Abstract
The PD-1/PD-L1 pathway plays an important role in regulation of alloimmune responses and in induction and maintenance of peripheral tolerance. Because GVHD is driven by donor T cells and PD-L1 expression can be markedly elevated on T cells during activation, we investigated the functional significance of PD-L1 expressed by donor T cells in regulating murine models of acute GVHD.
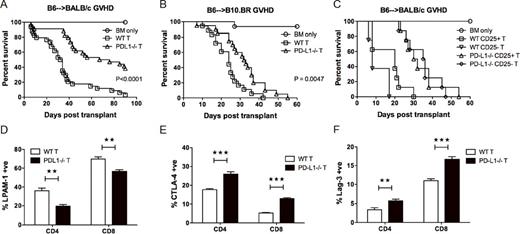
PD-L1 expression was up-regulated on donor CD4 and CD8 T cells during GVHD. We considered the possibility that PD-L1 expression on activated donor T cells might inhibit GVHD by down regulating donor anti-host T cell responses, consistent with PD-L1 co-inhibitory activity when expressed on host parenchymal cells during GVHD. Surprisingly, T cell mediated GVHD lethality was markedly reduced in recipients of PD-L1-/- compared to WT donor T cells in both B6 to BALB/c model of GVHD(P<0.0001; Fig 1A) and in B6 to B10.BR model (P=0.0047; Fig 1B), suggesting that PD-L1 expression on donor T cells is involved in interactions that enhance T cell mediated effector function. Survival data confirmed that PD-L1-/- Teffs and not Tregs were responsible for reduced lethality in recipients of PD-L1-/- donor T cells (Fig 1C). During GVHD, PD-L1-/- donor CD4 and CD8 T cells had reduced expression of gut homing receptors (Fig 1D), and recipients of PD-L1-/- donor T cells had reduced T cell infiltration into lymphoid organs and gut, retained intestinal epithelial integrity, and had lower inflammatory cytokine production. PD-L1-/- donor CD4 and CD8 T cells had increased expression of multiple inhibitory receptors (Fig 1E, 1F), reduced T cell proliferation, and increased T cell apoptosis by transcriptional profiling and cell surface marker expression. Four pathways, including proteasome activity showed decreased expression in PD-L1-/- donor T cells. In vitro T cell activation in the presence of single (PD-L1:B7-1) vs. dual (PD-L1:B7-1 and PD-L1:PD-1) pathway blocking anti-PD-L1 mAb confirmed that T-T interaction between PD-1 and PD-L1 is important for proliferation and survival, whereas sensitive in vitro assays with supported lipid bilayers found no evidence for a functionally relevant cis interaction of PD-L1 and PD-1 on T cells. We found a significant increase in glucose transporter (GLUT1) expression in proliferating WT vs. PD-L1-/- donor CD4 and CD8 T cells, along with increased glycolysis, OXPHOS, glutamine consumption and glutamate production. We also observed increased fatty acid (FA) uptake and FA oxidation, and enhanced pharmacologic inhibition of FA oxidation in WT donor T cells, suggesting that PD-1:PD-L1 interactions are important for FA metabolism, which may further support T cell survival. Studies using stable isotope carbon tracers highlighted the divergent roles for glutamine and glucose in energy generation and biosynthetic pathways. Given the importance of acetyl-CoA as a high energy thioester intermediate in the TCA cycle and a lipogenic precursor for T cells undergoing expansion, significantly enhanced production of acetyl-CoA from glucose by WT donor T cells support the notion that PD-L1 on T cells promotes clonal expansion of alloreactive T cells. In summary, these data are the first to show that PD-L1 expression on donor T cells can provide positive signals for T cell survival, activation, and metabolism. Greater understanding of the function of PD-L1 expression by activated donor T cells will provide new insight into the regulation of GVHD and suggest strategies to selectively inhibit PD-L1 on donor T cells that may be clinically useful to prevent GVHD.
PD-L1-/- vs. WT donor T cells lessen GVHD lethality, independent of donor Treg function. (A) Survival of BALB/c mice with WT B6 or PD-L1-/- T cells. (B) Survival of B10.BR mice with WT B6 or PD-L1-/- T cells. (C) Survival of BALB/c mice with WT B6 or PD-L1-/- T cells, or with WT B6 or PD-L1-/- CD25 depleted T cells (recipients of WT T cells vs. WT CD25-depleted T cells, P = 0.0003; recipients of PD-L1-/- T cells vs. PD-L1-/- CD25-depleted T cells, P = 0.2306; recipients of WT vs. PD-L1-/- T cells, P < 0.0001). (D) BALB/c mice transplanted with WT B6 or PD-L1-/- T cells. Mice were killed on d7 post-BMT and splenocytes were analyzed for LPAM-1, CCR9, and CXCR3 expression (not shown) on donor T cells. (E-F) BALB/c mice were transplanted with B6 Ly5.2 T cells plus PD-L1-/- T cells. Mice were killed on d3 post-BMT and splenocytes were analyzed for CTLA-4 and Lag-3 expression on donor T cells.
PD-L1-/- vs. WT donor T cells lessen GVHD lethality, independent of donor Treg function. (A) Survival of BALB/c mice with WT B6 or PD-L1-/- T cells. (B) Survival of B10.BR mice with WT B6 or PD-L1-/- T cells. (C) Survival of BALB/c mice with WT B6 or PD-L1-/- T cells, or with WT B6 or PD-L1-/- CD25 depleted T cells (recipients of WT T cells vs. WT CD25-depleted T cells, P = 0.0003; recipients of PD-L1-/- T cells vs. PD-L1-/- CD25-depleted T cells, P = 0.2306; recipients of WT vs. PD-L1-/- T cells, P < 0.0001). (D) BALB/c mice transplanted with WT B6 or PD-L1-/- T cells. Mice were killed on d7 post-BMT and splenocytes were analyzed for LPAM-1, CCR9, and CXCR3 expression (not shown) on donor T cells. (E-F) BALB/c mice were transplanted with B6 Ly5.2 T cells plus PD-L1-/- T cells. Mice were killed on d3 post-BMT and splenocytes were analyzed for CTLA-4 and Lag-3 expression on donor T cells.
Aoyama:CHUGAI PHAMACEUTICAL CO.,LTD: Honoraria; Mochida Pharmaceutical Co.,Ltd: Honoraria; Kyowa Hakko Kirin Company,Limited: Honoraria. Milone:Novartis: Patents & Royalties, Research Funding. Miller:Coronado: Speakers Bureau; BioSciences: Speakers Bureau; Celegene: Speakers Bureau. Sharpe:Costim Pharmaceuticals: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal