Issue Archive
Table of Contents
EDITORIAL
Introduction to a review series on acute lymphoblastic leukemia
Our understanding of the biology of acute lymphoblastic leukemia (ALL) continues to be refined, and these advances naturally lead to improvements in therapy and outcomes for pediatric and adult patients. Associate Editor Hervé Dombret introduces this series of reviews that bring readers up to date with the biology of both B-cell and T-cell ALL (B-ALL and T-ALL) as well as the latest approaches to first-line therapy. Passet et al discuss the different genetic subtypes of B-ALL and their implications, while Pölönen and colleagues discuss T-ALL, highlighting how biology informs classification and in turn prognostication and therapy. Badar and coauthors explore how the incorporation of immunotherapy is revolutionizing treatment regimens. Finally, Rampotas and Roddie focus specifically on the role of chimeric antigen receptor T cells in management of patients with B-ALL now and in the future.
BLOOD COMMENTARIES
REVIEW SERIES
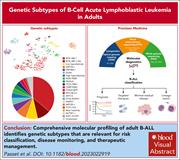
Genetic subtypes of B-cell acute lymphoblastic leukemia in adults
Our understanding of the biology of acute lymphoblastic leukemia (ALL) continues to be refined, and these advances naturally lead to improvements in therapy and outcomes for pediatric and adult patients. Associate Editor Hervé Dombret introduces this series of reviews that bring readers up to date with the biology of both B-cell and T-cell ALL (B-ALL and T-ALL) as well as the latest approaches to first-line therapy. Passet et al discuss the different genetic subtypes of B-ALL and their implications, while Pölönen and colleagues discuss T-ALL, highlighting how biology informs classification and in turn prognostication and therapy. Badar and coauthors explore how the incorporation of immunotherapy is revolutionizing treatment regimens. Finally, Rampotas and Roddie focus specifically on the role of chimeric antigen receptor T cells in management of patients with B-ALL now and in the future.
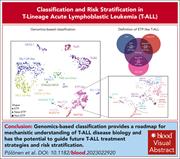
Classification and risk stratification in T-lineage acute lymphoblastic leukemia
Our understanding of the biology of acute lymphoblastic leukemia (ALL) continues to be refined, and these advances naturally lead to improvements in therapy and outcomes for pediatric and adult patients. Associate Editor Hervé Dombret introduces this series of reviews that bring readers up to date with the biology of both B-cell and T-cell ALL (B-ALL and T-ALL) as well as the latest approaches to first-line therapy. Passet et al discuss the different genetic subtypes of B-ALL and their implications, while Pölönen and colleagues discuss T-ALL, highlighting how biology informs classification and in turn prognostication and therapy. Badar and coauthors explore how the incorporation of immunotherapy is revolutionizing treatment regimens. Finally, Rampotas and Roddie focus specifically on the role of chimeric antigen receptor T cells in management of patients with B-ALL now and in the future.
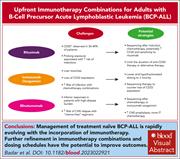
Incorporation of immunotherapy into frontline treatment for adults with B-cell precursor acute lymphoblastic leukemia
Our understanding of the biology of acute lymphoblastic leukemia (ALL) continues to be refined, and these advances naturally lead to improvements in therapy and outcomes for pediatric and adult patients. Associate Editor Hervé Dombret introduces this series of reviews that bring readers up to date with the biology of both B-cell and T-cell ALL (B-ALL and T-ALL) as well as the latest approaches to first-line therapy. Passet et al discuss the different genetic subtypes of B-ALL and their implications, while Pölönen and colleagues discuss T-ALL, highlighting how biology informs classification and in turn prognostication and therapy. Badar and coauthors explore how the incorporation of immunotherapy is revolutionizing treatment regimens. Finally, Rampotas and Roddie focus specifically on the role of chimeric antigen receptor T cells in management of patients with B-ALL now and in the future.
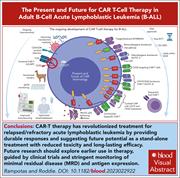
The present and future of CAR T-cell therapy for adult B-cell ALL
Our understanding of the biology of acute lymphoblastic leukemia (ALL) continues to be refined, and these advances naturally lead to improvements in therapy and outcomes for pediatric and adult patients. Associate Editor Hervé Dombret introduces this series of reviews that bring readers up to date with the biology of both B-cell and T-cell ALL (B-ALL and T-ALL) as well as the latest approaches to first-line therapy. Passet et al discuss the different genetic subtypes of B-ALL and their implications, while Pölönen and colleagues discuss T-ALL, highlighting how biology informs classification and in turn prognostication and therapy. Badar and coauthors explore how the incorporation of immunotherapy is revolutionizing treatment regimens. Finally, Rampotas and Roddie focus specifically on the role of chimeric antigen receptor T cells in management of patients with B-ALL now and in the future.
CLINICAL TRIALS AND OBSERVATIONS
Odronextamab monotherapy in R/R DLBCL after progression with CAR T-cell therapy: primary analysis of the ELM-1 study
Clinical Trials & Observations
The outcomes for patients with diffuse large B-cell lymphoma (DLBCL) who have progressive disease after chimeric antigen receptor (CAR) T-cell therapy are dismal. Topp et al showed that in a 60-patient cohort in an early-phase trial, odronextamab, a CD20×CD3 bispecific antibody, is a promising treatment for such patients, with one-third of all patients achieving complete response and one-fourth showing no progression after 1 year. Correlative studies indicate that T-cell fitness is preserved in many patients, suggesting that these clinical results, once confirmed, may lead to durable remissions for patients who fail CAR T-cell therapy.
HEMATOPOIESIS AND STEM CELLS
Progressive chromatin rewiring by ETO2::GLIS2 revealed in a genome-edited human iPSC model of pediatric leukemia initiation
The ETO2::GLIS2 fusion drives almost 20% of pediatric non–Down syndrome acute megakaryoblastic leukemia cases and is associated with a particularly poor outcome. Boudia and colleagues report a human induced pluripotent stem cell (iPSC) model of the disease, recapitulating the human disease and enabling a comprehensive molecular investigation. The authors identified osteogenic homeobox factor DLX3 as a critical player in the onset of leukemia and provide a system that could underpin future drug screening to generate novel treatment strategies.
IMMUNOBIOLOGY AND IMMUNOTHERAPY
A phase 1 trial of prizloncabtagene autoleucel, a CD19/CD20 CAR T-cell therapy for relapsed/refractory B-cell non-Hodgkin lymphoma
Clinical Trials & Observations
Despite the curative potential of anti-CD19 chimeric antigen receptor (CAR) T-cell therapy in relapsed B-cell lymphomas, treatment failure remains common, often due to loss of CD19 expression by the malignant cells. In a phase 1 study, Yu and colleagues describe a strategy to circumvent treatment failure through prizloncabtagene autoleucel, a dual targeting CAR T-cell therapy which targets both CD20 and CD19. The authors report that this bispecific product induced complete responses in 85% of patients, with a median duration of response exceeding 2 years, and a toxicity profile expected for this class of therapy.
LYMPHOID NEOPLASIA
Dissection of single-cell landscapes for the development of chimeric antigen receptor T cells in Hodgkin lymphoma
A small subset of patients with classic Hodgkin lymphoma (cHL) experience recurrent or progressive disease despite current chemotherapy- and immunotherapy-based therapies, highlighting a significant unmet need. Gottschlich and colleagues identified CD86 as a novel immunotherapeutic target in cHL and explored CD86–CTLA-4 cross talk between malignant cells and T cells in the tumor microenvironment. Based on these findings, the authors describe a CD86-28z chimeric antigen receptor T-cell approach with promising preclinical in vivo efficacy that warrants further investigation.
MYELOID NEOPLASIA
CD44-mediated metabolic rewiring is a targetable dependency of IDH-mutant leukemia
PLATELETS AND THROMBOPOIESIS
Aging platelets shift their hemostatic properties to inflammatory functions
Although anucleate, platelets are highly dynamic cells with the capacity to recognize different ligands, leading to their activation and involvement in processes beyond hemostasis. Anjum and colleagues reveal that, in both mice and humans, aging platelets have lesser procoagulant function but increase their capacity to interact with leukocytes and bacteria and that their transfusion enhances inflammatory responses in vivo. This shift in functional profile from hemostatic to inflammatory as platelets age has future implications for optimization of platelet transfusion preparation and storage.
LETTER TO BLOOD
BLOOD WORK
-
Cover Image
Cover Image
![issue cover]()
Lung histology image depicting recruitment of 96- to 108-hour-old platelets in a murine acute lung injury model. Pulse labeling showed that this age cohort of platelets was more likely to be recruited in inflammatory settings. See the article by Anjum et al on page 1568.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals






Two strikes, base hit: odronextamab after CAR T cells in LBCL
Clinical Trials & Observations