hoped this approach would tip the balance sufficiently to lessen the resistance of clots to commonly employed fibrinolytic agents.
Our studies show that uPA can be expressed and stored inside of developing megakaryocytes and their progeny. Secretion of uPA from the megakaryocytes and platelets into the plasma was undetectable, indicating that the protein was indeed preferentially stored in the circulating platelets, where it led to the digestion of α-granular proteins. However, this observation leaves several important questions unanswered. First, the mechanism by which u-PA is retained in the platelet and leads to α-granule digestion is unknown. Murine platelets express urokinase receptors on the cell surface,28 but it is not known whether sufficient receptors are also present in the membranes of the α-granules to account for the accumulation of u-PA. Second, platelet u-PA was predominantly found to be present in the form of enzymatically active tcu-PA, as determined by immunoblotting (Figure 2B), and the mechanism by which scu-PA is activated will require additional study. We posit that platelets endocytose sufficient plasminogen from plasma9 into their α-granules to form plasmin, as suggested by the capacity of u-PA platelets to digest exogenous factor V (Figure 5). Plasmin formation may be initiated by the low level of intrinsic activity of scu-PA,7 by the activation of scu-PA by u-PAR,29 or, less likely, by another platelet granular enzyme. It is likely that plasmin, once formed, then converts additional scu-PA to tcu-PA within the granules themselves, although the role of other proteases again cannot be excluded. Third, little tcu-PA was found as high-molecular-weight complexes with PAI-1. Murine platelets may contain less PAI-1 than human platelets, or the latent state of PAI-1 within the granules30,31 may limit its binding to u-PA, or complex formation may be inhibited by u-PAR,32 the pH, or other components of the α-granules, or, more likely, most of the PAI-1 was degraded by the u-PA.
Of particular note in our studies is that these animals had little obvious bleeding outside the peripartum period; however, these animals clearly were resistant to developing occlusive thrombi in an FeCl3-induced carotid artery thrombosis model. Only a small percentage of the u-PA–expressing animals developed complete arterial occlusions. It appears that the thrombi that did form were far more friable and transitory in nature. Moreover, lysis of preformed, fibrin microemboli targeted to the lungs occurred far more rapidly in the u-PA–expressing mice than in their wild-type counterparts. These data suggest that platelet activation initiated by fibrin contributes to thrombus growth or stability on the venous side of the circulation22 and that local release of u-PA causes rapid lysis of the nascent thrombi. Recent studies using combined platelet glycoprotein IIb/IIIa inhibitors and fibrinolytic agents33 and studies using pharmacologic inhibition of PAI-134 are consistent with these conclusions.
Transfusion of u-PA platelets equivalent to 10% of the recipient's platelet mass potently inhibited thrombus development in wild-type recipients. We infer that the ability of the transgenic platelets to disrupt thrombus development is more likely due to the released u-PA than to degradation of hemostatic α-granular proteins for several reasons. First, the near total loss of granular proteins, as in the Gray Platelet Disorder, is associated with little or no bleeding.35 Second, arterial thrombi are enriched with PAI-1. The absence of PAI-1 in mice results in a failure of thrombus formation in a chemically induced carotid artery thrombosis model.36 Third, transfusion of transgenic platelets into wild-type recipients receiving tranexamic acid reversed the effect of platelet-associated u-PA on thrombus formation (Table 2), notwithstanding the persistence of degraded α-granular proteins in the transfused platelets. These results suggest that it is the u-PA that is the major cause for the defective hemostasis in these mice.
During the course of our studies, Kahr et al reported that QPD platelets contain u-PA, which they posited is responsible for the degradation of α-granular proteins.10 This disorder had been attributed previously to abnormalities in factor V37 or multimerin.12 They estimated that QPD platelets contain about 90 pg of u-PA per microgram of total platelet protein.10 Based on a similar analysis of the data shown in Figure 2A compared with the included human recombinant uPA control, we estimate that line no. 19 platelets contain about 20 pg of u-PA per microgram of total platelet protein. Certainly cross-species comparisons of uPA are difficult because the specific activities of each uPA with human plasminogen are unknown, but it appears that line no. 19 animals have within a 5-fold-difference, similar levels of platelet uPA to the human disease. Moreover, there are striking similarities between the phenotype of the QPD patients and our transgenic mice, which we believe provide additional support for the conclusion that this syndrome results from the ectopic expression of u-PA in platelets. Both are dominantly inherited disorders ectopically expressing u-PA in their platelets and with many degraded α-granular proteins. In both QPD and our mice, the ectopic expression of u-PA is essentially confined to the platelets, and insufficient u-PA is secreted into the plasma to cause systemic fibrinolysis. Neither is improved by infusion of wild-type platelets but is improved by use of an antifibrinolytic agent, such as tranexamic acid. There are also interesting differences between our animals and humans with QPD, including the prevalence of perinatal bleeding, the nature of the fibrinogen degradation products, and certain hematologic values and platelet aggregation studies. Even if it were clear that the amount of platelet-uPA in the 2 species was comparable, differences in the expression or severity of human diseases in murine models are commonly observed—for example, the lack of joint disease in murine Hemophilia A38 and the greater risk of spontaneous thrombosis in factor VLeiden mice in certain strain backgrounds.39
In summary, these studies support the proposed etiology of QPD as being due to ectopic expression of u-PA in platelets. Second, they highlight the importance of the balance between platelet-dependent coagulation and fibrinolysis during thrombus growth on venous as well as on the arterial side of the circulation. Third, they show that the ectopic expression of u-PA in platelets may be a potent way to prevent untoward thrombus development. Our transgenic model shows that it is possible to genetically alter developing megakaryocytes in such a way that platelet function is effectively tipped from prothrombotic to antithrombotic. These studies provide a proof of principle that ectopic u-PA expression in platelets can be achieved. This strategy may have clinical application in situations where rethrombosis or the prevention of extension of a previous thrombosis would be desirable for an extended time. For example, reinfusion into a patient of megakaryocyte progenitors that had been treated with a retroviral gene transfer vector driving u-PA expression may be a potent mechanism to prevent postangioplasty restenosis for several weeks to months with low risk of long-term alteration of the recipient's stem cell genome. Untoward bleeding associated with the therapy can be controlled by treatment with an antifibrinolytic agent such as tranexamic acid. Finally, this same approach has the potential to promote delivery of prohemostatic proteins to sites of vascular interruption in patients with diverse hemorrhagic disorders.
Prepublished online as Blood First Edition Paper, April 10, 2003; DOI 10.1182/blood-2003-01-0054.
Supported in part by grants from the National Heart, Lung, and Blood Institute (NHLBI) (HL54749 [M.P.], HL64190 [M.P.], HL60169 [D.B.C.], HL66442 [D.B.C.], HL47826 [J.L.D.], and HL63194 [J.L.D.]).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Katya Ravid at Boston University for providing initial mouse PF4 sequence for these studies. Plasma-derived human factor V was kindly provided by Rodney Camire at the Children's Hospital of Philadelphia.