Abstract
Alloreactive donor cytolytic T lymphocytes play a critical role in pathophysiology of acute graft-versus-host disease (GVHD). As GVHD progression involves tumor necrosis factor superfamily receptor activation, and as apoptotic signaling for some tumor necrosis factor superfamily receptors might involve acid sphingomyelinase (ASMase)–mediated ceramide generation, we hypothesized that ASMase deletion would ameliorate GVHD. Using clinically relevant mouse models of acute GVHD in which allogeneic bone marrow and T cells were transplanted into asmase+/+ and asmase−/− hosts, we identify host ASMase as critical for full-blown GVHD. Lack of host ASMase reduced the acute inflammatory phase of GVHD, attenuating cytokine storm, CD8+ T-cell proliferation/activation, and apoptosis of relevant graft-versus-host target cells (hepatocytes, intestinal, and skin cells). Organ injury was diminished in asmase−/− hosts, and morbidity and mortality improved at 90 days after transplantation. Resistance to cytolytic T lymphocyte–induced apoptosis was found at the target cell membrane if hepatocytes lack ASMase, as hepatocyte apoptosis required target cell ceramide generation for formation of ceramide-rich macrodomains, sites concentrating proapoptotic Fas. These studies indicate a requirement for target cell ASMase in evolution of GVHD in liver, small intestines, and skin and provide potential new targets for disease management.
Introduction
Graft-versus-host disease (GVHD) is a major complication of allogeneic hematopoietic stem cell transplantation (HSCT) and is defined as a progressive systemic disease, which specifically affects the intestines, liver, and skin.1 The complex pathophysiology of GVHD involves initial host tissue damage from the conditioning regimen (chemotherapy and/or radiation) resulting in stress (or “danger”) signals (including inflammatory cytokines, chemokines, and ligands that trigger the innate immune system), which fuel the activation of alloreactive T cells by antigen-presenting cells (APCs). The activation and proliferation of large numbers of donor-derived CD4 and/or CD8 alloreactive T cells are indispensable for GVHD.
Murine and human datasets delineate the importance of T cell–cytotoxic pathways, including Fas ligand (FasL), perforin/granzymes, tumor necrosis factor (TNF), TNF-related apoptosis-inducing ligand, and TNF-like weak inducer of apoptosis in systemic and target organ GVHD.2 In murine GVHD models, inhibition of Fas or FasL resulted in most cases (7 of 8 studies) in decreased mortality,3-9 uniformly associated with less hepatic GVHD,3,6,10 although some studies reported less intestinal and cutaneous GVHD as well.3,6 The one study that differed from the others used lpr recipient mice that manifest chronic Fas inactivation and display markedly increased T-cell proliferation, attributed to increased antigen presentation by an up-regulated APC population normally deleted in a Fas-dependent manner.10 Studies examining the role of the perforin/granzyme pathway in GVHD resulted in conflicting results, with some studies reporting decreased or delayed GVHD mortality3-5,11-13 and others reporting no effect.7,8,14,15 Only one study examined the impact of perforin inhibition on target organ GVHD and found no differences. Finally, studies with TNF-deficient donors or TNF receptor–deficient recipients demonstrated the relevance of TNF for systemic and intestinal GVHD.16,17
Recent studies have indicated that the sphingomyelin pathway and its second messenger ceramide regulate TNF superfamily receptor–induced apoptosis in some systems,18,19 as well as apoptosis in select liver and gastrointestinal (GI) stress responses in vivo. Ceramide generation occurs rapidly in hepatic ischemia-reperfusion injury,20 TNF-induced hepatitis/cirrhosis,21 and radiation-induced GI toxicity.22 Genetic or pharmacologic inhibition of acid sphingomyelinase (ASMase)–mediated ceramide generation markedly attenuates pathogenesis of these syndromes. Mechanistic studies indicate that signaling through ceramide is mediated by its unique biophysical capacity to self-associate via hydrogen bonding and van der Waal forces, thereby forming large (1-5 μm), segregated membrane domains termed platforms.23 Whereas sphingomyelin is preferentially concentrated in the exoplasmic leaflet of the plasma membrane of all mammalian cells,24 stress-induced rapid translocation of ASMase onto the outer plasma membrane coincident with enzyme activation generates ceramide from sphingomyelin therein. Generated ceramide rapidly coalesces into ceramide-rich platforms,23,25 sites for protein oligomerization, including in some systems Fas and other members of the TNF superfamily,26,27 leading to transmembrane signaling. Consistent with this latter observation, disruption of platform generation abrogates signal transduction in multiple systems in vitro.25,28,29
To test the hypothesis that host ASMase might be directly involved in the pathogenesis of acute GVHD, we used a clinically relevant genetic model of GVHD using asmase+/+ and asmase−/− recipients. The data specify involvement of recipient ASMase in the acute inflammatory stage of GVHD, pathogenesis of target organ injury, and GVHD mortality. In vitro studies revealed that alloreactive cytolytic T lymphocyte (CTL)–induced apoptosis of hepatocytes requires target cell ASMase-mediated ceramide generation and formation of large ceramide-rich plasma membrane signaling platforms. The present studies define ASMase activation in GVH target organs as essential for pathology of murine acute GVHD and provide potential new targets for pharmacologic intervention in this disease.
Methods
Cell culture
Cell culture medium for lymphocyte and bone marrow (BM) harvesting consisted of RPMI 1640 supplemented with 10% heat-inactivated fetal calf serum, 100 U/mL penicillin, 100 μg/mL streptomycin, 2 mM l-glutamine, and 50 μM 2-mercaptoethanol. Anti–murine CD16/CD32 Fc block (2.4G2), fluorochrome-labeled CD3 (145-2C11), CD4 (RM4-5), CD8 (53-6.7), CD62L (MEL-14), B220 (RA3-6B2), CD11c (HL3), Gr-1(RB6-8C5), CD11b(M1/70), and Ly-9.1 (30C7) antibodies were obtained from BD Biosciences PharMingen. Ammonium chloride red blood cell lysis buffer, concanavalin A (conA), and concanamycin A were obtained from Sigma-Aldrich.
Mice and BMT
Female LP/J (“LP,” H-2b), B10.BR (“B10,” H-2k), and B6.MRL.lpr mice were obtained from The Jackson Laboratory. Pure C57BL/6 asmase+/+ and asmase−/− mice were propagated using heterozygous breeding pairs and genotyped as described.30 SCID-asmase+/+ and SCID-asmase−/− mice were propagated similarly. Male and female hosts were used in bone marrow transplantation (BMT) experiments at 8 to 12 weeks of age. BMT protocols were approved by the Memorial Sloan-Kettering Cancer Center (MSKCC) Institutional Animal Care and Use Committee. BM cells were removed aseptically and T cell–depleted using anti–Thy-1.2 antibody and low-TOX-M rabbit complement (Cedarlane Laboratories). Splenic T cells were obtained by purification over a nylon wool column. T-cell purity, routinely more than 90% of the nylon wool column-passaged population, was assessed by flow cytometry to precisely calculate donor T-cell infusion. Cells were resuspended in Dulbecco modified essential medium and transplanted by tail-vein infusion into lethally irradiated recipients that had received 1100 cGy (350 cGy for SCID experiments) total body irradiation (137Cs source) as a split dose with 3 hours between doses on day 0. Mice were housed in a pathogen-free facility at MSKCC in sterilized micro-isolator cages and received normal chow and autoclaved hyperchlorinated drinking water (pH 3.0).
Assessment of GVHD
Survival was monitored daily, and ear-tagged animals in coded cages were individually scored weekly for 5 clinical parameters (weight loss, hunched posture, decreased activity, fur ruffling, and skin lesions) on a scale from 0 to 2. A clinical GVHD score was generated by summation of the 5 criteria scores (0-10) as described.31 GVHD target organ pathology for small intestine (proximal jejunum), liver, and skin (tongue and ear) was assessed in a blinded fashion on hematoxylin and eosin–stained 5-μm histopathology sections. Briefly, intestine and liver were scored for 19 to 22 different parameters associated with GVHD as described,32 and skin was evaluated for the number of dyskeratotic and apoptotic cells, as published.33 Villus and crypt cell apoptosis was scored by quantification of TdT-mediated dUTP nick-end labeling (TUNEL)–positive nuclei.22 Because of a genetic shift in the B10.BR donor strain used in these studies, as reported by the vendor (The Jackson Laboratory) for these mice, transplantation of full major histocompatibility complex (MHC)–mismatched B10.BR BM into C57BL/6 recipients resulted in fatal bone marrow aplasia (beginning 21 days after transplantation), rendering survival experiments impossible. Assessment of brain, spinal cord, and lung specimen for evidence of Niemann-Pick disease (NPD) was performed by the Laboratory of Comparative Pathology at MSKCC.
Radiation, tissue preparation, and crypt microcolony survival assay
Whole-body radiation was delivered with a Shepherd Mark-I unit (Model 68, SN643) operating 137Cs sources at a dose rate of 2.02 Gy/min. Actuarial survival was monitored daily. The microcolony survival assay was performed as described previously.34,35 Briefly, 3.5 days after irradiation, mice were killed by hypercapnia asphyxiation, and samples of the small intestine were harvested and prepared for histologic staining. Surviving crypts were defined as containing 10 or more adjacent chromophilic non-Paneth cells, at least 1 Paneth cell, and a lumen. The number of surviving crypts was counted per circumference of a transverse cross section of the intestine. Ten to 20 circumferences were scored per mouse, and 2 to 4 mice were used to generate each data point.
Flow cytometric analysis and in vivo CFSE staining
Splenocytes were incubated with CD16/CD32 FcR block on ice for 15 minutes, subsequently incubated with primary antibodies for 45 minutes, washed, resuspended in fluorescence-activated cell sorter (FACS) buffer (phosphate-buffered saline + 2% bovine serum albumin + 0.1% NaN3), and analyzed on a FACScan flow cytometer (BD Biosciences) with CellQuest software. For carboxyfluorescein diacetate succinimidyl ester (CFSE) staining, red blood cell–lysed LP/J or B10.BR splenocytes were positively selected as per the manufacturer's instructions with anti-CD3 microbeads (Miltenyi Biotec), stained in 2.5 μM CFSE, and 15 to 20 × 106 stained cells were transplanted into C57BL/6 asmase+/+ or asmase−/− hosts. Splenocytes from these animals were harvested 72 hours (B10.BR) or 7 days (LP/J) thereafter, stained with fluorochrome-conjugated antibodies for surface antigens, and FACS analysis was carried out as detailed earlier in this section.
Enzyme-linked immunosorbent assay
Enzyme-linked immunosorbent assays for serum IL-1β, IL-2, interferon-γ (IFN-γ), and TNF-α levels were performed according to the manufacturer's instructions (R&D Systems).
Hepatocyte isolation
Hepatocytes were isolated by cannulation of the portal vein and retrograde in situ collagenase perfusion.36,37 Briefly, livers were perfused with 20 mL buffer 1 (Krebs Ringer with glucose + 0.1 mM ethyleneglycoltetraacetic acid) followed by 25 mL buffer 2 (Krebs Ringer with glucose containing 0.2 mM CaCl2 with 5000 units collagenase type I; Sigma-Aldrich) at 7 mL/min by peristaltic pump (Rainin Instrument LLC). Perfused livers were excised, minced in buffer 2, filtered through a 100-μm cell strainer, and resuspended in RPMI 1640 complete medium containing 10% fetal bovine serum (FBS). In some experiments, hepatocytes were further purified over a 60% Percoll gradient at 250g for 2 minutes. Viability was routinely more than 90%.
Hepatocyte apoptosis and platform detection assays
A total of 0.5 × 106 hepatocytes, rested for 30 minutes in complete medium, were stimulated for 16 hours at 37°C in 5% CO2 with 1 μg/mL anti-Fas Jo2 antibody (BD Biosciences PharMingen) or 0 to 2 × 106 splenic T cells isolated from asmase+/+ or asmase−/− C57BL/6 mice actively undergoing acute GVHD (10-21 days after transplantation of LP/J donor BM and T cells). In some studies, hepatocytes were pretreated for 30 minutes with nystatin (50 μg/mL) or dimethyl sulfoxide control (0.1% of total volume), and resuspended in RPMI supplemented with 1% lipid-free FBS before stimulation. For platform detection, stimulated hepatocytes were fixed with 4% formalin-buffered phosphate and blocked in phosphate-buffered saline containing 1% FBS, and surface ceramide was identified using a mouse monoclonal anti-ceramide antibody MID 15B4 IgM (1:50 dilution; Alexis Biochemicals) and Cy3- or fluorescein isothiocyanate (FITC)–conjugated anti–mouse IgM (1:500 or 1:100 dilution; Roche Diagnostics) as described.28 Fas was identified using recombinant mouse FasL fused to a 6× histidine tag (0.5 μg/mL, Sigma-Aldrich), rabbit anti-His6 antibody, and Cy3-conjugated antirabbit secondary antibody (1:100 dilution each; Roche Diagnostics). Fluorescence was detected with conventional fluorescence microscopy, using an Axiovert S-100 Zeiss fluorescence microscope, or with upright confocal microscopy using a Leica TCS SPZ. The percentage of cells containing platforms, that is, those in which the fluorescence condenses onto less than 15% of the cell surface, was determined by counting 150 to 250 cells per point. Apoptosis was quantified after staining with 100 μL of 24 μg/mL bis-benzimide trihydrochloride solution by nuclear morphology as described.28 Alternately, apoptosis was quantified by TUNEL staining according to the manufacturer's instructions (Roche Diagnostics). A minimum of 200 cells were examined per point.
Mixed lymphoctye reaction
Balb/c effector splenocytes were in vitro activated by incubation with 5 × 106 irradiated (20 Gy) C57BL/6 splenocytes in RPMI 1640 + 10% FBS for 5 days. At 2 days before the mixed lymphocyte reaction (MLR), asmase+/+ or asmase−/− target splenocytes were activated with 10 μg/mL conA (Sigma-Aldrich). Activated target splenocytes were labeled on the day of experiment with 200 nM Mitotracker Red CMXRos (Invitrogen) for 30 minutes for the purpose of detection or with 1 μCi/mL Na251CrO4 for 45 minutes at 37°C in 5% CO2, washed in RPMI 1640 + 10% FBS, and coincubated with activated Balb/c splenocytes in complete medium at 37°C. Platforms were detected after staining with anti-ceramide monoclonal antibody (mAb) and FITC-conjugated anti–mouse IgM, as described in “Hepatocyte apoptosis and platform detection assays.” Lysis of Na251CrO4-labeled target cells was quantified by 51Cr release into the supernatant by gamma counter (Cobra) using the formula: corrected % lysis = 100 × (sample 51Cr release − control 51Cr release)/(maximum 51Cr release − control 51Cr release), as described.8 In some studies, 500 nM C16-ceramide or C16-dihydroceramide (5 μM stock solution in EtOH:dodecane 98:2 at a final concentration of 0.1%) was provided to the target splenocytes before coincubation with effector cells. Alternatively, CFSE-labeled LP/J splenocytes were coincubated with irradiated (20 Gy) C57BL/6 dendritic cells (asmase+/+ or asmase−/−) in RPMI 1640 + 10% FBS for 5 days, and CFSE dilution of the CD4+ and CD8+ populations was determined by flow cytometry as described in “Flow cytometric analysis and in vivo CFSE staining.”
AICD assay
Activation-induced cell death (AICD) was induced on T cells as previously reported.38 Briefly, T cells were primed with 10 μg/mL conA (Sigma-Aldrich) for 48 hours, rested in medium containing 20 U/mL IL-2 (R&D Systems) for 24 hours, and resuspended in medium containing 20 U/mL IL-2 and anti-CD3 mAb. Platforms were detected 4 hours after anti-CD3 mAb incubation (10 μg/mL). In some experiments, cells were additionally stained with FITC-conjugated cholera toxin β-subunit (2 μg/mL; Sigma-Aldrich). Apoptosis was quantified 24 hours after incubation with anti-CD3 mAb (0-10 μg/mL).
Statistics
Statistical analysis of GVHD scores, splenocyte number, and proliferation assays was performed using the nonparametric unpaired Mann-Whitney U test. Mantel-Cox log-rank test was used for survival data. The 2-sided Student t test with 95% confidence estimations was used for all other analyses.
Results
Engagement of ASMase in minor and major HA-disparate models of GVHD
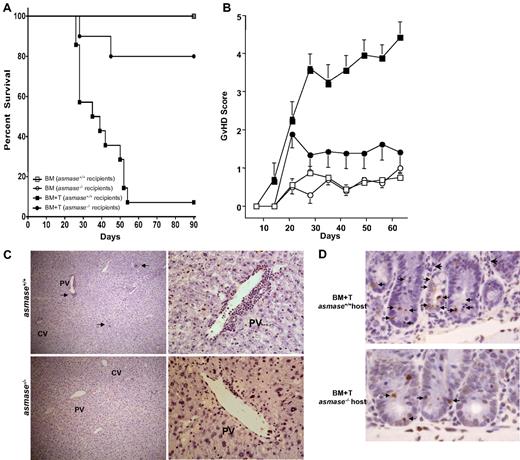
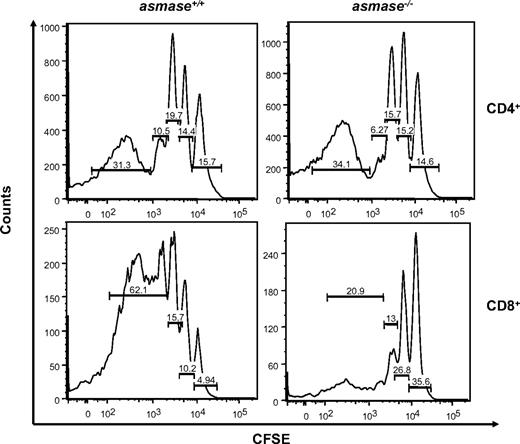
To evaluate involvement of host ASMase in CTL-mediated tissue injury during acute GVHD, we used the mHA-disparate LP/J (H-2b) → C57BL/6 (H-2b) allogeneic HSCT model. Lethally irradiated wild-type (asmase+/+) C57BL/6 or asmase−/− littermates received 5 × 106 T cell–depleted (TCD) LP/J BM cells and 3 × 106 LP/J donor splenic T cells. GVHD was observed in all recipients, albeit significantly reduced in asmase−/− recipients, as assessed by Kaplan-Meier survival curves (82.6% ± 7.9% survival in asmase+/+ recipients at day 90 compared with 17.6% ± 6.5% survival in asmase+/+ recipients; Figure 1A,P < .005), clinical GVHD scores (Figure 1B), and weight loss (not shown).
Host ASMase regulates graft-versus-host–associated morbidity, mortality, and target organ injury. Lethally irradiated (1100 cGy) C57BL/6asmase+/+ or C57BL/6asmase−/− mice received intravenous injection of LP TCD-BM cells (5 × 106) with or without splenic T cells (3 × 106). (A) Kaplan-Meier survival and (B) clinical GVHD score derived from weekly assessment of 5 clinical parameters (weight loss, hunched posture, decreased activity, fur ruffling, and skin lesions) are shown representing 6 to 8 BM control and 13 or 14 BM + T-cell recipients per group compiled from 2 experiments. Statistical analysis is as follows: (A) BM (asmase+/+ hosts) versus BM + T (asmase+/+ hosts), P < .001; BM + T (asmase+/+ hosts) versus BM + T (asmase−/− hosts), P < .001. (B) BM (asmase+/+ hosts) versus BM + T (asmase+/+ hosts)j P < .005; BM + T (asmase+/+ hosts) versus BM + T (asmase−/− hosts)j P < .005. (C) C57BL/6asmase+/+ or C57BL/6asmase−/− mice received transplants as described in Figure 1 and were killed 21 days thereafter for histopathologic analysis. Representative 5-μm hematoxylin and eosin–stained liver sections reveal increased lymphocyte infiltration (arrows) around the central and portal veins and destruction of hepatic architecture in asmase+/+ hosts receiving allogeneic T cells compared with asmase−/− littermates (left panels). Images were acquired using Zeiss Plan-NEOFLUAR 5×/0.3 numeric aperture (NA) dry lens (Carl Zeiss Inc) and QImaging camera model Retiga EX, and were processed with Improvision Volocity software (PerkinElmer) and Adobe Photoshop Version 7.0 software (Adobe Systems). Right panels reveal higher magnification images of typical endotheliitis observed around a portal vein in asmase+/+ (top panels) but not asmase−/− (bottom panels) hosts. Images were acquired as in left panels, using a Zeiss Plan-NEOFLUAR 40×/1.3 NA oil DIC lens. (D) Representative 5-μm TUNEL-stained sections of proximal jejunum crypts displaying epithelial apoptosis. Images were acquired as in panel C, using a Zeiss Plan-NEOFLUAR 40×/1.3 NA oil DIC lens. Small arrows indicate cells containing condensed or fragmented brown nuclei contrasting with the blue stain of nonapoptotic nuclei, quantified in panel E. Large arrows indicate areas of inflammatory cell infiltration. Crypt apoptosis (E) was scored in 200 crypts per point. Data (mean ± SEM) are collated from 2 experiments. Frequency histograms of apoptotic cells in the villus lamina propria (F) represent data from 150 villae per point, collated from 2 experiments. (G) C57BL/6 recipient hosts received marrow transplants as detailed earlier in the Figure 1 legend, and skin (tongue and ear) was harvested 21 days thereafter. Alternatively, skin was harvested 14 days after transplantation of 10 × 106 TCD-BM cells with or without 0.5 × 106 T cells from B10.BR (H2k) donors. Skin GVHD score was determined by the number of dyskeratotic apoptotic keratinocytes per millimeter of epidermis (mean ± SEM) as assessed in blinded fashion on hematoxylin and eosin–stained sections. Data represent 4 to 14 mice per group compiled from 3 independent experiments.
Host ASMase regulates graft-versus-host–associated morbidity, mortality, and target organ injury. Lethally irradiated (1100 cGy) C57BL/6asmase+/+ or C57BL/6asmase−/− mice received intravenous injection of LP TCD-BM cells (5 × 106) with or without splenic T cells (3 × 106). (A) Kaplan-Meier survival and (B) clinical GVHD score derived from weekly assessment of 5 clinical parameters (weight loss, hunched posture, decreased activity, fur ruffling, and skin lesions) are shown representing 6 to 8 BM control and 13 or 14 BM + T-cell recipients per group compiled from 2 experiments. Statistical analysis is as follows: (A) BM (asmase+/+ hosts) versus BM + T (asmase+/+ hosts), P < .001; BM + T (asmase+/+ hosts) versus BM + T (asmase−/− hosts), P < .001. (B) BM (asmase+/+ hosts) versus BM + T (asmase+/+ hosts)j P < .005; BM + T (asmase+/+ hosts) versus BM + T (asmase−/− hosts)j P < .005. (C) C57BL/6asmase+/+ or C57BL/6asmase−/− mice received transplants as described in Figure 1 and were killed 21 days thereafter for histopathologic analysis. Representative 5-μm hematoxylin and eosin–stained liver sections reveal increased lymphocyte infiltration (arrows) around the central and portal veins and destruction of hepatic architecture in asmase+/+ hosts receiving allogeneic T cells compared with asmase−/− littermates (left panels). Images were acquired using Zeiss Plan-NEOFLUAR 5×/0.3 numeric aperture (NA) dry lens (Carl Zeiss Inc) and QImaging camera model Retiga EX, and were processed with Improvision Volocity software (PerkinElmer) and Adobe Photoshop Version 7.0 software (Adobe Systems). Right panels reveal higher magnification images of typical endotheliitis observed around a portal vein in asmase+/+ (top panels) but not asmase−/− (bottom panels) hosts. Images were acquired as in left panels, using a Zeiss Plan-NEOFLUAR 40×/1.3 NA oil DIC lens. (D) Representative 5-μm TUNEL-stained sections of proximal jejunum crypts displaying epithelial apoptosis. Images were acquired as in panel C, using a Zeiss Plan-NEOFLUAR 40×/1.3 NA oil DIC lens. Small arrows indicate cells containing condensed or fragmented brown nuclei contrasting with the blue stain of nonapoptotic nuclei, quantified in panel E. Large arrows indicate areas of inflammatory cell infiltration. Crypt apoptosis (E) was scored in 200 crypts per point. Data (mean ± SEM) are collated from 2 experiments. Frequency histograms of apoptotic cells in the villus lamina propria (F) represent data from 150 villae per point, collated from 2 experiments. (G) C57BL/6 recipient hosts received marrow transplants as detailed earlier in the Figure 1 legend, and skin (tongue and ear) was harvested 21 days thereafter. Alternatively, skin was harvested 14 days after transplantation of 10 × 106 TCD-BM cells with or without 0.5 × 106 T cells from B10.BR (H2k) donors. Skin GVHD score was determined by the number of dyskeratotic apoptotic keratinocytes per millimeter of epidermis (mean ± SEM) as assessed in blinded fashion on hematoxylin and eosin–stained sections. Data represent 4 to 14 mice per group compiled from 3 independent experiments.
Consistent with survival data, host target organ pathology at 21 days after allotransplantation was ameliorated in asmase−/− recipients. Semiquantitative histopathologic analyses based on 19 standardized criteria for liver GVHD39 revealed significantly higher liver GVHD scores in asmase+/+ recipients than in asmase−/− littermates (Table 1). Morphologic manifestations of hepatic damage, characterized by lymphocyte infiltration (Figure 1C left panel arrows), portal tract inflammation, endotheliitis (Figure 1C right panels), and loss of hepatic architecture were less prominent in asmase−/− recipients. Similarly, histopathologic analyses based on 22 criteria of intestinal GVHD, including villus blunting and mucosal atrophy, generalized inflammation, and apoptosis,39 were attenuated in asmase−/− recipients (Table 1). Apoptotic damage to epithelium within the stem cell/clonogen compartment of the crypts of Lieberkühn decreased from 3.8 (± 0.4) apoptotic cells/crypt in asmase+/+ mucosa to 0.95 (± 0.2) apoptotic cells/crypt in asmase−/− recipients (Figure 1D: large arrows identify inflammation, and small arrows represent apoptotic epithelial cells within the crypt; quantified in Figure 1E, P < .05). TUNEL staining of jejunal specimens from asmase+/+ recipients revealed significant endothelial apoptosis (> 3 apoptotic endothelial cells per villus) in 88.4% of villi lamina propria, with many showing extensive apoptosis (≥ 10 apoptotic cells/villus), decreased to 25.4% in asmase−/− recipients (Figure 1F, P < .05). ASMase deficiency also protected hosts from cutaneous keratinocyte apoptosis, decreased from 8.2 (± 1.2) apoptotic cells/mm2 of asmase+/+ epidermis to 5.1 (± 0.9) apoptotic cells/mm2 in asmase−/− epidermis (Figure 1G, P < .05).
Similar clinical-pathologic abnormalities were observed in an MHC-disparate allogeneic BMT model of B10.BR (H-2k) into C57BL/6 recipients (H-2b). ASMase deficiency attenuated hepatic and intestinal pathology scores (Table 1), hepatic lymphocyte infiltration, endotheliitis, and global destruction of the hepatic architecture (not shown), crypt epithelium apoptosis (59.3% ± 3.8% of crypts containing apoptotic cells in asmase+/+ vs 15.8% ± 3.7% in asmase−/− hosts, P < .05), and keratinocyte apoptosis (apoptotic index of 11.2 ± 1.2 apoptotic cells/mm2 epidermis in wild-type mice vs 3.2 ± 1.7 in asmase−/− littermates; Figure 1G; P < .01).
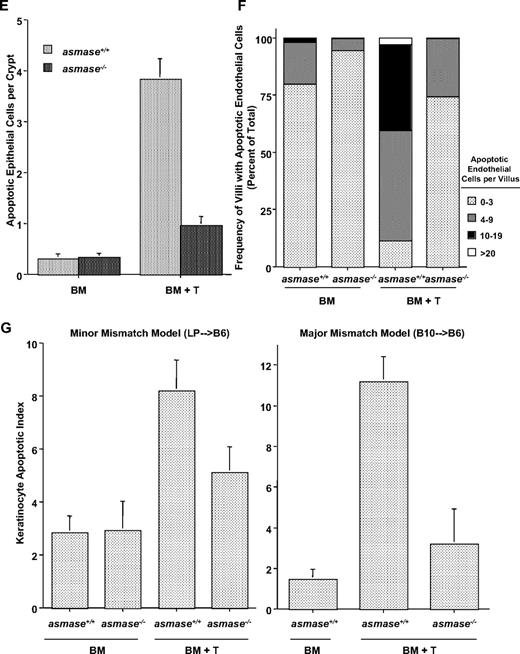
ASMase deficiency does not impact preconditioning injury or engraftment
Because severity of GVHD may depend on intensity of pretransplantation conditioning of the GI tract40,41 and because ASMase-dependent endothelial cell apoptosis within the GI tract contributes to radiation damage at doses more than 10 Gy,22 we examined whether host ASMase deficiency might impact GVHD outcome by affecting conditioning. Using the crypt microcolony assay, a measure of crypt stem cell survival,35,42 we compared the extent of GI damage after 11-Gy split-dose radiation (2 × 5.5 Gy) used in our conditioning regimen, to 11-Gy single dose. Although asmase−/− mice are less sensitive to crypt lethality after 11-Gy single-dose (P < .01; Figure 2A), recapitulating published data,30 there was no significant difference in crypt survival after 11-Gy split-dose (P > .05, Figure 2A). These data, consistent with findings that 5.5 Gy is below the threshold for radiation-induced endothelial cell apoptosis,22 suggest that enhanced survival in asmase−/− recipients is not attributable to attenuated conditioning injury. Reduced sensitivity to GVHD in asmase−/− recipients was similarly not attributable to enhanced survival of host immune elements after preconditioning, as no differences were observed in the number of host-derived CD4+ or CD8+ lymphocytes 14 days after transplantation (Table 2). Indeed, elimination of mature host B and T lymphocytes by crossing asmase+/+ and asmase−/− animals with animals harboring the SCID mutation did not restore asmase−/− recipient sensitivity to GVHD morbidity and mortality in an mHA-disparate LP/J (H-2b) → C57BL/6 (H-2b) allogeneic HSCT model (Figure 2B, P < .05). Although every SCID-asmase+/+ animal died with extensive evidence of clinical GVHD scoring (not shown) and necropsy evidence of liver and GI damage characteristic of GVHD-associated mortality (90% mortality within 32 days; supplemental Table 1 [available on the Blood website; see the Supplemental Materials link at the top of the online article]), all SCID-asmase−/− animals survived the first 32 days after BMT. Thereafter, after a period of a few weeks, 66.7% of SCID-asmase−/− animals died of an accelerated form of NPD, as autopsy revealed neuronal vacuolation and Purkinje cell dropout, lung infiltration with vacuolated macrophages, and evidence of eosinophilic crystalline pneumonia in these animals, with only mild to moderate lymphocyte infiltration, apoptosis, or other GVH-associated damage to small intestines and liver (supplemental Table 1). It should be noted that clinical and pathologic NPD did not impact our earlier studies, as it occurs only after 6 to 9 months in our C57BL/6asmase−/− colony. Finally, no differences were observed in immune ablation or graft take. asmase−/− mice displayed equal sensitivity to bone marrow aplasia after 10- to 12-Gy radiation compared with asmase+/+ littermates (Figure 2C; and data not shown), an equal or greater proportion of donor-derived lymphoid cells at 14 days after infusion of TCD-BM (Table 3), and no statistically significant differences in hematopoietic reconstitution 21 days after BMT (supplemental Table 2). Taken together, these data identify host sensitivity to target cell apoptosis, and not differences in preconditioning, host immune function, or engraftment, as the major determinant of reduced sensitivity to acute GVHD-associated organ damage in asmase−/− hosts.
Preconditioning injury or host immune function does not contribute to impaired GVHD sensitivity in asmase−/− recipients. (A) Wild-type and asmase−/− C57BL/6 mice were exposed to 11-Gy split-dose radiation (5.5 Gy × 2 separated by 3 hours) or 11-Gy single dose. Proximal jejunum was harvested 3.5 days thereafter, and the microcolony assay performed according to the method of Withers and Elkind.35 Data (mean ± SEM) were compiled from 2 to 4 animals irradiated concomitantly, with 10 to 20 circumferences scored per mouse. (B) Irradiated (350 cGy split-dose) SCID-C57BL/6asmase+/+ or SCID-C57BL/6asmase−/− mice received BM and T cells as in Figure 1A, and were monitored for survival. Note that SCID-C57BL/6asmase−/− mice died with significant lung and central nervous system damage consistent with development of accelerated NPD while displaying only minimal to moderate evidence of GVHD (supplemental Table 2). (C) Actuarial survival of 8- to 12-week-old male wild-type and asmase−/− C57BL/6 mice exposed to 10 or 12 Gy whole-body radiation. Actuarial survival was calculated by the product-limit Kaplan-Meier method. Nine to 12 animals were irradiated per group.
Preconditioning injury or host immune function does not contribute to impaired GVHD sensitivity in asmase−/− recipients. (A) Wild-type and asmase−/− C57BL/6 mice were exposed to 11-Gy split-dose radiation (5.5 Gy × 2 separated by 3 hours) or 11-Gy single dose. Proximal jejunum was harvested 3.5 days thereafter, and the microcolony assay performed according to the method of Withers and Elkind.35 Data (mean ± SEM) were compiled from 2 to 4 animals irradiated concomitantly, with 10 to 20 circumferences scored per mouse. (B) Irradiated (350 cGy split-dose) SCID-C57BL/6asmase+/+ or SCID-C57BL/6asmase−/− mice received BM and T cells as in Figure 1A, and were monitored for survival. Note that SCID-C57BL/6asmase−/− mice died with significant lung and central nervous system damage consistent with development of accelerated NPD while displaying only minimal to moderate evidence of GVHD (supplemental Table 2). (C) Actuarial survival of 8- to 12-week-old male wild-type and asmase−/− C57BL/6 mice exposed to 10 or 12 Gy whole-body radiation. Actuarial survival was calculated by the product-limit Kaplan-Meier method. Nine to 12 animals were irradiated per group.
Host ASMase deficiency attenuates serum proinflammatory cytokine elevation and CD8+ T-cell proliferation
Pathogenesis of acute GVHD involves an early inflammatory “cytokine storm” resulting from tissue damage from the conditioning regimen coupled to alloreactive T-cell activation, proliferation, and cytokine secretion. As expected, serum levels of IL-2 and IFN-γ, IL-1β, and TNF-α at day 7 after BMT were significantly increased in recipients of BM + T cells compared with recipients of BM cells only (P < .05, Table 4). Serum levels for IL-2, IFN-γ, IL-1β, and TNF-α, however, were significantly lower in asmase−/− versus asmase+/+ recipients of BM + T cells. We confirmed these findings in a second GVHD model (B10.BR→C56BL/6) and found lower serum levels of IFN-γ and TNF-α in asmase−/− versus asmase+/+ recipients of BM + T cells. These data indicate that asmase−/− recipients have significantly lower levels of proinflammatory cytokines during the early stage of GVHD development.
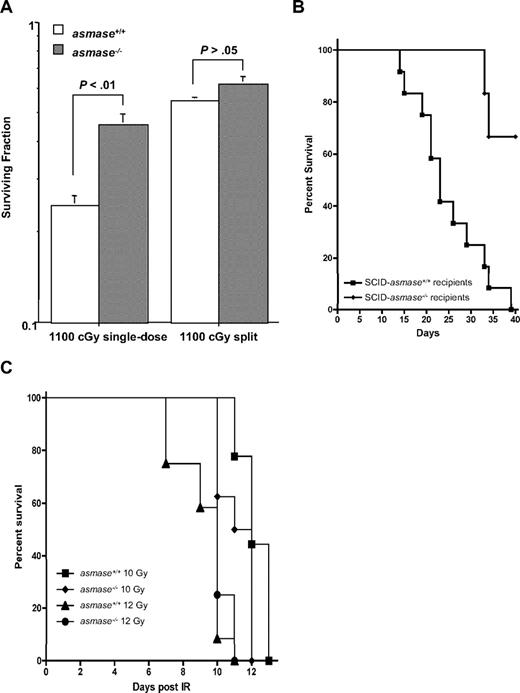
Whereas in vivo expansion of LP and B10.BR CD4+ T cells, determined by retention of the CFSE label, was not statistically different in asmase+/+ or asmase−/− littermates (Figure 3 top panels; and data not shown for B10.BR), rapid proliferation of alloreactive donor CD8+ T cells was significantly impaired in asmase−/− recipients of LP/J (Figure 3 bottom panels; from 62.1% in asmase+/+ to 20.9% in asmase−/− hosts; P < .005) and B10.BR splenocytes (from 50.9% ± 1.6% in asmase+/+ to 30.0% ± 3.5% in asmase−/− recipients, n = 3, P < .005, not shown). Attenuation of CD8+ T-cell proliferation in asmase−/− recipients resulted in significant reduction in splenic donor LP/J CD8+ T cells 14 days after BMT (Table 2, P < .001). This reduction in LP/J donor CD8+ cells did not result from inability of asmase−/− DCs to stimulate splenocyte proliferation, as equal CFSE dilution of LP/J CD4+ and CD8+ T cells was observed after stimulation with either asmase−/− or asmase+/+ DCs in vitro (not shown). Nor did it result from differences in the number of host DCs in asmase−/− compared with asmase+/+ hosts after preconditioning (not shown). Finally, the impairment in CD8+ T-cell proliferation was not a result of an inherent defective capacity to proliferate once exposed to an asmase−/− environment, as splenic T cells harvested from asmase−/− and asmase+/+ recipients displayed similar specific proliferative responses ex vivo when challenged with conA (supplemental Figure 1), and exhibited intact proliferation in response to irradiated third-party stimulation (BALB/c). We conclude that alloreactive proliferation of donor CD8+ T cells in asmase−/− recipients is significantly diminished, and we speculate that this reduction is a result of a direct or indirect effect of lower levels of proinflammatory cytokines (causing less activation of donor and host APCs).
Donor CD8+ T-cell expansion is impaired in asmase−/− hosts. C57BL/6asmase+/+ and C57BL/6asmase−/− recipients were infused with 15 to 206 CFSE-stained splenic CD3+ T cells from LP/J donors as described in “Flow cytometric analysis and in vivo CFSE staining.” Spleens were harvested 7 days thereafter and multicolor flow cytometry was performed. Percentage of CFSE “high” (cells with mean fluorescent values ≥ 104) and “low” (mean fluorescent values ≤ 103) CD4+ and CD8+ populations are shown from 1 representative of 2 independent experiments.
Donor CD8+ T-cell expansion is impaired in asmase−/− hosts. C57BL/6asmase+/+ and C57BL/6asmase−/− recipients were infused with 15 to 206 CFSE-stained splenic CD3+ T cells from LP/J donors as described in “Flow cytometric analysis and in vivo CFSE staining.” Spleens were harvested 7 days thereafter and multicolor flow cytometry was performed. Percentage of CFSE “high” (cells with mean fluorescent values ≥ 104) and “low” (mean fluorescent values ≤ 103) CD4+ and CD8+ populations are shown from 1 representative of 2 independent experiments.
CTL-induced hepatocyte apoptosis requires ceramide-rich platforms in an ex vivo model of GVHD
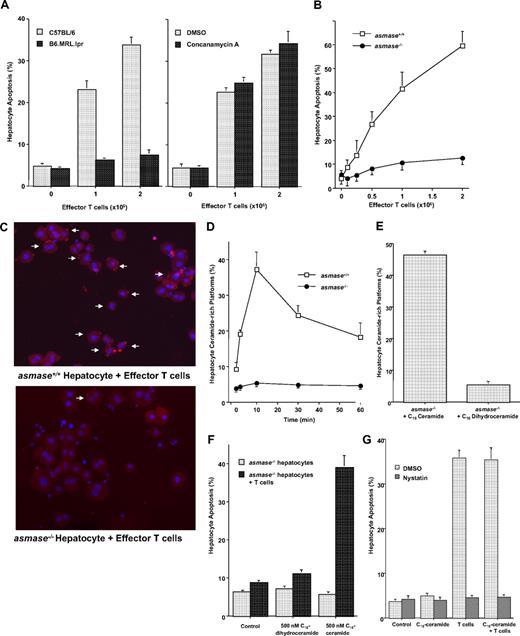
Because differences in tissue damage with the total body irradiation dosing schedule used as conditioning regimen were not found (Figure 2A,C), we investigated whether ASMase deficiency renders target cells directly resistant to CTL-induced apoptosis using a 2-cell ex vivo model of alloactivated splenic CTL effectors and untreated C57BL/6 hepatocytes. Hepatocytes were chosen as target cells in this assay because they are classic target cells for GVHD and use the sphingomyelin pathway for apoptosis.20,21,43 Coincubation with 0 to 2 × 106 alloactive splenic T cells increased hepatocyte apoptosis from 4.7% (± 0.7%) to 33.8% (± 1.9%) by 16 hours, detected by nuclear morphologic changes (Figure 4A). In contrast, syngeneic LP hepatocytes did not undergo significant apoptosis above baseline (not shown). Consistent with in vivo studies,6 B6.MRL.lpr hepatocytes lacking functional Fas receptors were resistant to CTL-induced apoptosis (Figure 4A left panel), whereas selective inhibition of the granule exocytosis-mediated cytolytic pathway by 2-hour incubation with 100 ng/mL concanamycin A (supplemental Figure 2) had no effect on hepatocyte apoptosis (Figure 4A right panel). These studies suggest that CTL-mediated hepatocyte apoptosis in this model requires Fas but not perforin/granzyme signaling. Although previous studies showed that Fas levels were unaltered in asmase−/− hepatocytes,43 asmase−/− hepatocytes were nonetheless resistant to apoptosis at all doses of allogeneic effector T cells from 0.1 to 2 × 106 (Figure 4B), and always from 4 to 48 hours (data not shown). Further, as C57BL/6 asmase−/− DCs equally stimulated proliferation and CFSE dilution of MHC-disparate LP splenocytes as asmase+/+ DCs (supplemental Figure 3A; and data not shown), and donor T cells isolated from asmase−/− hosts equally lysed hepatocytes as asmase+/+ CTLs ex vivo (supplemental Figure 3B), it appears that the murine asmase−/− milieu allows for the full repertoire of events required for antigen processing and presentation, antigen recognition by incipient CTLs, and their full activation. Collectively, the in vivo and ex vivo studies suggest that an intrinsic deficit in ceramide signaling plays an important role in attenuated liver GVHD in asmase−/− recipients.
In vivo activated allogeneic CTLs require target hepatocyte ASMase for efficient killing ex vivo. Hepatocytes, isolated as described in “Hepatocyte isolation,” were coincubated with splenic T cells harvested from lethally irradiated wild-type C57BL/6 recipients 10 to 14 days after transplantation of LP BM+ T cells. (A) A total of 2 × 106 GVH-activated splenic CTLs were coincubated with 0.5 × 106 wild-type C57BL/6 or B6.MRL.lpr (FasR−/−) hepatocytes (left panel) in complete medium for 16 hours. Alternatively, dimethyl sulfoxide– or concanamycin A–pretreated (100 ng/mL, 30 minutes) GVH-activated splenic CTLs were coincubated with 0.5 × 106 wild-type C57BL/6 hepatocytes for 16 hours (right panel). Apoptosis was quantified after fixation by nuclear bisbenzimide staining. (B) asmase−/− hepatocytes are resistant to apoptosis induced by GVH-activated splenic CTLs. CTL coincubation was performed as in panel A, and apoptosis was quantified 16 hours thereafter. (C) Representative images of asmase+/+ (top left panel) and asmase−/− (bottom left panel) C57BL/6 hepatocytes after 10 minutes of coincubation in suspension with 2 × 106 GVH-activated splenic T cells. Hepatocytes were fixed and stained with 4,6-diamidino-2-phenylindole (DAPI) and Cy-3-labeled anticeramide mAb as described in “Hepatocyte apoptosis and platform detection assays.” Arrows indicate ceramide-rich platform generation on the outer leaflet of the plasma membrane. Note that, after incubation, cells were centrifuged at 50g for 4 minutes at 4°C before staining and imaging. Hence, CTLs (small blue nuclei) distributed with hepatocytes (large blue nuclei) do not reflect biologic association. Images were acquired using Zeiss Plan-NEOFLUAR 40×/1.3 NA oil DIC lens and Zeiss AxioCam MRm camera, and were processed with Zeiss AxioVision software and Adobe Photoshop Version 7.0 software. (D) Quantification of ceramide-rich platforms in asmase+/+ and asmase−/− hepatocytes after incubation with 2 × 106 GVH-activated splenic CTLs. A total of 0.5 × 106 hepatocytes were coincubated for the indicated times, fixed, and stained as in panel C. Exogenous C16-ceramide bypasses the requirement for target cell ASMase, restoring platform generation (E) and conferring apoptosis (F) onto GVH-activated CTL-stimulated asmase−/− hepatocytes. Platform generation and apoptosis were quantified as in panels D and A, respectively. (G) Disruption of membrane GEMs with nystatin inhibits CTL-induced hepatocyte apoptosis. A total of 0.5 × 106 wild-type hepatocytes, preincubated with 50 μg/mL nystatin for 30 minutes and resuspended in RPMI containing 1% lipid-free FBS, were coincubated with 2 × 106 GVH-activated splenic T cells, and apoptosis was quantified as in panel A. Data (mean ± SEM) represent triplicate determinations from 3 independent experiments each for panels A, B, D, E, F, and G.
In vivo activated allogeneic CTLs require target hepatocyte ASMase for efficient killing ex vivo. Hepatocytes, isolated as described in “Hepatocyte isolation,” were coincubated with splenic T cells harvested from lethally irradiated wild-type C57BL/6 recipients 10 to 14 days after transplantation of LP BM+ T cells. (A) A total of 2 × 106 GVH-activated splenic CTLs were coincubated with 0.5 × 106 wild-type C57BL/6 or B6.MRL.lpr (FasR−/−) hepatocytes (left panel) in complete medium for 16 hours. Alternatively, dimethyl sulfoxide– or concanamycin A–pretreated (100 ng/mL, 30 minutes) GVH-activated splenic CTLs were coincubated with 0.5 × 106 wild-type C57BL/6 hepatocytes for 16 hours (right panel). Apoptosis was quantified after fixation by nuclear bisbenzimide staining. (B) asmase−/− hepatocytes are resistant to apoptosis induced by GVH-activated splenic CTLs. CTL coincubation was performed as in panel A, and apoptosis was quantified 16 hours thereafter. (C) Representative images of asmase+/+ (top left panel) and asmase−/− (bottom left panel) C57BL/6 hepatocytes after 10 minutes of coincubation in suspension with 2 × 106 GVH-activated splenic T cells. Hepatocytes were fixed and stained with 4,6-diamidino-2-phenylindole (DAPI) and Cy-3-labeled anticeramide mAb as described in “Hepatocyte apoptosis and platform detection assays.” Arrows indicate ceramide-rich platform generation on the outer leaflet of the plasma membrane. Note that, after incubation, cells were centrifuged at 50g for 4 minutes at 4°C before staining and imaging. Hence, CTLs (small blue nuclei) distributed with hepatocytes (large blue nuclei) do not reflect biologic association. Images were acquired using Zeiss Plan-NEOFLUAR 40×/1.3 NA oil DIC lens and Zeiss AxioCam MRm camera, and were processed with Zeiss AxioVision software and Adobe Photoshop Version 7.0 software. (D) Quantification of ceramide-rich platforms in asmase+/+ and asmase−/− hepatocytes after incubation with 2 × 106 GVH-activated splenic CTLs. A total of 0.5 × 106 hepatocytes were coincubated for the indicated times, fixed, and stained as in panel C. Exogenous C16-ceramide bypasses the requirement for target cell ASMase, restoring platform generation (E) and conferring apoptosis (F) onto GVH-activated CTL-stimulated asmase−/− hepatocytes. Platform generation and apoptosis were quantified as in panels D and A, respectively. (G) Disruption of membrane GEMs with nystatin inhibits CTL-induced hepatocyte apoptosis. A total of 0.5 × 106 wild-type hepatocytes, preincubated with 50 μg/mL nystatin for 30 minutes and resuspended in RPMI containing 1% lipid-free FBS, were coincubated with 2 × 106 GVH-activated splenic T cells, and apoptosis was quantified as in panel A. Data (mean ± SEM) represent triplicate determinations from 3 independent experiments each for panels A, B, D, E, F, and G.
Whereas death receptor activation requires ceramide-rich platform generation in some systems,25,28 we explored CTL-induced platform generation in untreated allogeneic hepatocytes ex vivo. Alloactivated T cells induced a 1.5 (± 0.1)–fold overall increase in ceramide signal as determined by mean fluorescence intensity per pixel in asmase+/+ hepatocytes (Figure 4C; P < .005 vs unstimulated controls), which did not occur in asmase−/− hepatocytes. Generated ceramide clustered into platforms on the surface of the target hepatocytes after coincubation (Figure 4C), evident within 1 minute, peaking at 10 minutes, and persisting for more than 60 minutes (Figure 4D). Fas, required for apoptosis in this system, concentrated within ceramide-rich platforms (supplemental Figure 4), determined by confocal microscopy. In contrast, asmase−/− hepatocytes were completely resistant to ceramide-rich platform formation (Figure 4C; quantified in Figure 4D) and Fas concentration therein (supplemental Figure 4), demonstrating that CTL-induced platform generation in hepatocytes was ASMase-dependent.
Subapoptotic concentrations of exogenous C16-ceramide (up to 500 nM) restored platform formation in CTL-treated asmase−/− hepatocytes to 46.3% (± 1.3%) of cells (Figure 4E), demonstrating that ASMase-mediated ceramide generation drives platform formation. Hepatocyte apoptosis was specifically ceramide-dependent, as C16-ceramide nearly completely restored CTL-induced apoptosis to asmase−/− hepatocytes (Figure 4F), bypassing the requirement for target cell ASMase. In contrast, C16-dihydroceramide, the biologically inactive analog of C16-ceramide, failed to restore CTL-induced platform generation (Figure 4E) or hepatocyte apoptosis (Figure 4F). It thus appears that CTL-induced hepatocyte apoptosis ex vivo requires target cell ceramide generation for efficient cell death induction, consistent with in vivo protection from acute liver GVHD observed in asmase−/− mice. Furthermore, pharmacologic disruption of cell-surface sphingolipid microdomains, sites of sphingomyelin concentration, with the cholesterol-chelating agent nystatin28 abrogated CTL-induced ceramide-rich platform generation (not shown) and completely inhibited 2 × 106 alloactivated CTL-induced hepatocyte apoptosis (Figure 4G). Exogenous C16-ceramide was unable to overcome cholesterol chelation (Figure 4G), suggesting that ceramide-rich platform formation requires functional sphingolipid microdomains for signaling, possibly serving as a site for preassembly of the apoptotic machinery.
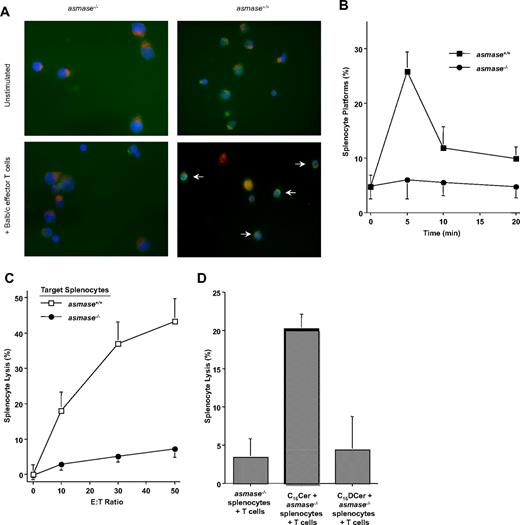
Multiple models of CTL-mediated apoptosis require target cell ASMase and ceramide-rich platforms
Resistance of asmase−/− target cells to CTL-induced lysis was similarly observed in 2 standardized assays for T cell–mediated cytolysis. Alloactivated BALB/c effector T cells, stimulated by culture for 5 days with 5 × 106 irradiated (2 Gy) C57BL/6 splenocytes, rapidly generated ceramide-rich platforms on Mitotracker Red–labeled target conA-activated splenocytes. Within 5 minutes of coincubation, the incidence of platforms on asmase+/+ splenocytes, identified as intense green staining condensed onto less than 15% of the cell surface, increased from 4.7% (± 2.1%) to 25.8% (± 6.6%; P < .01; Figure 5A; quantified in Figure 5B). Fas colocalized within these ceramide-rich platforms (not shown). In contrast, platform generation was absent in asmase−/− splenocytes. Furthermore, MLR-primed CTLs induced 43.2% (± 6.5%) asmase+/+ splenocyte lysis at an effector/target ratio of 50:1 (Figure 5C), attenuated to 7.3% (± 2.5%) in asmase−/− target cells, as quantified by 51Cr-release assay. Sublethal exogenous 500 nM C16-ceramide restored both platform generation and CTL-induced lysis of asmase−/− target splenocytes, whereas C16-dihydroceramide was ineffective in both events (Figure 5D; and data not shown).
In vitro–activated CTLs require target splenocyte ASMase for efficient killing. (A) Representative images and (B) quantification of ceramide-rich platforms (indicated by arrows in panel A) formed on the surface of Mitotracker Red–labeled, conA-activated (5 μg/mL for 24 hours) target C57BL/6asmase+/+ and C57BL/6asmase−/− splenocytes, on coincubation for 20 minutes with effector Balb/c splenic T cells that had been activated in vitro with 2 × 106 irradiated (20 Gy) C57BL/6 splenocytes/mL media for 5 days at a target/effector ratio of 2:1. Target splenocytes were fixed with 4% formalin-buffered phosphate, and stained with DAPI and FITC-labeled anticeramide mAb. Images were acquired as in Figure 4C. Platforms were identified as previously described.28 (C) Lysis of 51Cr-labeled target C57BL/6asmase+/+ and C57BL/6asmase−/− splenocytes after coincubation with effector Balb/c splenic T cells for 6 hours measured by the chromium-release assay. (D) Cytolytic response of 51Cr-labeled target C57BL/6asmase−/− splenocytes to activated effector Balb/c splenic T cells as in panel B, in the presence of 500 nM C16-ceramide or C16-dihydroceramide (DCer). Data (mean ± SEM) represent triplicate samples from 3 independent experiments for panels B through D.
In vitro–activated CTLs require target splenocyte ASMase for efficient killing. (A) Representative images and (B) quantification of ceramide-rich platforms (indicated by arrows in panel A) formed on the surface of Mitotracker Red–labeled, conA-activated (5 μg/mL for 24 hours) target C57BL/6asmase+/+ and C57BL/6asmase−/− splenocytes, on coincubation for 20 minutes with effector Balb/c splenic T cells that had been activated in vitro with 2 × 106 irradiated (20 Gy) C57BL/6 splenocytes/mL media for 5 days at a target/effector ratio of 2:1. Target splenocytes were fixed with 4% formalin-buffered phosphate, and stained with DAPI and FITC-labeled anticeramide mAb. Images were acquired as in Figure 4C. Platforms were identified as previously described.28 (C) Lysis of 51Cr-labeled target C57BL/6asmase+/+ and C57BL/6asmase−/− splenocytes after coincubation with effector Balb/c splenic T cells for 6 hours measured by the chromium-release assay. (D) Cytolytic response of 51Cr-labeled target C57BL/6asmase−/− splenocytes to activated effector Balb/c splenic T cells as in panel B, in the presence of 500 nM C16-ceramide or C16-dihydroceramide (DCer). Data (mean ± SEM) represent triplicate samples from 3 independent experiments for panels B through D.
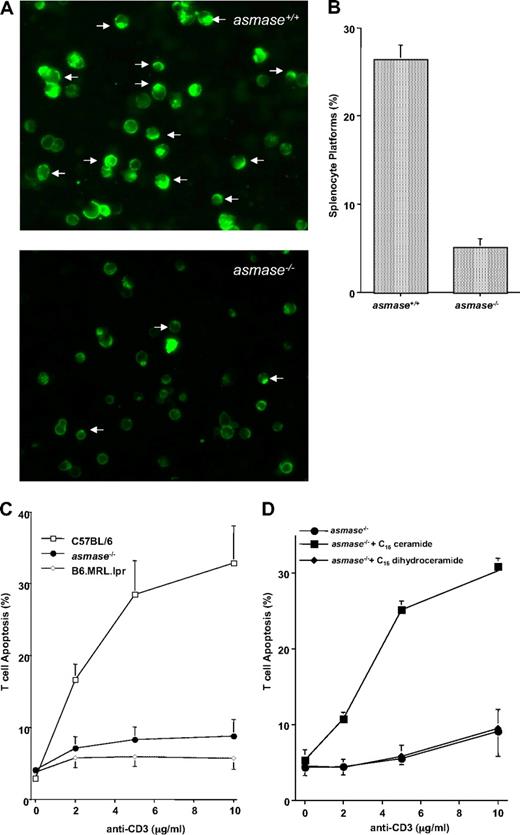
Similarly, asmase+/+, asmase−/−, or MRL.lpr (FasR−/−) T cells were stimulated for 24 hours with 10 μg/mL conA, washed, rested in medium containing 20 U/mL rIL-2 for 24 hours, and AICD initiated by restimulation in medium containing 20 U/mL rIL-2 and increasing concentrations of plate-bound anti-CD3 mAb for 24 hours.38 AICD induction by anti-CD3 mAb conferred ceramide-rich platform generation 4 hours after stimulation (Figure 6A), evident in 26.4% (± 1.6%) of asmase+/+ T cells compared with 5.1% (± 1.0%) of asmase−/− T cells (P < .005; Figure 6B). Confocal analysis identified colocalization of the sphingolipid GM1 (supplemental Figure 5) and Fas (supplemental Figure 6) within ceramide-rich platforms in asmase+/+ T cells.
Activation-induced cell death of splenocytes requires ASMase for efficient killing. (A) Representative images and (B) quantification of ceramide-rich platforms (arrows) formed on the surface of C57BL/6asmase+/+ and C57BL/6asmase−/− C57BL/6 splenic T cells 4 hours after induction of AICD with 10 ng/mL anti-CD3 as described in “Activation-induced cell death.” Cells were fixed with 4% formalin-buffered phosphate and stained with DAPI and FITC-labeled anticeramide mAb as in Figure 4C. Images were acquired as in Figure 4C. AICD induces a 2.0- ± 0.1-fold increase in the overall ceramide signal as determined by mean fluorescence intensity in asmase+/+ T cells (P < .005 compared with unstimulated controls), not evident in asmase−/− T cells, accounting for the difference in overall staining between panels. (C) Apoptotic response of C57BL/6asmase+/+ or C57BL/6asmase−/− splenic T cells after AICD apoptotic fratricide was induced as in panel A. Apoptosis was quantified 16 hours thereafter after nuclear bisbenzimide staining. (D) AICD was initiated in C57BL/6asmase−/− splenic T cells as in panel A, in the presence of 500 nM C16-ceramide or C16-dihydroceramide. Apoptosis was quantified 16 hours thereafter after nuclear bisbenzimide staining. Data (mean ± SEM) represent triplicate samples from 3 independent experiments for panels B through D.
Activation-induced cell death of splenocytes requires ASMase for efficient killing. (A) Representative images and (B) quantification of ceramide-rich platforms (arrows) formed on the surface of C57BL/6asmase+/+ and C57BL/6asmase−/− C57BL/6 splenic T cells 4 hours after induction of AICD with 10 ng/mL anti-CD3 as described in “Activation-induced cell death.” Cells were fixed with 4% formalin-buffered phosphate and stained with DAPI and FITC-labeled anticeramide mAb as in Figure 4C. Images were acquired as in Figure 4C. AICD induces a 2.0- ± 0.1-fold increase in the overall ceramide signal as determined by mean fluorescence intensity in asmase+/+ T cells (P < .005 compared with unstimulated controls), not evident in asmase−/− T cells, accounting for the difference in overall staining between panels. (C) Apoptotic response of C57BL/6asmase+/+ or C57BL/6asmase−/− splenic T cells after AICD apoptotic fratricide was induced as in panel A. Apoptosis was quantified 16 hours thereafter after nuclear bisbenzimide staining. (D) AICD was initiated in C57BL/6asmase−/− splenic T cells as in panel A, in the presence of 500 nM C16-ceramide or C16-dihydroceramide. Apoptosis was quantified 16 hours thereafter after nuclear bisbenzimide staining. Data (mean ± SEM) represent triplicate samples from 3 independent experiments for panels B through D.
AICD-associated apoptosis in asmase+/+ T cells was anti-CD3 mAb dose-dependent, reaching 32.9% (± 5.2%) apoptosis 16 hours after induction (Figure 6C). In contrast, apoptosis was abrogated in MRL.lpr (Fas-deficient) T cells (Figure 6C), confirming the requirement for Fas/FasL interaction in this system.44 Similarly, asmase−/− T cells manifested near-complete resistance to AICD-induced apoptosis in vitro. asmase−/− T cells failed to undergo detectable apoptosis above background (8.8%) in response to up to 10 ng/mL anti-CD3 (P < .05 vs asmase+/+ at 10 ng/mL anti-CD3; Figure 6C), despite normal up-regulation of Fas (supplemental Figure 7A) and FasL (supplemental Figure 7B). Natural long chain C16-ceramide, but not C16-dihydoceramide, restored platform generation in (not shown) and apoptosis of asmase−/− T cells stimulated to undergo AICD (Figure 6D). Thus, target cell ASMase-mediated ceramide-rich platform formation appears required for T cell–induced apoptosis in both antigen-disparate and fratricidic settings.
Discussion
The present studies define formation of ceramide-rich membrane platforms on the exoplasmic leaflet of the plasma membrane of target cells as critical for sensitivity to CTL-induced cell death. These structures, formed within seconds, are readily detected by confocal or conventional microscopy as they reach 1 to 5 μm in length. Although additional work will be required to fully identify substituents of these platforms, it is clear that in hepatocytes and conA blasts they concentrate ceramide, glycosphingolipids, such as GM1 (the target of cholera toxin), and activated cytokine receptors, such as Fas, consistent with previous findings.28 These structures probably serve as sites for the selective protein concentration and oligomerization necessary for transmission of death signals across the plasma membrane.25 Consistent with this notion, genetic or pharmacologic disruption of platforms prevents CTL-mediated death in in vivo–activated CTL, in vitro MLR, and in vitro AICD assays, 3 distinct cellular models of CTL-induced cell kill. Further, provision of ceramide, the product of ASMase action, to target cells genetically deficient in ASMase restored CTL-induced platform formation and cell killing. That formation of ceramide-rich platforms represents a biologically relevant phenomenon is denoted by marked reduction in multiple aspects of the pathophysiologic response in standardized GVHD models with MHC and minor histocompatability antigen disparity when target allotransplantation recipients are genetically defective in initiating this program.
In the initiation phase of acute GVHD, conditioning damage to the intestines coupled to donor CTL attack of host tissue propagate a proinflammatory state characterized by a “cytokine storm” required for donor CTL expansion. In asmase−/− recipients of allogeneic BM and T cells, an attenuated cytokine response is observed, as well as significant reduction in donor CTL expansion. We have published that one type of GI tract damage after single high doses of radiation requires a wave of ASMase-dependent endothelial cell apoptosis coupling vascular insufficiency to stem cell damage.22 As the threshold for endothelial cell apoptosis is approximately 10 Gy, well above the 5.5 Gy used in our preconditioning regimen of 1100 cGy delivered as a split dose, we were not surprised to find lack of statistical difference in preconditioning-induced GI tract damage between asmase+/+ and asmase−/− mice (Figure 2A). We think, based on these data, that attenuated cytokine expression and CTL expansion response in ASMase knockout animals cannot be attributed to differences in conditioning injury. Our data demonstrating similar killing capacity of alloactivated T cells harvested from asmase−/− recipients as asmase+/+ recipients, and the normal proliferative response of T cells coincubated with asmase−/− splenocytes, suggest that antigen presentation and recognition were not decreased in asmase−/− hosts. Indeed, the only phenotypic defect we find mechanistically consistent with the observed resistance to GVHD was that displayed by asmase−/− target cells (hepatocytes) in initiating ceramide-mediated death. Thus, we attribute attenuated cytokine storm to indicate early donor T cell–mediated tissue damage, which propagates inflammation,3 is diminished in the absence of target cell asmase−/−. Further, as cytokine elevation feed-forwards CTL expansion, we hypothesize this as the mechanism for reduced CD8+ clonal expansion in the asmase−/− background.
Multiple groups previously identified generation of ceramide-rich platforms as critical to Fas-mediated death signaling, yet this concept is currently far from consensus, as some studies have failed to recognize platform formation45,46 and others have questioned the relevance of ceramide to Fas activation.47 Algeciras-Schimnich et al45 did not detect Fas-containing platforms in SKW.4, K50, or H9 lymphoid cells lines. This probably resulted from failure to protect Fc receptors while using agonistic anti-Fas Apo-1-3 antibody, resulting in their nonspecific clustering and the masking of specific Fas clustering within platforms.27 Further, although Muppidi and Siegel46 detected constitutive Fas localization in gycosphingolipid-enriched microdomains (GEMs) of cells displaying type 1 apoptosis, they failed to detect Fas translocation into GEMs in cells engaging a type 2 response. Revisiting these studies in our laboratory using the same reagents revealed excessive detergent use may have selectively extracted Fas from ceramide-rich platforms during biophysical isolation in type 2 cells (supplemental Figure 8). It is well recognized that resident GEM proteins are more tightly bound to GEMs and less easily extracted than proteins that traffic in and out of GEMs.48
Whereas the current studies are the first to address the role of ceramide-rich platforms in tissue sensitivity to T cell–mediated cytotoxicity, previous data suggested that ceramide itself might play a role in T-cell immunity. During phytohemagglutin-induced hepatitis, a model for acute T cell–mediated autoreactive liver disorder,18 FasL up-regulation is induced on lymphocytes and on their migration to the liver, hepatocytes are killed by apoptosis, prompting hepatitis.49 ASMase deficiency rendered hepatocytes resistant to apoptosis despite normal up-regulation of lymphocyte FasL.18 Similarly, CD4 activation by the HIV receptor molecule gp120, or by an agonistic anti-CD4 antibody, activates the Fas/FasL system and initiates apoptosis, whereas CD4+ T cells deficient in ASMase normally up-regulated Fas/FasL but were resistant to apoptosis.18 Furthermore, asmase−/− CD8+ T cells were recently shown defective in cytolytic granule exocytosis, delaying lymphocytic choriomeningitis virus elimination.50 Thus, ceramide may contribute to both effector arms of CTL signaling, required for target cell response to TNF superfamily ligands and for release of cytolytic granules by effector CTLs.
The current investigation identifies multiple events during the early (donor T-cell proliferation, serum cytokine expansion) and late (target organ damage, tissue apoptosis, morbidity, and mortality) phases of acute GVHD impacted by inactivation of ASMase-mediated ceramide generation. These studies thus provide several previously unrecognized membrane-based signaling targets for therapy. Whether ceramide signaling can be leveraged pharmacologically is currently uncertain, as only limited effort has been applied to development of pharmacologic tools. Further, the benefit of inactivation of ceramide-rich platforms may not be restricted to Fas-mediated pathophysiology as evidence indicates that other inflammatory cytokines, including TNF, IL-1, CD40, and TNF-related apoptosis-inducing ligand, may similarly use ASMase for transmembrane signal transmission. ASMase-generated ceramide-rich platforms may thus represent a promiscuous target for GVHD and other T cell–mediated immune disorders, and hence may warrant further investigation.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Adam Kochman, Vanessa Hubbard, Uttam Rao, and Nury Yim for their technical assistance in these studies.
This work was supported by the National Institutes of Health (grant CA52462 to Z.F.; grant CA85704 to R.K.; grants HL69929, CA33049, and CA107096 to M.R.v.d.B.) and by awards from the Leukemia & Lymphoma Society, the Ryan Gibson Foundation, the Emerald Foundation, the Experimental Therapeutics Center of Memorial Sloan-Kettering Cancer Center funded by Mr William H. Goodwin and Mrs Alice Goodwin, and the Commonwealth Foundation for Cancer Research (M.R.v.d.B.).
National Institutes of Health
Authorship
Contribution: J.A.R. designed experiments, collected and analyzed data, and wrote the paper; B.S., J.Z., D.S., C.G.K., L.W.K., and S.X.L. collected data; G.F.M., C.L., and S.X.L. analyzed data; and Z.F., M.R.v.d.B., and R.K. designed experiments and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Richard Kolesnick, Laboratory of Signal Transduction, Memorial Sloan-Kettering Cancer Center, 1275 York Ave, New York, NY 10065; e-mail: r-kolesnick@ski.mskcc.org.